- Department of Neurosurgery, Hikone Chuo Hospital, Hikone, Japan
- Department of Radiology, Fujieda Municipal General Hospital, Fujieda, Japan
- Department of Physical Therapy, Faculty of Health and Medical Sciences, Hokuriku University, Kanazawa, Japan
- Department of Neurosurgery, Shizuoka General Hospital, Shizuoka, Japan.
Correspondence Address:
Yoshinori Maki, Department of Neurosurgery, Hikone Chuo Hospital, Hikone, Japan.
DOI:10.25259/SNI_156_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoshinori Maki1, Motohiro Takayama1, Tsuyoshi Okawa2, Akio Goda3, Akinori Miyakoshi4. Diffusion tensor imaging combined with the dual-echo steady-state (DESS) protocol for the evaluation of the median nerve in the carpal tunnel: A preliminary study. 29-Mar-2024;15:110
How to cite this URL: Yoshinori Maki1, Motohiro Takayama1, Tsuyoshi Okawa2, Akio Goda3, Akinori Miyakoshi4. Diffusion tensor imaging combined with the dual-echo steady-state (DESS) protocol for the evaluation of the median nerve in the carpal tunnel: A preliminary study. 29-Mar-2024;15:110. Available from: https://surgicalneurologyint.com/surgicalint-articles/12829/
Abstract
Background: Carpal tunnel syndrome (CTS) is diagnosed based on neurological, electrophysiology, and radiological findings. Due to the technical development of magnetic resonance imaging (MRI), the median nerve is evaluated with several MRI protocols. However, diffusion tensor imaging (DTI) combined with a dual-echo steady-state (DESS) protocol is not frequently used to evaluate the median nerve of CTS. This study aimed to evaluate the median nerve in the carpal tunnel using DTI combined with a DESS protocol.
Methods: Five healthy volunteers and seven patients with CTS were enrolled. The patients underwent MRI for CTS pre- and post-operatively. The median nerve was evaluated using a 3-T MRI scanner. The parameters of the DESS protocol were as follows: Repetition time (TR)/echo time (TE) = 10.83/3.32 ms, slice thickness = 0.45 mm, field of view (FoV) = 350 × 253 × 350 mm, and 3D voxel size = 0.5 × 0.5 ×0.4 mm. The parameters of the DTI sequence were as follows: TR/TE = 4000/86 ms, slice thickness = 3 mm, FoV = 160 × 993 × 90 mm, 3D voxel size = 1.2 × 1.2 ×3.0 mm, and b value = 0.1000 s/mm2. The apparent diffusion coefficient (ADC) and fractional anisotropy (FA) values of the median nerve were statistically analyzed. Statistical significance was set at P
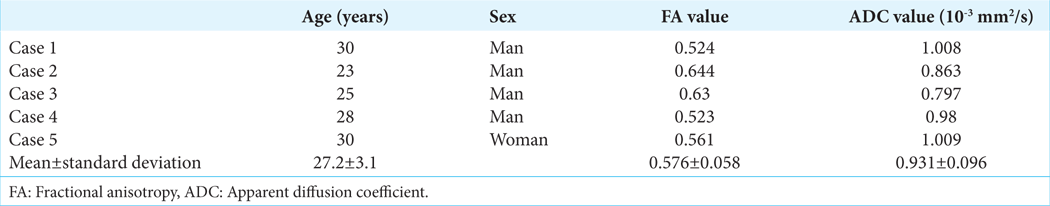
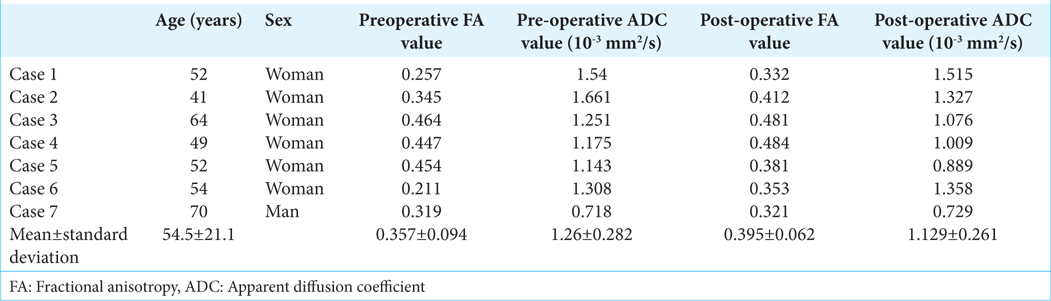
Results: The FA value of healthy volunteers was 0.576 ± 0.058, while those of the patients were 0.357 ± 0.094 and 0.395 ± 0.062 pre-and post-operatively, respectively. Statistically significant differences were identified between the FA values of healthy volunteers and pre-operative/post-operative patients. The ADC values of healthy volunteers and pre-operative patients were 0.931 ± 0.096 and 1.26 ± 0.282 (10-3 mm2/s), respectively (P
Conclusion: This MRI protocol may be useful for evaluating the median nerve in the carpal tunnel.
