- Department of Neurosurgery, Aga Khan University, Karachi, Pakistan
- Department of Radiology, Aga Khan University, Karachi, Pakistan
- Department of Neurosurgery, Aga Khan University, Karachi, Pakistan
Correspondence Address:
Fatima Mubarak
Department of Neurosurgery, Aga Khan University, Karachi, Pakistan
DOI:10.4103/sni.sni_300_18
Copyright: © 2019 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Syeda Maheen Batool, Fatima Mubarak, Syed Ather Enam. Diffusion-weighted magnetic resonance imaging may be useful in differentiating fungal abscess from malignant intracranial lesion: Case report. 25-Jan-2019;10:13
How to cite this URL: Syeda Maheen Batool, Fatima Mubarak, Syed Ather Enam. Diffusion-weighted magnetic resonance imaging may be useful in differentiating fungal abscess from malignant intracranial lesion: Case report. 25-Jan-2019;10:13. Available from: http://surgicalneurologyint.com/surgicalint-articles/9195/
Abstract
Background:Diffusion-weighted magnetic resonance has a well-defined role in differentiating between important intracranial lesions. Sometimes, the surgeon is faced with a dilemma of how to diagnose an infectious versus malignant lesion.
Case Description:A 28-year-old male presented to the neurosurgery clinic with complaints of headache and left-sided weakness for 2 weeks. Neurological examination was intact. Magnetic resonance imaging (MRI) scan showed a large infiltrating heterogeneous mass involving the right parietal lobe. On further reviewing, there was homogenous diffusion restriction in the center of lesion. In addition, its aggressive behavior confirmed it to be a fungal abscess.
Conclusions:Correctly identifying an infectious versus tumor etiology is important. Research has been carried out to employ diffusion-weighted imaging (DWI) in differentiating the variable radiological findings. The role of DWI in diagnosing bacterial abscess is more commonly seen in comparison to fungal abscess. DWI has a high diagnostic potential, but more works need to be done.
Keywords: Diagnosis, diffusion-weighted imaging, fungal, radiology, tumor
INTRODUCTION
In neurosurgical practice, an essential component of the diagnostics is the use of relevant radiological imaging modality in order to localize and diagnose an intracranial lesion.
Among the various diagnostic tests available, this paper will discuss the role of diffusion-weighted magnetic resonance. Diffusion-weighted imaging (DWI) has a well-defined role in differentiating between important intracranial lesions, namely, brain abscess, arachnoid cyst, cystic/necrotic tumor, and epidermoid tumor. Quantitative analysis allows one to clearly delineate vascular, inflammatory, metabolic, infectious, and nonvascular disorders.[
This process of identification is based on the measure of resistance to random water diffusion secondary to important tissue properties, including the degree of cellularity, presence of inflammatory infiltrate, viscosity of fluid, and loss of cell membrane. This can be quantified using apparent diffusion coefficient (ADC). Broadly speaking, a lesion can have a high signal intensity on DWI (due to restriction to water diffusion) associated with low ADC score or a low signal intensity associated with a higher ADC score.[
This case report discusses the presentation of a fungal infection and its differentiation from a neoplasm based on radiological investigations and histopathology studies.
CASE PRESENTATION
A 28-year-old male presented to the neurosurgery clinic with complaints of headache and left-sided weakness for 2 weeks. He had no previously known comorbidities. His past medical history was not significant for diabetes or any immunocompromised state.
General physical examination was unremarkable. On neurological examination, Glasgow coma scale (GCS) score was 15. The patient was alert, awake, and oriented to time, place, and person. Pupils were bilaterally equal and reactive. No cranial nerve deficits were found. Motor examination revealed normal bulk and tone with power of 5/5 in upper and lower limbs bilaterally and the reflexes were normal. Sensory system was intact with no deficits.
