- Department of Orthopedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
- Department of Neurosurgery, Ibn Sina Diagnostic and Consultation Centre, Dhaka, Bangladesh.
- Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Correspondence Address:
Nazmin Ahmed
Department of Orthopedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
DOI:10.25259/SNI_579_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shahidul Islam Khan1, Nazmin Ahmed2, Bipin Chaurasia3, Kamrul Ahsan1. Diagnosis and treatment of noncommunicating extradural spinal thoracolumbar arachnoid cyst. 25-Nov-2020;11:405
How to cite this URL: Shahidul Islam Khan1, Nazmin Ahmed2, Bipin Chaurasia3, Kamrul Ahsan1. Diagnosis and treatment of noncommunicating extradural spinal thoracolumbar arachnoid cyst. 25-Nov-2020;11:405. Available from: https://surgicalneurologyint.com/surgicalint-articles/10410/
Abstract
Background: Noncommunicating extradural spinal arachnoid cysts are extremely rare. They are believed to arise from congenital defects in the dura mater and become enlarged as a consequence of increased cerebro-spinal fluid (CSF) pressure within the subarachnoid space. Most retain a communicating pedicle through which the extradural cyst maintains connection with the subarachnoid space, and only rarely does this communication become sealed. The optimal treatment consists of complete surgical removal of the cyst with ligation of the communicating pedicle.
Case Description: A 29-year-old male presented with a progressive spastic paraparesis of 6 months’ duration. The MRI showed a circumscribed intradural extramedullary cystic lesion located from D11-L2. Notably, peroperatively, the cyst appeared to be entirely extradural, without a communicating intradural pedicle. Further, no CSF leak was observed even after Valsalva maneuvers. Following surgical extirpation of the cyst, the patient sustained an uneventful recovery within 1 postoperative month.
Conclusion: Noncommunicating extradural arachnoid cysts are extremely rare causes of spinal cord compression and should be fully excised.
Keywords: Cerebro-spinal fluid, Noncommunicating extradural spinal arachnoid cyst
INTRODUCTION
Noncommunicating spinal extradural arachnoid cysts are extremely rare contributors to spinal cord compression and most typically involve thoracic spine (65%).[
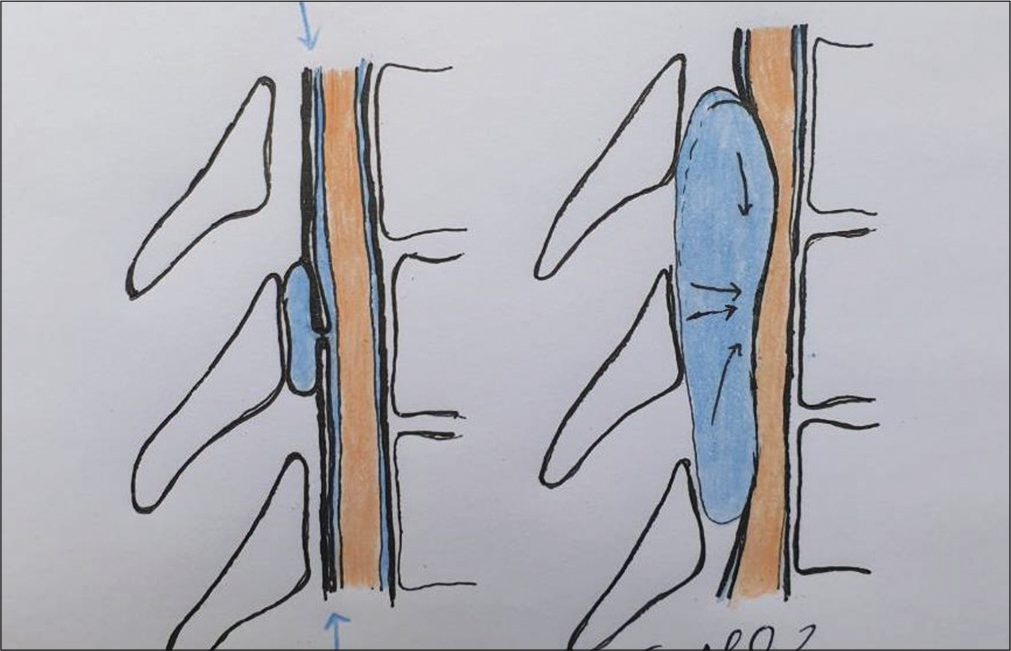
Figure 1:
Schematic picture demonstrated the natural history and pathogenesis of the spinal arachnoid cyst. A small extradural arachnoid pouch with a communicating pedicle is illustrated. Progressive expansion of the cyst occur as a consequence of raised CSF pressure within the spinal subarachnoid space (drawn by blue arrowhead); the cyst wall tension is greater enough to seal the communication (drawn by black arrowhead).
CASE REPORT
History and physical examination
A 29-year-old male patient presented with 6 months’ duration of a progressive paraparesis (4/5) accompanied by a partial T8 sensory level, but with intact sphincter function.