Keywords: Apparent diffusion coefficient, Diffusion tensor imaging, Dual-echo in the steady-state, Fractional anisotropy, Median nerve
INTRODUCTION
Carpal tunnel syndrome (CTS) is an entrapment neuropathy that irritates the median nerve.[
Several magnetic resonance imaging (MRI) protocols have been utilized to evaluate the median nerve in the carpal tunnel; however, the evaluation of the median nerve in the carpal tunnel with a dual-echo in the steady-state (DESS) protocol has not been described in detail.[
This study aimed to evaluate the ADC and FA values of the median nerve using the DESS protocol in healthy volunteers and patients with CTS. Changes between the pre-operative and post-operative ADC and FA values of patients with CTS were also analyzed.
MATERIALS AND METHODS
This study enrolled five healthy volunteers and seven patients with CTS after obtaining informed consent. MRI examination was performed according to the protocol described below. Healthy volunteers underwent MRI examination only once; in contrast, the patients with CTS underwent MRI examination twice, preoperatively and postoperatively (within three months after the surgery).
Protocol of MRI examination
MRI was performed using a 3-T MRI scanner (SIEMENS MAGNETOM Trio Tim Syngo MR B17). The wrist undergoing examination was slightly elevated, and a head coil was placed distal to the wrist joint. A single loop-coil of 7 cm diameter was set on the palm to increase the signal intensity. A DESS[
Statistical analysis
The ADC and FA values of the key slices of the median nerves were evaluated, and the data of the healthy volunteers were statistically compared with the pre-operative and postoperative data of the patients with CTS. The pre-operative and post-operative patient data were also compared. SPSS Statistics software (version 24; Chicago, Illinois, USA) was used to perform the statistical analyses. Student’s t-test was used to analyze the collected data. The power and effect size was evaluated using G* power (version 3.1.9.6, Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). A power ≥0.8 was defined as significant. A significant effect size was defined as a d > 0.8. Statistical significance was set at P < 0.05.