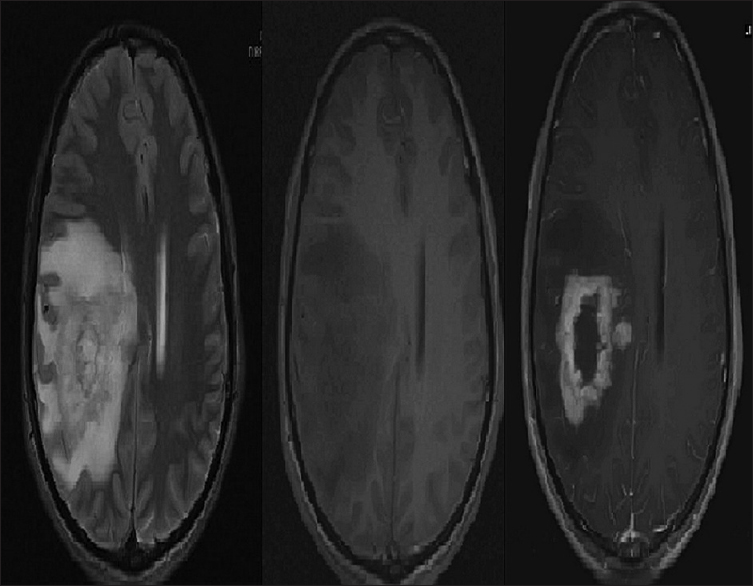
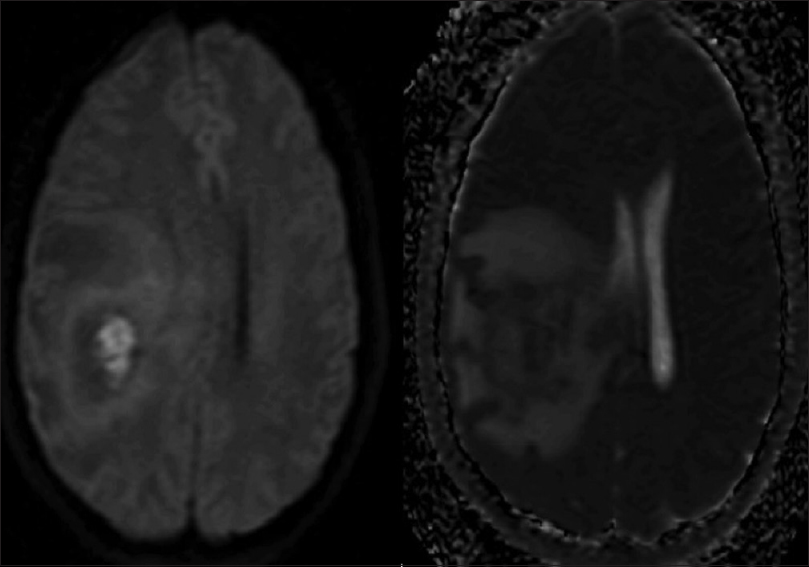
The investigation done to arrive at a diagnosis included magnetic resonance imaging (MRI). The scan showed a large infiltrating heterogeneous mass involving the right parietal lobe. The mass was also seen to be extending to corpus callosum. Based on these features, a presumptive diagnosis of a neoplastic mass, most likely glioblastoma, was made. Images are shown in
On further reviewing of DWI, there was homogenous diffusion restriction in the center of lesion. In addition, its aggressive behavior as evident by conventional sequences confirmed it to be a fungal abscess as shown in
Subsequently, patient was planned for neuronavigation-guided craniotomy and excision of the space-occupying lesion. Intraoperatively, a firm-to-hard diffuse mass was noted in the right parietal lobe with mild-to-moderate vascularity. Postoperatively, patient recovered well and had no neurological deficits.
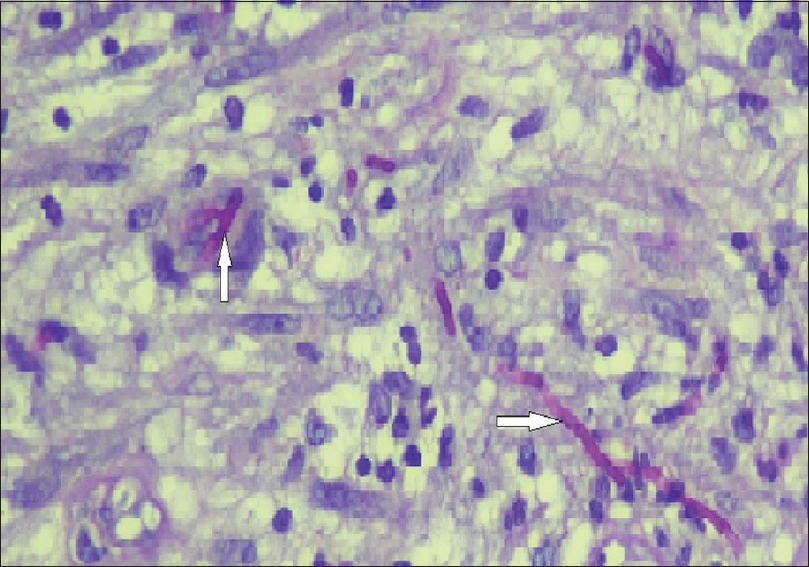
Microscopic examination of the resected lesion showed dense acute and chronic inflammation along with scattered granulomas and multinucleated giant cells. Rhinocladiella mackenziei was identified as the causative pathogen in the fungal culture as shown in
Patient was started on antifungal therapy. The patient remained stable and afebrile. Occupational physiotherapy was done. Patient was discharged in a stable condition.
