- Department of Neurosurgery, Kagoshima University, Kagoshima, Japan,
- Department of Radiology, Izumi Regional Medical Center, Akune, Japan,
- Department of Orthopedics, Yoshii-chuo Hospital, Izumi, Japan,
- Department of Neurologic Surgery, Mayo Clinic, Rochester, Minnesota, United States,
- Department of Otolaryngology, Head and Neck Surgery, Graduate School of Medical and Dental Sciences, Kagoshima University, Kagoshima, Japan.
Correspondence Address:
Kazunori Arita, Department of Neurosurgery, Kagoshima University, Kagoshima, Japan.
DOI:10.25259/SNI_1220_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tomohisa Okada1, Kaisei Makimoto2, Riichiro Yoshii3, Koji Yoshimoto1, F. M. Moinuddin4, Masaru Yamashita5, Kazunori Arita1. Dissecting aneurysm of the anterior inferior cerebellar artery in the internal auditory canal presenting with deafness without hemorrhage: A case report and literature review. 11-Mar-2022;13:88
How to cite this URL: Tomohisa Okada1, Kaisei Makimoto2, Riichiro Yoshii3, Koji Yoshimoto1, F. M. Moinuddin4, Masaru Yamashita5, Kazunori Arita1. Dissecting aneurysm of the anterior inferior cerebellar artery in the internal auditory canal presenting with deafness without hemorrhage: A case report and literature review. 11-Mar-2022;13:88. Available from: https://surgicalneurologyint.com/surgicalint-articles/11434/
Abstract
Background: Anterior inferior cerebellar artery (AICA) aneurysms in the internal auditory canal (IAC) are rare. We have reported a case of dissecting AICA aneurysm in the IAC presenting initially with the eighth nerve palsy followed by the seventh nerve palsy without hemorrhage.
Case Description: A 68-year-old woman presented with a sudden onset of vertigo accompanied by deafness and tinnitus on the right side that was preceded by intermittent right retroauricular pain 2 weeks before. Audiogram showed severe sensorineural hearing loss. Computed tomography and magnetic resonance imaging (MRI) indicated absence of prior subarachnoid hemorrhage. Magnetic resonance angiogram (MRA) suggested a tiny aneurysm at the fundus of the IAC accompanied with thinning of the lateral pontine segment of the AICA. Conservative treatment led to moderate improvement of the symptoms. However, the patient developed the right retroauricular pain again, followed by the right facial paralysis 5 months later but still without signs of hemorrhage on MRI. Digital subtraction angiogram showed dissecting aneurysm in the IAC. The patient was managed with oral steroids and direct intervention was avoided due to a risk of ischemia supposed by large area irrigated by the AICA. Follow-up MRA 18 months after the first presentation showed improvement in the narrowing of the AICA proximal to the aneurysm. The patient was functionally independent despite right-sided hearing loss and slight facial paresis.
Conclusion: This report warns physicians that a dissecting AICA aneurysm without subarachnoid hemorrhage may cause eighth and seventh nerve palsy.
Keywords: Anterior inferior cerebellar artery, Deafness, Dissecting aneurysm, Facial palsy. Internal auditory canal
INTRODUCTION
Aneurysm of the anterior inferior cerebellar artery (AICA) comprises 1–2% of all intracranial aneurysms.[
CASE REPORT
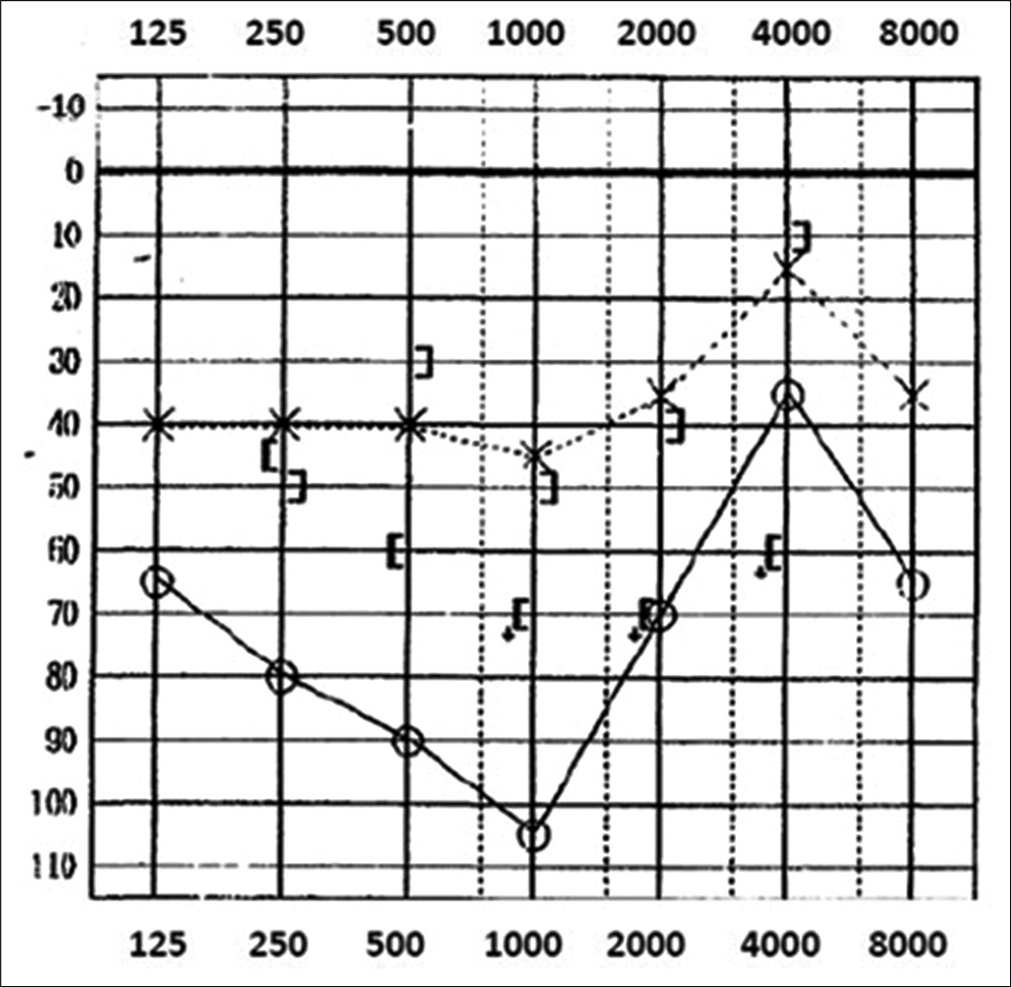
A 68-year-old woman with hypertension and dyslipidemia had intermittent right retroauricular pain, which was controlled by analgesics. Two weeks later, she presented with severe vertigo and nausea accompanied with the right-sided deafness and tinnitus. Computed tomography (CT) showed no abnormalities such as SAH or hematoma. Neurological examination showed no abnormalities, except unilateral deafness and persistent spontaneous left beating nystagmus. Pure tone audiogram revealed severe sensorineural hearing loss with an average air conduction threshold of 92.5 dB [
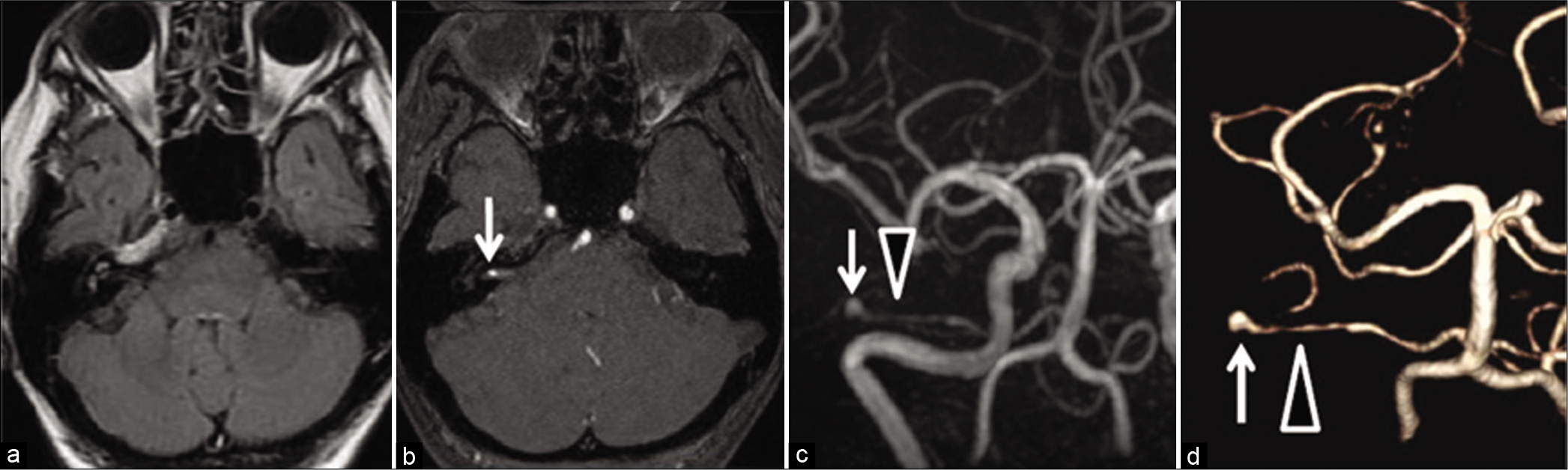