RESULTS
Data of healthy volunteers
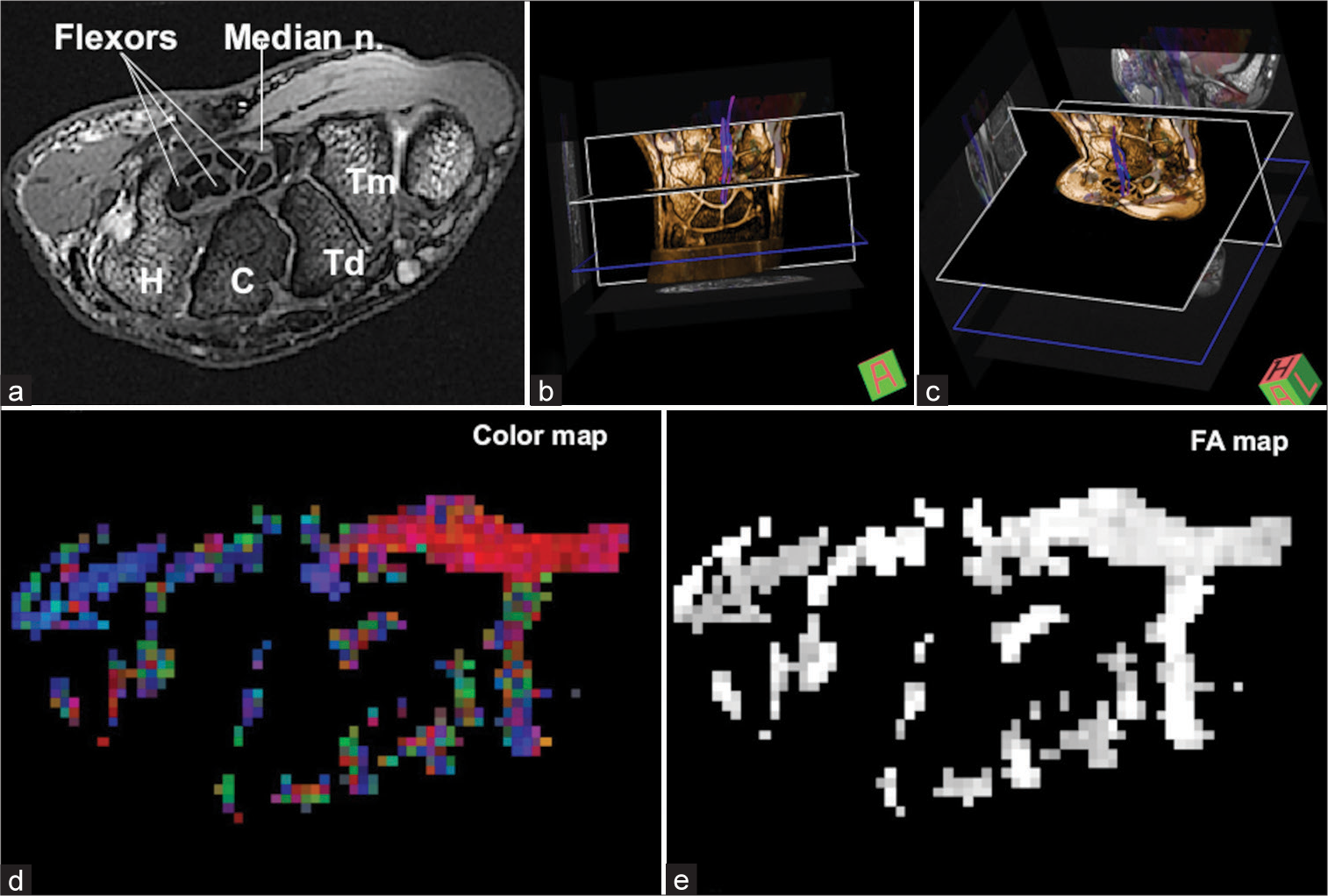
In healthy volunteers, the median nerve in the carpal tunnel could be clearly identified as superior to the tendons of the flexor muscle tendons on MR images [
Figure 1:
Representative data of a healthy volunteer (a) the median nerve can be observed on an image acquired using transversal DESS with fat suppression. (b and c) The median nerve can be visualized with fiber tractography. (d and e) Color map and FA map images were extracted to calculate the ADC and FA values of the median nerve. C: Os capitatum, H: Os hamatum, n.: Nerve, Td: Os trapezoideum, Tm: Os trapezium, FA: Fractional anisotropy, ADC: Apparent diffusion coefficient, DESS: Dual-echo in the steady-state.
