- Department of Neurosurgery, Nara Medical University, Shijo-Cho, Kashihara, Nara, Japan.
DOI:10.25259/SNI_280_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daisuke Wajima, Fumihiko Nishimura, Katsuya Masui. Diffuse large B-cell lymphoma in the sphenoid sinus: A case report and review of literature. 25-Jul-2020;11:208
How to cite this URL: Daisuke Wajima, Fumihiko Nishimura, Katsuya Masui. Diffuse large B-cell lymphoma in the sphenoid sinus: A case report and review of literature. 25-Jul-2020;11:208. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10155
Abstract
Background: Non-Hodgkin lymphomas (NHLs) in paranasal sinus are uncommon, accounting for 0.17–2% of all NHL cases; it is especially rare in the sphenoid sinus. In this report, we describe a case of NHL in the sphenoid sinus.
Case Description: A 66-year-old man presented with a sudden left eye movement disorder. His head computed tomography and gadolinium-enhanced magnetic resonance imaging (Gd-MRI) showed a mass lesion extending around the left sphenoid sinus. However, the tumor regrowth about twice was observed during 2 weeks, partial removal of tumor was performed by the endoscopic trans-nasal transsphenoidal surgery, then histologically proved it to be diffuse large B-cell lymphoma (DLBCL). After R-THP-COP regimen (rituximab 375 mg/m2,
Conclusion: NHLs in the sphenoid sinus is very rare disease, however, it is important to be diagnosed pathologically as soon as possible for being in remission state by the chemotherapy.
Keywords: Chemotherapy, Endoscopic trans-nasal transsphenoidal surgery, Non-Hodgkin lymphoma, Sphenoid sinus
INTRODUCTION
Non-Hodgkin lymphomas (NHLs) in paranasal sinus are uncommon, accounting for 0.17–2% of all NHL cases; it is especially rare in the sphenoid sinus.[
CASE PRESENTATION
A 66-year-old man was referred to our hospital with a sudden onset of headache, diplopia, and left ptosis. He was suffered from rheumatoid arthritis for several years and had taken methotrexate (MTX) tablets regularly. Neurological examinations revealed left oculomotor and trochlear nerve palsy without other cranial nerve disorders. Head computed tomography (CT) and gadolinium-enhanced brain magnetic resonance image (Gd-MRI) showed the mass lesion around the left sphenoid bone extending both to the left temporal middle fossa and to sphenoid sinus [
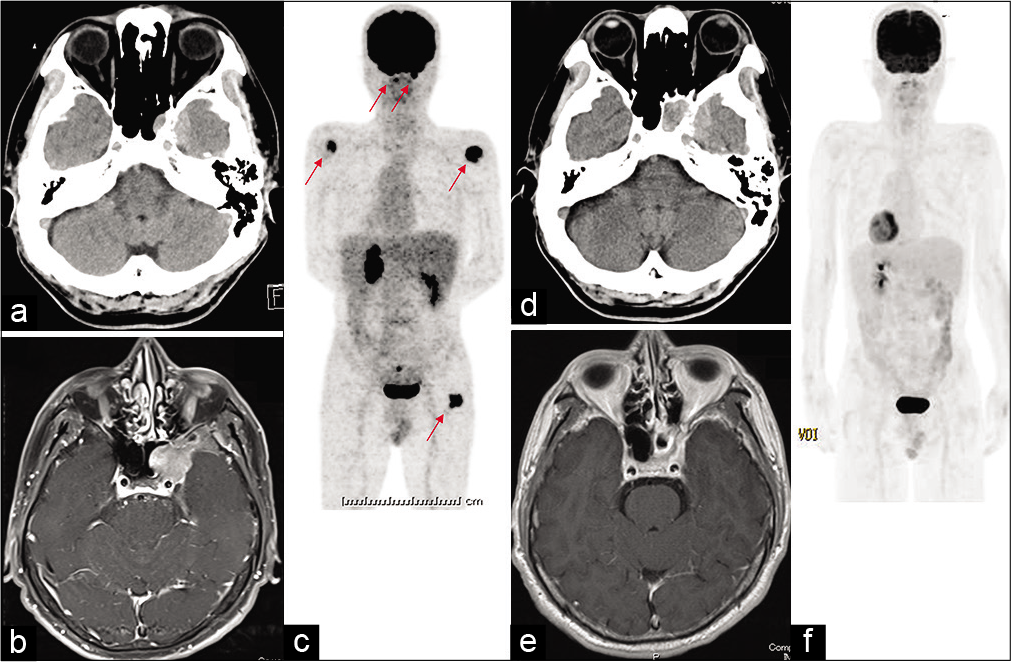
Figure 1:
Image examinations of the case. Head computed tomography examinations before operation showed the mass lesion around the left sphenoid bone extending to lateral to the left temporal middle fossa and medial to sphenoid sinus (a). The mass lesion was heterogeneously enhanced with the gadolinium-enhanced magnetic resonance image (Gd-MRI) (b). Fluorodeoxyglucose-positron emission tomography (FDG-PET) showed multiple lesions in the left sphenoid bone, nasal cavity, bilateral humeri, and left femur (c). Two weeks after the first presentation to our hospital, the tumor size was increased about the twice size compared as the previous study (d). After the removal of tumor and chemotherapy, his Gd- MRI and FDG-PET showed the disappearance of the lesion (e and f).
