- Norton Neuroscience Institute, Norton Healthcare, Louisville, Kentucky, United States.
- Neurodiagnostic Center of Louisville, Louisville, Kentucky, United States.
- Norton Vascular Surgery, Norton Healthcare, Louisville, Kentucky, United States.
- Department of Neurological Surgery, University of Louisville School of Medicine, Louisville, Kentucky, United States.
Correspondence Address:
Christopher B. Shields
Norton Neuroscience Institute, Norton Healthcare, Louisville, Kentucky, United States.
Department of Neurological Surgery, University of Louisville School of Medicine, Louisville, Kentucky, United States.
DOI:10.25259/SNI_33_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lisa B. E. Shields1, Vasudeva G. Iyer2, Stephen B. Self3, Yi Ping Zhang1, Christopher B. Shields1,4. Differentiation of vascular claudication due to bilateral common iliac artery stenosis versus neurogenic claudication with spinal stenosis. 17-May-2021;12:231
How to cite this URL: Lisa B. E. Shields1, Vasudeva G. Iyer2, Stephen B. Self3, Yi Ping Zhang1, Christopher B. Shields1,4. Differentiation of vascular claudication due to bilateral common iliac artery stenosis versus neurogenic claudication with spinal stenosis. 17-May-2021;12:231. Available from: https://surgicalneurologyint.com/surgicalint-articles/10808/
Abstract
Background: Differentiating between neurogenic and vascular claudication may be difficult. Vascular claudication due to aortic and iliac artery occlusions may present as low back, hip, and buttock pain while walking short distances. These findings are often very similar to those seen for neurogenic claudication attributed to lumbar stenosis.
Case Description: A 68-year-old female presented with low back, right hip, and groin pain while walking short distances. She had previously undergone lumbar and cardiac surgery. Now, with negative repeated lumbar studies, the CT angiogram (CTA) revealed a dense calcified plaque in the right common iliac artery resulting in 90% stenosis at its origin and
Conclusion: Spine surgeons should be aware that vascular and neurogenic claudication may mimic each other. Obtaining MR studies of the lumbar spine and EMG/NCV, along with the appropriate vascular studies (CTAs), help differentiate between the two, and result in the appropriate operative choices.
Keywords: Claudication, Electromyography/nerve conduction study, Hip, Neurogenic, Vascular
INTRODUCTION
While a spinal MRI/CT is the preferred modality for detecting lumbar stenosis, CT angiogram (CTA) and ankle–brachial index (ABI) studies are the gold standards for confirming aortoiliac occlusive disease (i.e., peripheral arterial disease).[
Here, we report a 68-year-old female who presented with “claudication.” When MR studies documented resolved lumbar stenosis, the abdominal/pelvic CTA documented significant bilateral iliac artery occlusive disease. Here, we presented a case of vascular claudication and reviewed the various factors that separate vascular and neurogenic claudication.
CASE PRESENTATION
History and radiological imaging
A 68-year-old female (body mass index 34.75 kg/m2), with a history of hypertension, hyperlipidemia, diabetes mellitus, prior smoking, and a myocardial infarction (status post 1-vessel coronary artery bypass graft), presented with a 5-year history of low back pain/right hip/groin pain and numbness of the anterior aspect of the right thigh. When the lumbar myelogram/myelo-CT documented L4-5 stenosis with Grade I spondylolisthesis, the patient underwent a L4-5 lumbar decompression/fusion. When she failed to improve, she underwent a negative exploratory arthroscopy of the right hip. She underwent an abdominal aortoiliac CTA which documented marked aortoiliac calcification.
Now, the patient presented with a normal neurological examination, except for loss of pinprick sensation over the anterior thighs bilaterally. However, the vascular examination of the lower extremities revealed an absent right-sided posterior tibial pulse and loss of bilateral dorsalis pedis pulses.