Data of patients with CTS
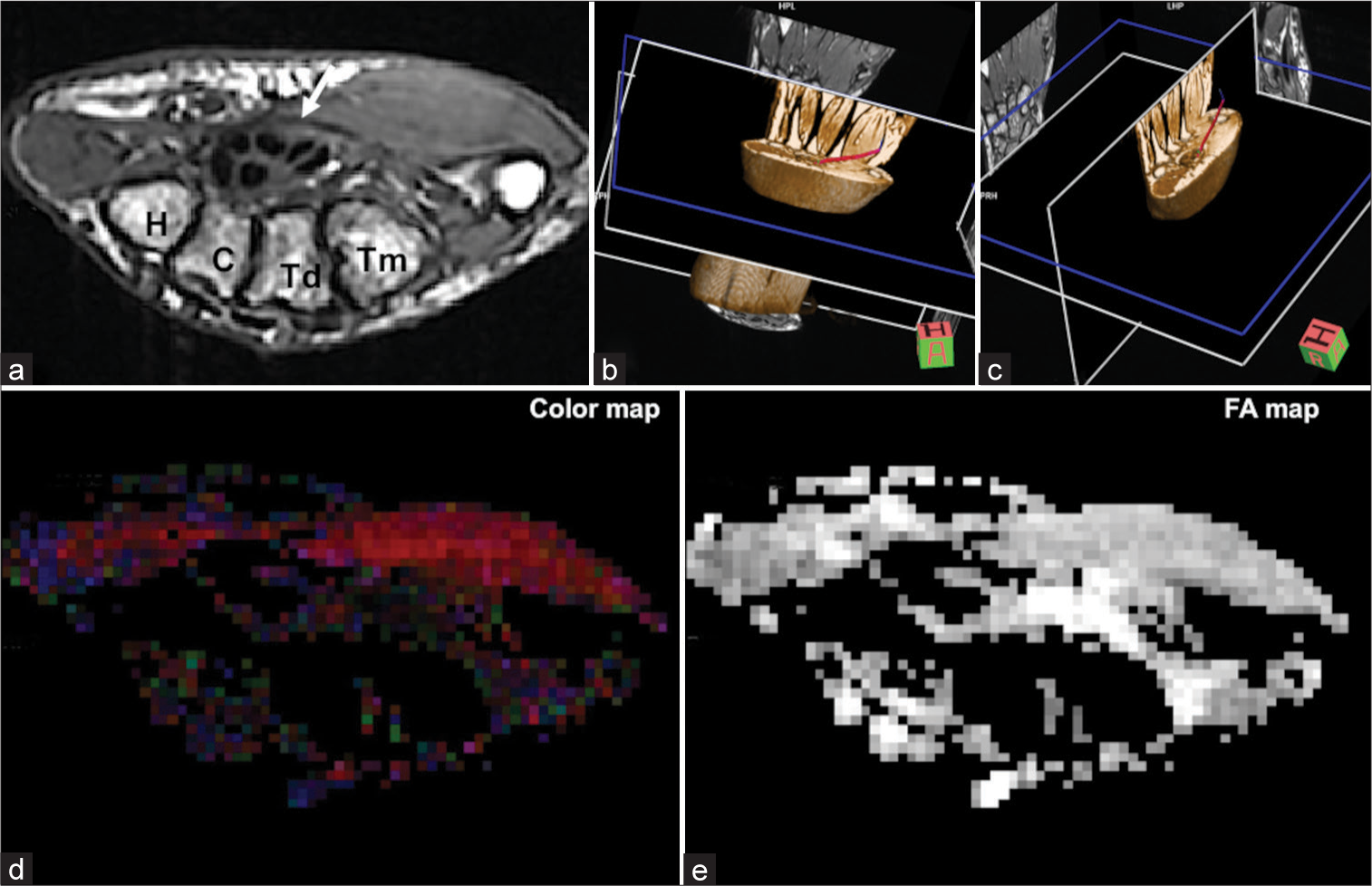
The median nerve in the carpal tunnel could be identified vaguely in patients with CTS. Moreover, it could not be visualized clearly with fiber tractography [
Figure 2:
Representative pre-operative data of a patient with carpal tunnel syndrome (a) the median nerve is not clearly visible compared with that of the healthy volunteer (white arrow). (b and c) The median nerve could not be detected with fiber tractography. (d and e) The color map and FA map images are not clear compared with those of the healthy volunteers. C: Os capitatum, H: Os hamatum, n.: Nerve, Td: Os trapezoideum, Tm: Os trapezium, FA: Fractional anisotropy.