Neuroimaging findings
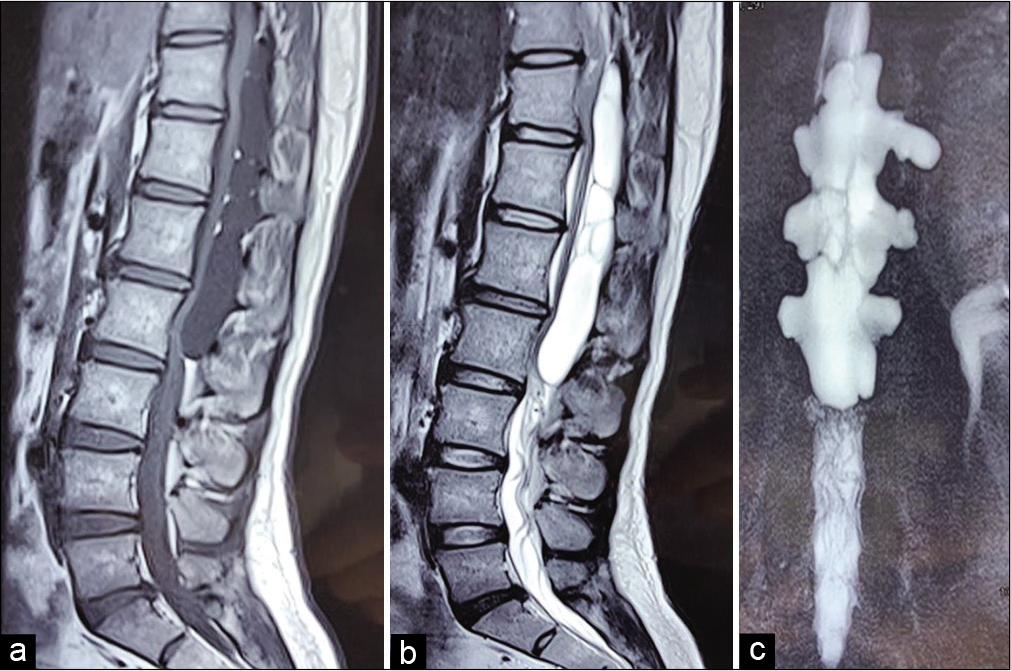
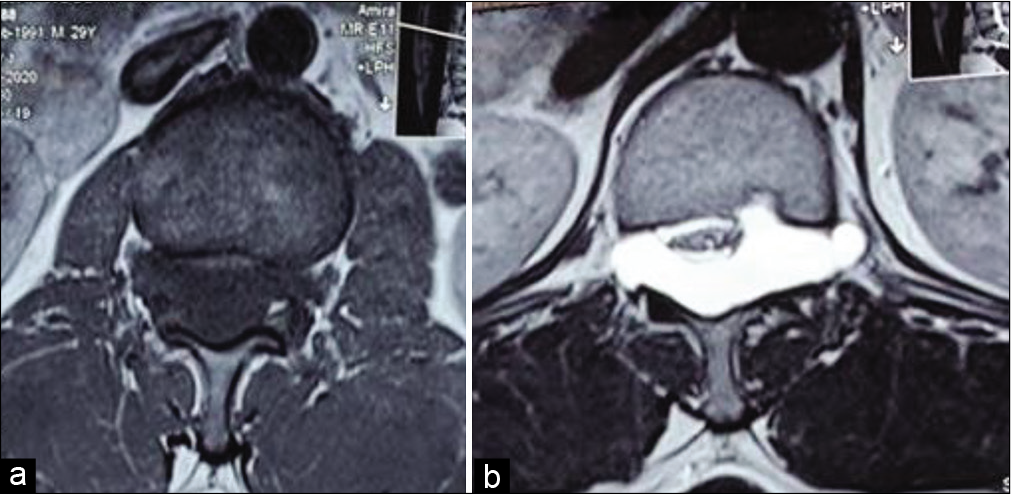
The thoracic MR revealed a well-defined, nonenhancing intradural extramedullary cystic lesion in the spinal canal measuring 8 cm × 3.2 cm extending from D11 to L2. It was hypointense on T1 and hyperintense on T2WI studies and contained internal septations. The lesion significantly compressed the spinal cord, conus, and cauda equina [
Figure 2:
MRI of the dorsolumbar region sagittal section, T1WI (a) and T2WI (b), demonstrates a large intradural extramedullary cystic lesion with multiple internal septations, having significant compression over spinal cord, conus medullaries, and cauda equine. MR myelogram (c) showing variable extension into bilateral neural foramen.