We thought that pathological examination was necessary to rule out malignant tumors. Fluorodeoxyglucose-positron emission tomography (FDG-PET) showed multiple lesions in the left sphenoid bone, nasal cavity, bilateral humeri, and left femur [
In spite of the cessation of oral MTX for rheumatoid arthritis for 2 weeks after the removal of tumor, the tumor regrowth was observed on the head CT. The patient was treated with R-THP- COP regimen (rituximab 375 mg/m2, cyclophosphamide 750 mg/m2, epirubicin 50 mg/m2, vincristine 2 mg/day, and prednisolone 100 mg/day) and two courses of intrathecal MTX therapy for central nervous system prophylaxis. After the eighth course of R-THP-COP, his Gd-MRI and FDG-PET showed the disappearance of the lesion [
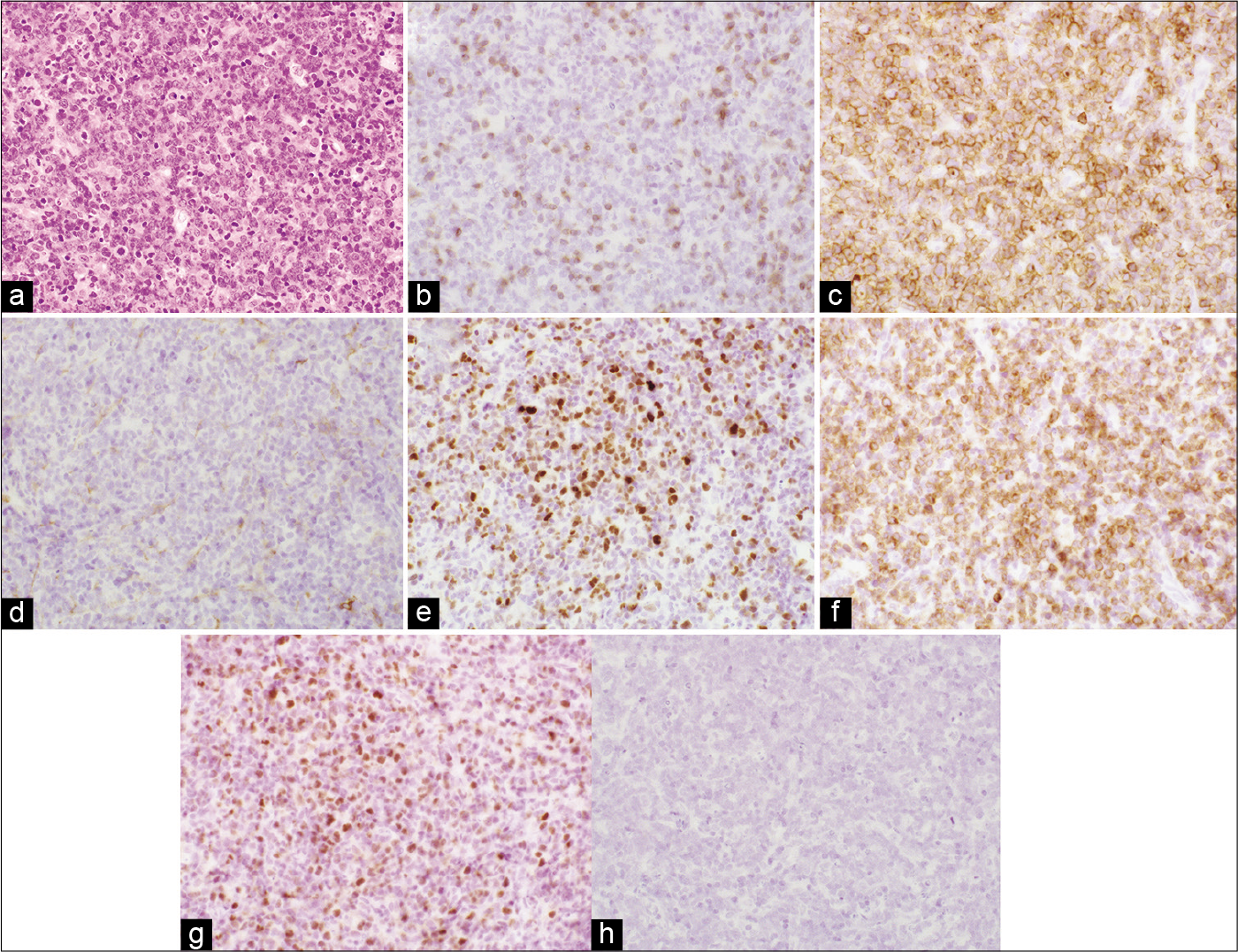
Histopathological examinations showed that large B cells with nuclei display prominent nucleoli that diffusely infiltrate the brain tissue in hematoxylin-eosin staining [
Figure 2:
Histopathological examinations including immunohistochemistry and flow cytometry showed that large cells with nuclei display prominent nucleoli that diffusely infiltrate the brain tissue in hematoxylin-eosin staining (a), cluster of differentiation (CD) 3(‒) (b), CD5(+) (c), CD10(‒) (d), multiple myeloma oncogene (MUM)-1(+) (e), Bcl-2(+) (f), Bcl-6(+) (g), and EBER (EBV-encoded small RNA) in situ hybridization (EBER-ISH) (‒) (h), thus the diagnosis was confirmed as diffuse large B-cell lymphoma.
DISCUSSION
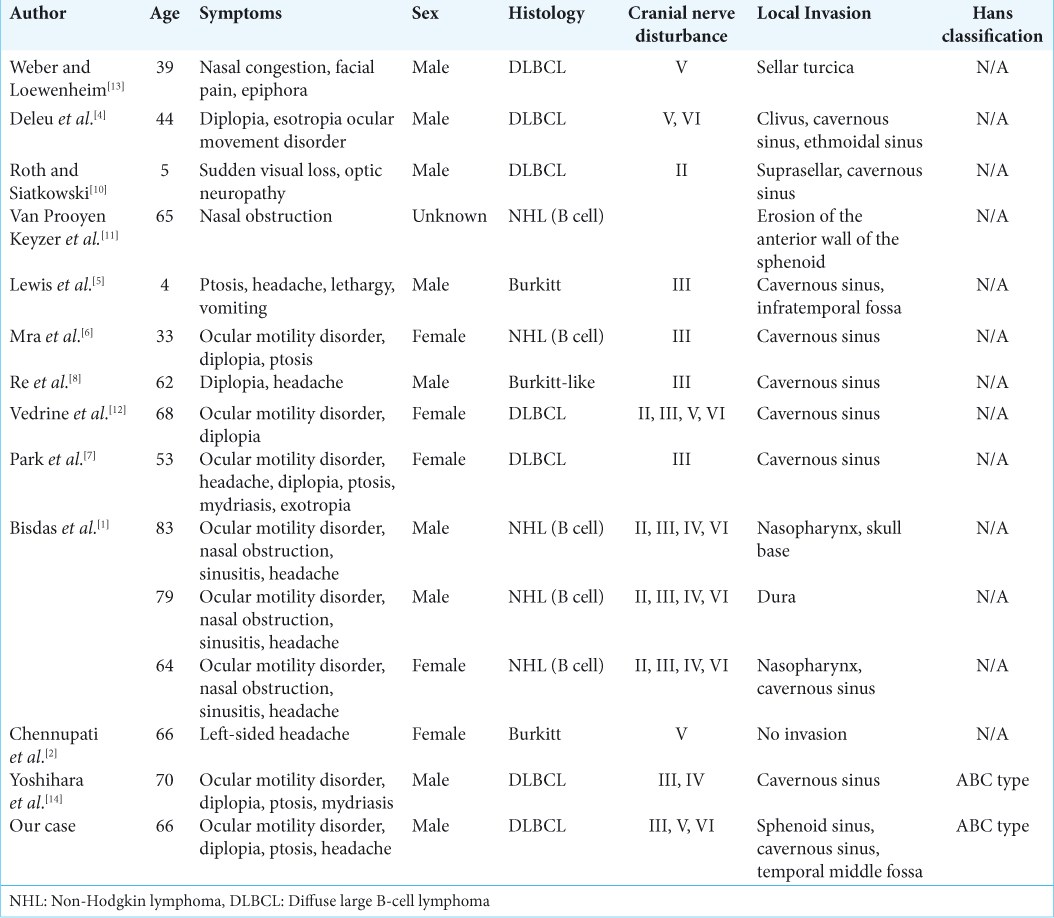