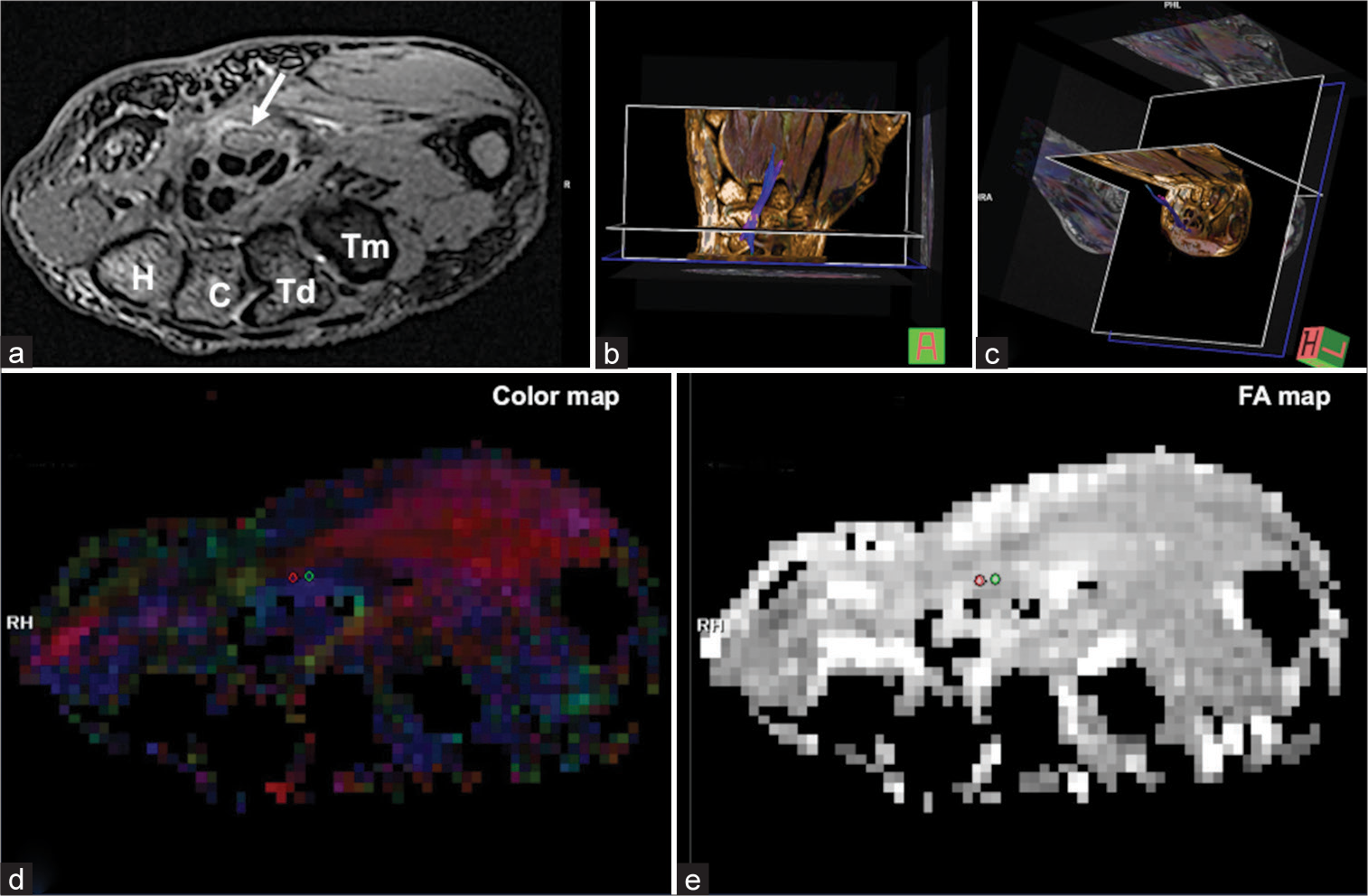
Figure 3:
Representative post-operative data of a patient with carpal tunnel syndrome (a-c) Postoperatively, the median nerve could be identified on an image acquired using DESS with fat suppression and fiber tractography. (d and e) A lesion on the median nerve to extract ADC and FA values was easily identified. C: Os capitatum, H: Os hamatum, n.: Nerve, Td: Os trapezoideum, Tm: Os trapezium, ADC: Apparent diffusion coefficient, FA: Fractional anisotropy, DESS: Dual-echo in the steady-state.