Magnetic resonance imaging (MRI) showed no abnormalities suggestive of prior SAH on fluid attenuated inversion recovery (FLAIR) and T2* images [
Figure 2:
Magnetic resonance imaging at the initial presentation. (a) A fluid-attenuated inversion recovery image of cerebellopontine angle showed no subarachnoid hemorrhage nor mass lesion. (b) A source image of magnetic resonance angiography (MRA) showed a dot (arrow) of arterial flow in fundus of the right internal auditory canal (IAC). (c) MRA showed thinning of right anterior inferior cerebellar artery (AICA) (arrowhead) in premeatal portion of lateral pontine segment and aneurysmal dilatation (arrow) in its meatal portion. (d) Volume rendering image also showed “string (arrowhead) and pearl (arrow)” in the AICA.
MRA showed narrowing in the premeatal portion of the lateral pontine segment and aneurysmal dilatation in the meatal portion, the string and pearl sign, in the right AICA, suggestive of dissecting aneurysm [
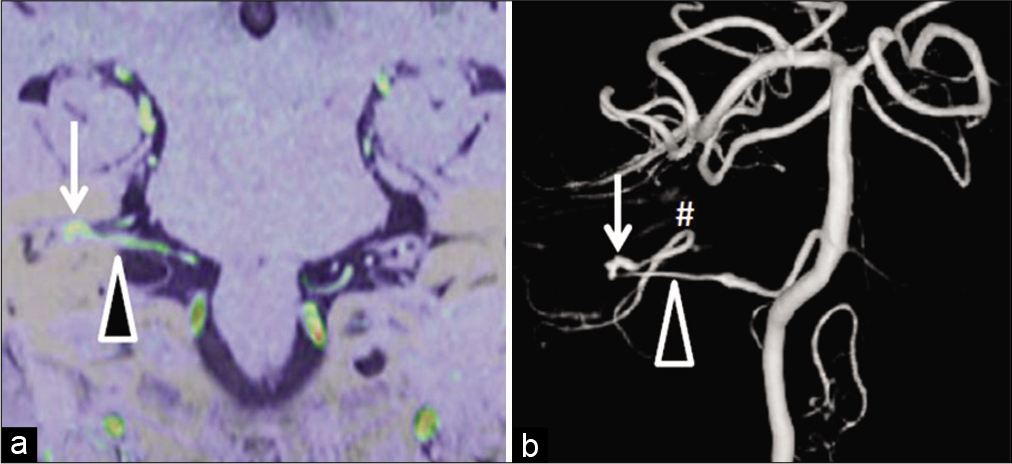
Five months after onset, the patient had transient right retroauricular pain again, followed by right facial paresis, which gradually progressed to House–Brackmann (HB) Grade IV. The average air conduction hearing was almost same as 2 months before, with a threshold of 73.8 dB. MRA showed a similar degree of narrowing of the AICA and intrameatal aneurysm with different shape [
Figure 3:
Angiogram at the emergence of facial nerve paresis 5 months after onset. (a) MRA source image superimposed on coronal 3D-constructive interference in steady-state image showed lateral pontine segment (arrowhead) of the anterior inferior cerebellar artery (AICA) and the aneurysm (arrow) in the fundus of IAC. (b) Digital subtraction angiogram showed thinning of the AICA (arrowhead) proximal to aneurysm (arrow) suggesting the dissection of the AICA. Flocculopeduncular segment was noted (#). Ipsilateral posterior inferior cerebellar artery was absent.