Primary malignancies of the sphenoid sinus, especially the lymphoma, are rare. As far as we have reviewed, 15 cases of sphenoid lymphoma including this case have been reported with detailed clinical history [
In our case, the patient had oral MTX tablets regularly for rheumatoid arthritis. We suspected the MTX-associated lymphoproliferative disorders; however, the regrowth after the cessation of oral MTX was observed. In addition, we diagnosed clinically this case as the DLBCL in the sphenoid sinus. Pathologically, many cases of MTX -associated lymphoproliferative disorders have been positive in EBER immunostaining;[
In clinical practice, it is known that definite histological diagnosis is required before the initiation of any treatment.[
CONCLUSION
NHLs in paranasal sinus are very rare, however, this should be considered as a differential diagnosis of paranasal sinus tumors.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bisdas S, Fetscher S, Feller AC, Baghi M, Knecht R, Gstoettner W. Primary B cell lymphoma of the sphenoid sinus: CT and MRI characteristics with correlation to perfusion and spectroscopic imaging features. Eur Arch Otorhinolaryngol. 2007. 264: 1207-13
2. Chennupati SK, Govindaraj S, Setzen G, Chiu AG. Adult Burkitt lymphoma originating in the sphenoid sinus: Case report and review of the literature. Ear Nose Throat J. 2009. 88: E07-
3. Cleary KR, Batsakis JG. Sinonasal lymphomas. Ann Otol Rhinol Laryngol. 1994. 103: 911-4
4. Deleu D, Lagopoulos M, Al Moundhry M, Katchy K. Isolated bilateral abducens nerve palsy in primary sphenoidal sinus non-Hodgkin lymphoma. Acta Neurol Belg. 2000. 100: 103-6