No statistically significant difference was identified between the ADC values of the healthy volunteers and the postoperative FA values of the patients with CTS (P = 0.124). The d values of the ADC and FA values were 0.87 and 2.86, respectively. The powers of the ADC and FA values were 0.27 and 0.99, respectively. The paired samples t-test did not detect a statistically significant difference between the pre-operative and post-operative ADC and FA values of the patients with CTS (ADC values: P = 0.057, FD values: P = 0.184). The d values of the ADC and FA values were 1.91 and 1.22, respectively. The powers of the ADC and FA values were 0.99.
DISCUSSION
In this study, the median nerve in healthy volunteers and patients with CTS was objectively evaluated using DTI combined with a DESS protocol. The median nerve could be visualized clearly in healthy volunteers, whereas the median nerve could be visualized only vaguely in patients with CTS preoperatively. However, the median nerve could be visualized clearly postoperatively. The ADC and FA values of the median nerve at the level of the hook of the hamate were also analyzed. The pre-operative ADC and FA values of the patients with CTS were significantly higher than those of the healthy volunteers. Although no statistically significant differences were detected, the median ADC values decreased, and the median FA values increased postoperatively. The previous studies evaluating the median nerve in the carpal tunnel utilized MRI sequences, such as read-out segment echo-planar imaging and single-shot echo-planar imaging.[
Limitations
Only a limited number of healthy volunteers and patients with CTS were recruited in this study. The distribution of the age and sex in those groups was not equivalent. This limitation could have been a confounding factor and could have affected the statistical results, such as the insufficient power of the ADC values in our study. A DESS protocol with fat suppression was used to collect clinical data in our study. However, reports on the use of this sequence for the evaluation of the medial nerve in the carpal tunnel are scarce. Thus, the optimal parameters of the DESS protocol with fat suppression for evaluating the median nerve in patients with CTS should be investigated in future studies. In addition, the ADC and FA values were compared between healthy volunteers and patients with CTS. However, these values were not evaluated based on subjective and objective clinical findings from questionnaires or nerve conduction studies. The correlation between the ADC and FA values and clinical symptoms should also be addressed in future studies. Finally, patients with CTS were followed up for a limited period postoperatively in this study. Due to the patient’s wishes, the timing of the post-operative MRI examination was not completely standardized, which may have affected the postoperative ADC and FA values. It is also necessary to evaluate whether the ADC and FA values of the median nerve in patients with CTS chronologically shift to those of healthy volunteers.
CONCLUSION
DESS with fat-suppression protocol may be useful for evaluating the median nerve in the carpal tunnel. Further research is required to optimize this sequence for clinical use.