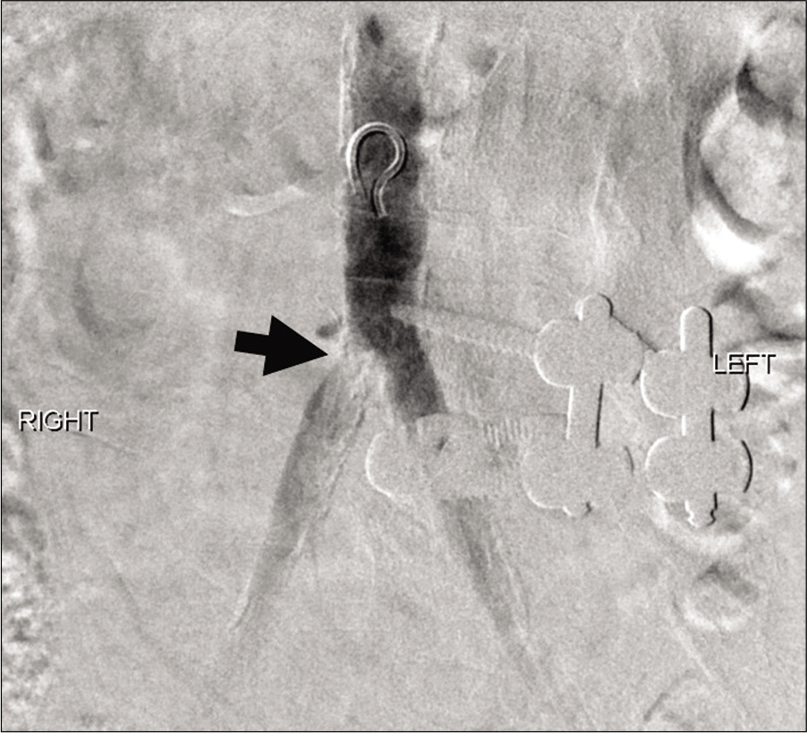
On the CTA and abdominal subtraction arteriogram, there was diffuse atherosclerotic disease and moderate to high-grade stenosis involving the right common iliac artery near its origin [
Vascular surgery
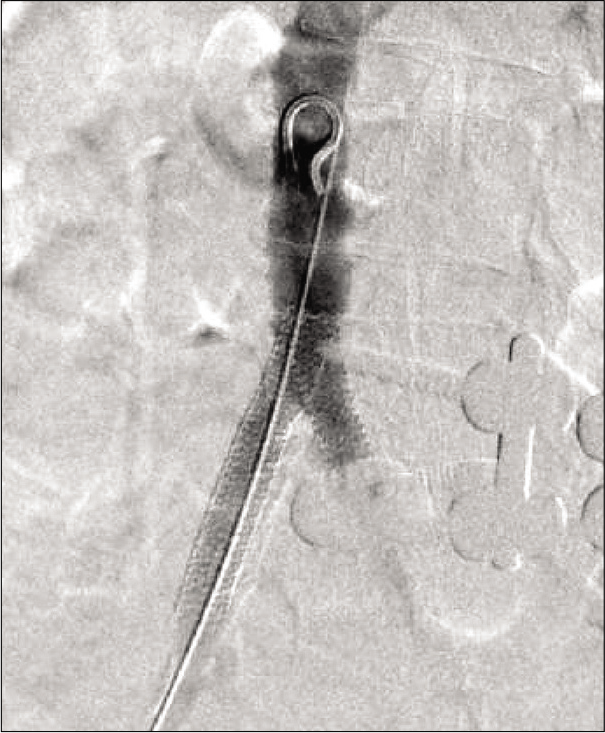
When the abdominal aortoiliac CTA confirmed severe bilateral aortoiliac calcification, she underwent appropriate bilateral endovascular stenting procedures. An 8.0 mm × 57.0 mm ExpressTM LD stent (Boston Scientific; Marlborough, MA) was placed on the right, and an 8.0 mm × 37.0 mm ExpressTM LD stent was placed on the left. These kissing stents extended from the distal aorta into the common iliac arteries bilaterally and were deployed simultaneously by inflating the delivery balloon to 10 atmospheres. Following stent placement, the common iliac arteries were widely patent with no significant residual stenosis noted on the intraoperative arteriogram [
Postoperative follow-up
Postoperatively, the patient’s right hip and buttock pain completely resolved within 1 week of stent placement. She was asymptomatic while walking a mile. The right lower extremity demonstrated mild arterial insufficiency at rest with an ABI of 0.89 and digit pressure of 91 mm Hg 1 week postoperatively.