5. Lewis WB, Perlman PW, Ilasi J. Pediatric American Burkitt’s lymphoma of the sphenoid sinus. Otolaryngol Head Neck Surg. 2000. 123: 642-4
6. Mra Z, Roach JC, Brook AL. Infectious and neoplastic diseases of the sphenoid sinus-a report of 10 cases. Rhinology. 2000. 40: 34-40
7. Park YM, Cho JH, Cho JY, Huh JS, Ahn JY. Non-Hodgkin’s lymphoma of the sphenoid sinus presenting as isolated oculomotor nerve palsy. World J Surg Oncol. 2007. 5: 86-
8. Re M, Di Massimo U, Romeo R, Mallardi V. Burkitt-like lymphoma of the sphenoid sinus: Case report. Acta Otorhinolaryngol Ital. 2004. 24: 30-2
9. Rizzi R, Curci P, Delia M, Rinaldi E, Chiefa A, Specchia G. Spontaneous remission of methotrexate-associated lymphoproliferative disorders after discontinuation of immunosuppressive treatment for autoimmune disease. Review of the literature. Med Oncol. 2009. 26: 1-9
10. Roth DB, Siatkowski RM. Bilateral blindness as the initial presentation of lymphoma of the sphenoid sinus. Am J Ophthalmol. 2000. 129: 256-8
11. Van Prooyen Keyzer S, Eloy P, Delos M, Doyen C, Bertrand B, Rombaux P. Sinonasal lymphomas. Case report. Acta Otorhinolaryngol Belg. 2000. 54: 45-51
12. Vedrine PO, Thariat J, Merrot O, Percodani J, Dufour X, Choussy O. Primary cancer of the sphenoid sinus-a GETTEC study. Head Neck. 2009. 31: 388-97
13. Weber AL, Loewenheim H. Lymphoma of the sphenoid sinus presenting as an expansile mass. Ann Otol Rhinol Laryngol. 1993. 102: 318-21
14. Yoshihara S, Kondo K, Ochi A. Diffuse large B-cell lymphoma in the sphenoid sinus mimicking fibrous dysplasia in CT and MRI. BMJ Case Rep. 2014. 2014: 1-4