Ethical Approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Andreisek G, White LM, Kassner A, Sussman MS. Evaluation of diffusion tensor imaging and fiber tractography of the median nerve: Preliminary results on intrasubject variability and precision of measurements. AJR Am J Roentgenol. 2010. 194: W65-72
2. Brienza M, Pujia F, Colaiacomo MC, Anastasio MG, Pierelli F, Di Biasi C. 3T diffusion tensor imaging and electroneurography of peripheral nerve: A morphofunctional analysis in carpal tunnel syndrome. J Neuroradiol. 2014. 41: 124-30
3. Cingoz M, Kandemirli SG, Alis DC, Samanci C, Kandemirli GC, Adatepe NU. Evaluation of median nerve by shear wave elastography and diffusion tensor imaging in carpal tunnel syndrome. Eur J Radiol. 2018. 101: 59-64
4. Eladawi S, Balamoody S, Amerasekera S, Choudhary S. 3T MRI of wrist ligaments and TFCC using true plane oblique 3D T2 Dual Echo Steady State (DESS)-a study of diagnostic accuracy. Br J Radiol. 2022. 95: 20210019
5. Filli L, Piccirelli M, Kenkel D, Boss A, Manoliu A, Andreisek G. Accelerated magnetic resonance diffusion tensor imaging of the median nerve using simultaneous multi-slice echo planar imaging with blipped CAIPIRINHA. Eur Radiol. 2016. 26: 1921-8
6. Genova A, Dix O, Saefan A, Thakur M, Hassan A. Carpal tunnel syndrome: A review of literature. Cureus. 2020. 12: e7333
7. Kim Y, Jeong HS, Kim HJ, Seong M, Kim Y, Kim ST. Three-dimensional double-echo steady-state with water excitation magnetic resonance imaging to localize the intraparotid facial nerve in patients with deep-seated parotid tumors. Neuroradiology. 2021. 63: 731-9
8. Koh SH, Kwon BC, Park C, Hwang SY, Lee JW, Kim SS. A comparison of the performance of anatomical MRI and DTI in diagnosing carpal tunnel syndrome. Eur J Radiol. 2014. 83: 2065-73
9. Kwon BC, Koh SH, Hwang SY. Optimal parameters and location for diffusion-tensor imaging in the diagnosis of carpal tunnel syndrome: A prospective matched case-control study. AJR Am J Roentgenol. 2015. 204: 1248-54
10. Liu C, Li HW, Wang L, Zhu L, Jiang XF, Yang MJ. Optimal parameters and location for diffusion tensor imaging in the diagnosis of carpal tunnel syndrome: A meta-analysis. Clin Radiol. 2018. 73: 1058.e11-9
11. Lindberg PG, Feydy A, Le Viet D, Maier MA, Drapé JL. Diffusion tensor imaging of the median nerve in recurrent carpal tunnel syndrome-initial experience. Eur Radiol. 2013. 23: 3115-23
12. Miwa T, Miwa H. Ultrasonography of carpal tunnel syndrome: Clinical significance and limitations in elderly patients. Intern Med. 2011. 50: 2157-61
13. Naraghi A, da Gama Lobo L, Menezes R, Khanna M, Sussman M, Anastakis D. Diffusion tensor imaging of the median nerve before and after carpal tunnel release in patients with carpal tunnel syndrome: Feasibility study. Skeletal Radiol. 2013. 42: 1403-12
14. Razek AA, Shabana AA, El Saied TO, Alrefey N. Diffusion tensor imaging of mild-moderate carpal tunnel syndrome: Correlation with nerve conduction study and clinical tests. Clin Rheumatol. 2017. 36: 2319-24
15. Roemer FW, Kwoh CK, Hannon MJ, Crema MD, Moore CE, Jakicic JM. Semiquantitative assessment of focal cartilage damage at 3 T MRI: A comparative study of dual echo at steady state (DESS) and intermediate-weighted (IW) fat suppressed fast spin echo sequences. EurJ Radiol. 2011. 80: e126-31
16. Rojoa D, Raheman F, Rassam J, Wade RG. Meta-analysis of the normal diffusion tensor imaging values of the median nerve and how they change in carpal tunnel syndrome. Sci Rep. 2021. 11: 20935
17. Schmid AB, Campbell J, Hurley SA, Jbabdi S, Andersson JL, Jenkinson M. Feasibility of diffusion tensor and morphologic imaging of peripheral nerves at ultra-high field strength. Invest Radiol. 2018. 53: 705-15
18. Stecco C, Giordani F, Fan C, Biz C, Pirri C, Frigo AC. Role of fasciae around the median nerve in pathogenesis of carpal tunnel syndrome: Microscopic and ultrasound study. J Anat. 2020. 236: 660-7
19. Wang CK, Jou IM, Huang HW, Chen PY, Tsai HM, Liu YS. Carpal tunnel syndrome assessed with diffusion tensor imaging: Comparison with electrophysiological studies of patients and healthy volunteers. Eur J Radiol. 2012. 81: 3378-83
20. Wipperman J, Goerl K. Carpal tunnel syndrome: Diagnosis and management. Am Fam Physician. 2016. 94: 993-9