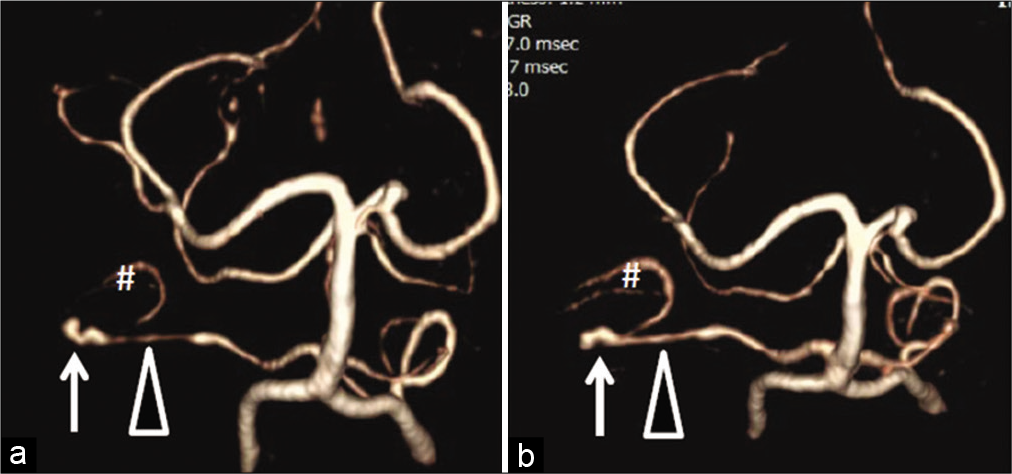
MRA at 18 months after onset showed slight increase in diameter of the AICA and slight decrease in the aneurysmal size compared to those 13 months before [
Figure 4:
Change in appearance of the AICA on volume rendering MRA images. (a) At the emergence of facial paresis 5 months after onset arrow: aneurysm, arrowhead: lateral pontine segment of AICA, #: flocculopeduncular segment of AICA. (b) At 18 months after onset. At 18 months after onset, the aneurysm size slightly decreased (arrow), caliber of the AICA (arrowhead) slightly increased, and flocculopeduncular segment (#) became apparent compared to that 13 months before.
Due to the absence of rupture during the clinical course, mild residual symptoms, improvement in the narrowing of the parent artery, and supposed wide irrigation area by the AICA due to the lack of ipsilateral PICA, we considered further follow-up under blood pressure control rather than direct intervention, which may result in serious neurological sequelae.
DISCUSSION
This is a rare case with intrameatal dissecting AICA aneurysm that presented with the eighth and then seventh nerve palsy without hemorrhage.
The AICA is anatomically divided into four segments – anterior pontine, lateral pontine, flocculopeduncular, and cortical segment.[
To the best of our knowledge, intrameatal AICA aneurysm has been reported in only 26 patients (21 women), including our patient.[
Twenty-one (80.8%) patients were admitted due to SAH as the initial presentation.[
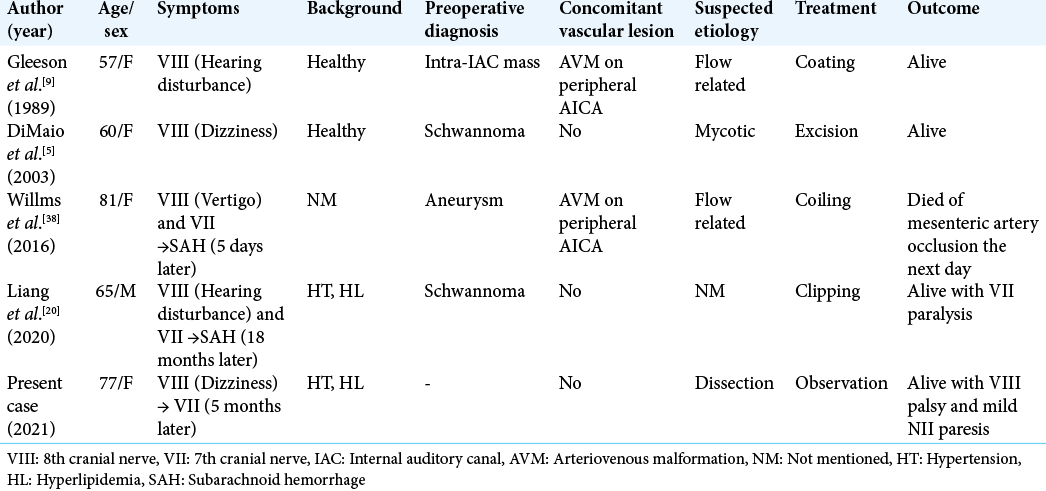
Five (19.2%) patients, including our patient, sought medical attention due to acute or slowly progressing eighth nerve symptom without SAH [
Among the 16 cases of dissecting AICA aneurysms reported,[
The patient in this case report had an unruptured dissecting AICA aneurysm. The natural course of unruptured intracranial arterial dissection is completely different from that of ruptured one. The recurrent bleeding rate of ruptured dissecting aneurysm is quite high at 14.1–71.4%.[
Although our patient’s right ear deafness persisted, she was able to work and right facial nerve paresis and narrowing of dissected segment of AICA showed some improvement at the last follow-up. Surgical trapping or endovascular treatment may result in worsening of facial nerve paresis and infarction in the cerebellum and/or brachium pontis considering the suspected wide area irrigated by the AICA in our patient. Due to these reasons, we chose a strategy of close monitoring under blood pressure control for this particular case.