DISCUSSION
Correctly identifying an infectious versus tumor etiology is important but sometimes difficult. This improves patient outcomes, incurs less treatment costs, and determines the optimal site (periphery vs. core) for taking a tissue biopsy. In addition, if a presurgical diagnosis of a fungal abscess is made, it is possible to premedicate the patient with appropriate antifungal therapy.
Research has been carried out in the last decade or so to determine and suggest useful ways to employ DWI in achieving this purpose. A study looked at the effectiveness of ADC and DWI in differentiating brain abscess from a cystic or necrotic tumor. Variable degree of increased signal intensity was seen in all pyogenic lesions on DWI along with low ADC scores (mean ADCR = 0.63 mm2/s). As expected, all tumors were seen as low-signal intensity areas with high ADC scores (mean ADCR = 3.42 mm2/s).[
In short, lesions appearing hypointense (consistent with elevated diffusion) on DWI are likely to be representative of tumor, toxoplasmosis, and ischemic infarction. In contrast, a pyogenic abscess will be seen as a hyperintense region with restricted water diffusion.
Fungal infection, however, can demonstrate variable radiological presentation. Focal cerebritis will be seen as a hyperintense region on DWI. Frank abscess presents as a well-circumscribed, rim-enhancing lesion with surrounding edema and diffusion restriction.[
The patient, discussed in this case report, did not have any clinical features suggestive of meningitis or raised intracranial pressure. R. mackenziei, the pathogen isolated in this case, occurs commonly in immunocompetent people. It has variable presentation including brain abscess, skin manifestations, headache, and hemiparesis.[
The role of DWI in diagnosing bacterial abscess is more commonly seen in comparison to fungal abscess. Consequently, no well-defined radiological criteria to diagnose a fungal abscess have been established yet. DWI has a high diagnostic potential, but more works need to be done to aid the surgeon in making a prompt and efficacious therapeutic decision.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chang SC, Lai PH, Chen WL, Weng HH, Ho JT, Wang JS. Diffusion-weighted MRI features of brain abscess and cystic or necrotic brain tumors: Comparison with conventional MRI. Clin Imaging. 2002. 26: 227-36
2. Finelli PF, Gleeson E, Ciesielski T, Uphoff DF. Diagnostic role of target lesion on diffusion-weighted imaging: A case of cerebral aspergillosis and review of the literature. Neurologist. 2010. 16: 364-7
3. Guzman R, Barth A, Lovblad KO, El-Koussy M, Weis J, Schroth G. Use of diffusion-weighted magnetic resonance imaging in differentiating purulent brain processes from cystic brain tumors. J Neurosurg. 2002. 97: 1101-7
4. Jabeen K, Farooqi J, Zafar A, Jamil B, Mahmood SF, Ali F. Rhinocladiella mackenziei as an emerging cause of cerebral phaeohyphomycosis in Pakistan: A case series. Clin Infect Dis. 2011. 52: 213-7
5. Kastrup O, Wanke I, Maschke M. Neuroimaging of Infections. NeuroRx. 2005. 2: 324-32
6. Leuthardt EC, Wippold FJ, Oswood MC, Rich KM. Diffusion-weighted MR imaging in the preoperative assessment of brain abscesses. Surg Neurol. 2002. 58: 395-402
7. Mascalchi M, Filippi M, Floris R, Fonda C, Gasparotti R, Villari N. Diffusion-weighted MR of the brain: Methodology and clinical application. Radiol Med. 2005. 109: 155-97
8. Naggara O, Letourneau-Guillon L, Mellerio C, Belair M, Pruvo JP, Leclerc X. Diffusion-weighted MR imaging of the brain. J Radiol. 2010. 91: 329-51
9. Taj-Aldeen SJ, Almaslamani M, Alkhalf A, Al Bozom I, Romanelli AM, Wickes BL. Cerebral phaeohyphomycosis due to Rhinocladiella mackenziei (formerly Ramichloridium mackenziei): A taxonomic update and review of the literature. Med Mycol. 2010. 48: 546-56
10. Velayudhan V, Chaudhry ZA, Smoker WRK, Shinder R, Reede DL. Imaging of intracranial and orbital complications of sinusitis and atypical sinus infection: What the Radiologist needs to know. Curr Probl Diagn Radiol. 2017. 46: 441-51