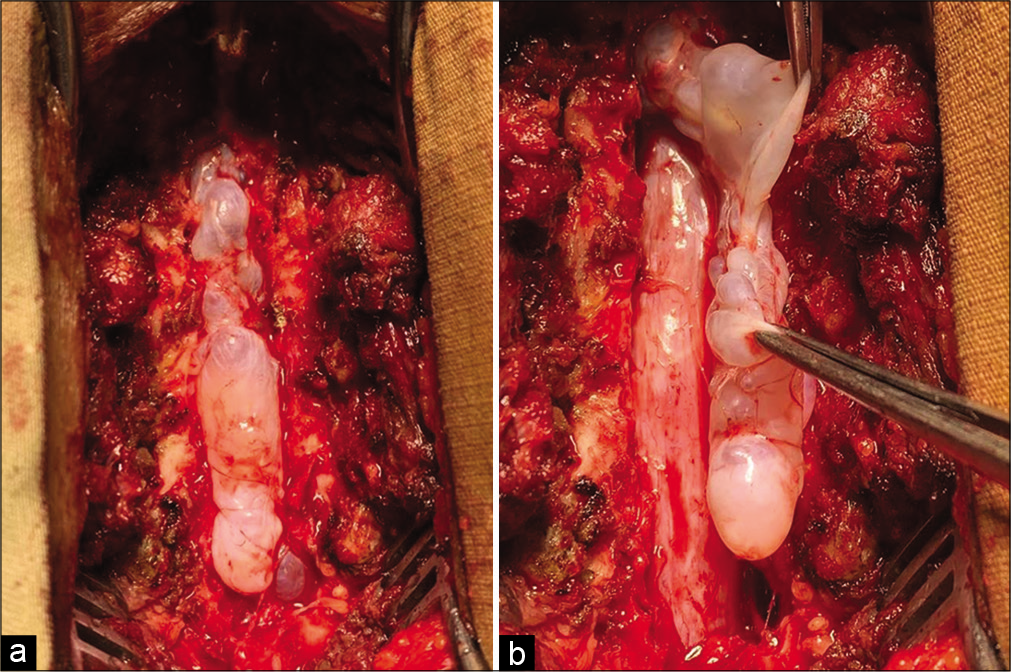
Surgery: A laminectomy was performed from D11 to L2. Once the large extradural spinal arachnoid cyst was exposed, a plane was easily developed between the cyst and thecal sac allowing for complete en bloc cyst removal [
DISCUSSION
Noncommunicating spinal extradural arachnoid cysts are extremely rare. The pathophysiology of cyst enlargement can be explained by either the active fluid secretion theory or pulsatile CSF dynamic theory.[
They have been classified into three categories: extradural cysts without spinal nerve root fibers (Type I), subdivided into extradural arachnoid cysts (Type IA), sacral meningoceles (Type IB), extradural cysts with spinal nerve root fibers (Type II), and intradural cysts (Type III).[
Clinical presentation
These cysts are usually seen in adolescents, whereas dorsolumbar and lumbar cysts usually appear in adults. Single cysts can extend over several spinal segments in craniocaudal direction, and may be accompanied by multiple, separate dural defects/communicating pedicles.[
Diagnostic studies of choice for spinal arachnoid cysts
MR is the diagnostic study of choice because as it best defines the type and extent of the cyst, and relationship to surrounding neurovascular structures. For demonstrating the communication with the subarachnoid space, the optimal examination is the CT myelogram.[
CONCLUSION
Noncommunicating extradural thoracic spinal arachnoid cysts rarely contribute to spinal cord compression as shown in the case presented. The treatment of choice is routine gross total resection utilizing a decompressive laminectomy alone, with only select cases warranting consideration of fusion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are grateful to Dr. Nazmin Ahmed for the wonderful color illustrations.
References
1. Eroglu U, Bozkurt M, Kahilogullari G, Dogan I, Ozgural O, Shah KJ. Surgical management of spinal arachnoid cysts in adults. World Neurosurg. 2019. 122: e1146-52
2. Ido K, Matsuoka H, Urushidani H. Effectiveness of a transforaminal surgical procedure for spinal extradural arachnoid cyst in the upper lumbar spine. J Clin Neurosci. 2002. 9: 694-6
3. Khosla A, Wippold FJ. CT myelography and MR imaging of extramedullary cysts of the spinal canal in adult and pediatric patients. AJR Am J Roentgenol. 2002. 178: 201-7
4. Kim IS, Hong JT, Son BC, Lee SW. Noncommunicating spinal extradural meningeal cyst in thoracolumbar spine. J Korean Neurosurg Soc. 2010. 48: 534-7
5. Kojimahara Y, Tsuge S, Hasegawa K, Fukutake K, Nakamura K, Wada A. A case of a spinal extradural arachnoid cyst. Case Rep Orthop. 2019. 2019: 3516598
6. Kulkarni AG, Goel A, Thiruppathy SP, Desai K. Extradural arachnoid cysts: A study of seven cases. Br J Neurosurg. 2004. 18: 484-8
7. Liu JK, Cole CD, Sherr GT, Kestle JR, Walker ML. Noncommunicating spinal extradural arachnoid cyst causing spinal cord compression in a child. J Neurosurg. 2005. 103: 266-9
8. Sonawane DV, Garg BK, Dave H, Nangare V, Chandanwale A. Multiple spinal extradural arachnoid cyst: A case report. Int J Spine. 2019. 4: 27-30