CONCLUSION
We have reported the first case of intrameatal dissecting AICA aneurysm presenting with the eighth nerve symptom without SAH, which did not ruptured for >20 months under blood pressure control.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Haibunsha Kagoshima for giving productive comments on this manuscript and Editage (www.editage.com) for English language editing.
References
1. Andrade G, Faquini I, Azevedo-Filho H, Laércio J, Câmara D, Mendes JC. Dissecting anterior inferior cerebellar artery aneurysm treated by endovascular route. Arq Neuropsiquiatr. 2010. 68: 645-7
2. Bambakidis NC, Manjila S, Dashti S, Tarr R, Megerian CA. Management of anterior inferior cerebellar artery aneurysms: An illustrative case and review of literature. Neurosurg Focus. 2009. 26: E6
3. Castaigne P, Pertuiset B, Cambier J, Brunet P. Aneurysm of the internal auditory artery revealed by recurrent facial paralysis. Radical cure. Presse Med. 1967. 75: 2493-6
4. Choi CH, Cho WH, Choi BK, Lee SW. Rerupture following endovascular treatment for dissecting aneurysm of distal anterior inferior cerebellar artery with parent artery preservation: Retreatment by parent artery occlusion with Guglielmi detachable coils. Acta Neurochir (Wien). 2006. 148: 363-6
5. DiMaio S, Mohr G, Dufour JJ, Albrecht S. Distal mycotic aneurysm of the AICA mimicking intracanalicular acoustic neuroma. Can J Neurol Sci. 2003. 30: 388-92
6. Fujimura N, Abe T, Hirohata M, Morimitsu H, Tokutomi T, Shigemori M. Bilateral anomalous posterior inferior cerebellar artery-anterior inferior cerebellar artery anastomotic arteries associated with a ruptured cerebral aneurysm-case report. Neurol Med Chir (Tokyo). 2003. 43: 396-8
7. Fukushima S, Hirohata M, Okamoto Y, Yamashita S, Ishida S, Shigemori M. Anterior inferior cerebellar artery dissecting aneurysm in a juvenile. Case report. Neurol Med Chir (Tokyo). 2009. 49: 81-4
8. Fukushima Y, Enomoto T, Yoshino S, Yoshida K, Fukushima T, Hirakawa K. Coil embolization for a ruptured intrameatal aneurysm of the distal anterior inferior cerebellar artery with preservation of the parent artery. J Neuroendovasc Ther. 2014. 8: 146-51
9. Gleeson MJ, Cox TC, Strong AJ. Aneurysm of the anterior inferior cerebellar artery mimicking an intracanalicular acoustic neuroma. J Laryngol Otol. 1989. 103: 107-10
10. Gonzalez LF, Alexander MJ, McDougall CG, Spetzler RF. Anteroinferior cerebellar artery aneurysms: Surgical approaches and outcomes--a review of 34 cases. Neurosurgery. 2004. 55: 1025-35
11. Goto S, Ohshima T, Yamamoto T, Nishihori M, Nishizawa T, Shimato S. A case of ruptured intrameatal aneurysm successfully treated with coil embolization. Nagoya J Med Sci. 2015. 77: 307-13
12. Hancock JH, Miller JS. Spontaneous dissection of the anterior inferior cerebellar artery. Neuroradiology. 2000. 42: 535-8
13. Hori T, Hirakawa K, Ishijima B, Manaka S, Fukushima T. Aneurysm in the internal auditory meatus. Case report. J Neurosurg. 1971. 35: 605-9
14. Inoue Y, Morinaga K, Matsumoto Y, Ohmiya N, Mikami J, Matsuoka T. A case of ruptured internal auditory meatus aneurysm. Surg Cerebral Stroke. 1987. 15: 280-4
15. Kamano S, Kirino T, Mizuno S. Intrameatal aneurysm. Neurochirurgia (Stuttg). 1986. 29: 28-30
16. Kang HS, Roh HG, Han MH, Koh YC. Successful endovascular occlusion of a ruptured distal anterior inferior cerebellar artery aneurysm of the caudal trunk: Case report. Intervent Neuroradiol. 2007. 13: 271-6
17. Kim HC, Chang IB, Lee HK, Song JH. Ruptured total intrameatal anterior inferior cerebellar artery aneurysm. J Korean Neurosurg Soc. 2015. 58: 141-3