DISCUSSION
Differentiation of neurogenic claudication versus vascular claudication
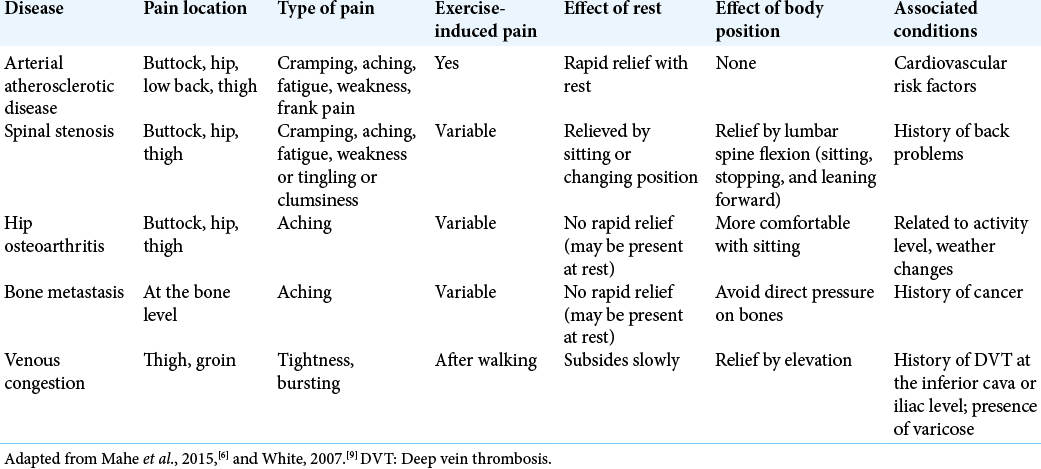
Spine surgeons often neglect to perform a vascular examination (abdominal CTA), especially when the symptoms are not typical for spinal stenosis and spinal imaging studies fail to demonstrate truly “significant” findings for lumbar stenosis. The diagnosis of vascular claudication due to arterial atherosclerotic disease, particularly at the L2-3 level, and/or hip joint disease is presented in [
Endovascular procedures for vascular claudication
Aortoiliac CTA is now the procedure of choice to define aortoiliac disease that is now largely treated with endovascular procedures (e.g., percutaneous transluminal angioplasty with or without stent placement); they have high success rates without major complications.[
CONCLUSION
It may be difficult for spine surgeons to differentiate between lumbar neurogenic claudication and peripheral vascular claudication. Whereas MR studies best document lumbar stenosis, abdominal/pelvic CTAs readily demonstrate aortoiliac disease.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
1. Burke CR, Henke PK, Hernandez R, Rectenwald JE, Krishnamurthy V, Englesbe MJ. A contemporary comparison of aortofemoral bypass and aortoiliac stenting in the treatment of aortoiliac occlusive disease. Ann Vasc Surg. 2010. 24: 4-13
2. DeWolfe VG, Lefevre FA, Humphries AW, Shaw MB, Phalen GS. Intermittent claudication of the hip and the syndrome of chronic aorto-iliac thrombosis. Circulation. 1954. 9: 1-16
3. Haig AJ, Park P, Henke PK, Yamakawa KS, Tomkins-Lane C, Valdivia J. Reliability of the clinical examination in the diagnosis of neurogenic versus vascular claudication. Spine J. 2013. 13: 1826-34
4. Jeon CH, Han SH, Chung NS, Hyun HS. The validity of ankle-brachial index for the differential diagnosis of peripheral arterial disease and lumbar spinal stenosis in patients with atypical claudication. Eur Spine J. 2012. 21: 1165-70
5. Johansson JE, Barrington TW, Ameli M. Combined vascular and neurogenic claudication. Spine (Phila Pa 1976). 1982. 7: 150-8
6. Mahe G, Kaladji A, Le FA, Jaquinandi V. Internal iliac artery stenosis: Diagnosis and how to manage it in 2015. Front Cardiovasc Med. 2015. 2: 33
7. Moon JY, Hwang HP, Kwak HS, Han YM, Yu HC. The results of self-expandable kissing stents in aortic bifurcation. Vasc Specialist Int. 2015. 31: 15-9
8. Prince JF, Smits ML, van Herwaarden JA, Arntz MJ, Vonken EJ, van den Bosch MA. Endovascular treatment of internal iliac artery stenosis in patients with buttock claudication. PLoS One. 2013. 8: e73331
9. White C. Clinical practice. Intermittent claudication. N Engl J Med. 2007. 356: 1241-50