18. Kiya K, Uozumi T, Emoto K, Matsuoka T. Aneurysm of the anterior inferior cerebellar artery at the internal auditory meatus: Case report and review of the literature. Hiroshima J Med Sci. 1989. 38: 39-44
19. Lee SJ, Koh JS, Ryu CW, Lee SH. Ruptured intrameatal aneurysm of the anterior inferior cerebellar artery accompanying an arteriovenous malformation: A case report. Cerebellum. 2012. 11: 808-12
20. Liang B, Brammeier T, Huang J, Benardete EA. Plugged anterior inferior cerebellar artery aneurysm causing facial palsy, hearing loss, and subarachnoid hemorrhage treated by a translabyrinthine approach. Cureus. 2020. 12: e12282
21. Matsuyama T, Okuchi K, Norimoto K, Ueyama T. Ruptured dissecting anterior inferior cerebellar artery aneurysm. Case report. Meurol Med Chir (Tokyo). 2002. 42: 214-6
22. Michael E. Glasscock, III. Middle fossa approach to the temporal bone. Arch Otolaryng. 1969. 90: 41-53
23. Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, Tsuchida T. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 1995. 36: 905-11
24. Mizutani T. Natural course of intracranial arterial dissections. J Neurosurg. 2011. 114: 1037-44
25. Okumura Y, Sakaki T, Hirabayashi H, Shimomura T. Intrameatal aneurysm successfully treated by meatal loop trapping--case report. Neurol Med Chir (Tokyo). 1999. 39: 161-4
26. Peluso JP, van Rooij WJ, Sluzewski M, Beute GN. Distal aneurysms of cerebellar arteries: Incidence, clinical presentation, and outcome of endovascular parent vessel occlusion. AJNR Am J Neuroradiol. 2007. 28: 1573-8
27. Rodríguez-Hernández A, Rhoton AL, Lawton MT. Segmental anatomy of cerebellar arteries: A proposed nomenclature. Laboratory investigation. J Neurosurg. 2011. 115: 387-97
28. Saito A, Ezura M, Takahashi A, Yoshimoto T. An arterial dissection of the distal anterior inferior cerebellar artery treated by endovascular therapy. No Shinkei Geka. 2000. 28: 269-74
29. Santillan A, Gobin YP, Patsalides A, Riina HA, Rosengart A, Stieg PE. Endovascular management of distal anterior inferior cerebellar artery aneurysms: Report of two cases and review of the literature. Surg Neurol Int. 2011. 2: 95
30. Sasame J, Nomura M. Dissecting aneurysm of anterior inferior cerebellar artery initially presenting with nonhemorrhagic symptom. J Stroke Cerebrovasc Dis. 2015. 24: e197-9
31. Sato Y, Abe T, Suzuki Y, Katsuki M, Mashiyama S, Tominaga T. Parent artery occlusion against dissecting aneurysm involving the proximal anterior inferior cerebellar artery: Case report and literature review. NMC Case Rep J. 2020. 7: 81-4
32. Spallone A, De Santis S, Giuffrè R. Peripheral aneurysms of the anterior inferior cerebellar artery. Case report and review of literature. Br J Neurosurg. 1995. 9: 537-41
33. Sun Y, Wrede KH, Chen Z, Bao Y, Ling F. Ruptured intrameatal AICA aneurysms--a report of two cases and review of the literature. Acta Neurochir (Wien). 2009. 151: 1525-30
34. Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y. Trapping of ruptured dissecting aneurysm of distal anterior inferior cerebellar artery. Case report. Brain Nerve. 2009. 61: 203-7
35. Tamura Y, Shirai W, Tokumitsu N. Ruptured intrameatal aneurysm of the distal anterior inferior cerebellar artery: A case report. Jpn J Neurosurg (Tokyo). 2017. 26: 682-7
36. Tokimura H, Ishigami T, Yamahata H, Yonezawa H, Yokoyama S, Haruzono A. Clinical presentation and treatment of distal anterior inferior cerebellar artery aneurysms. Neurosurg Rev. 2012. 35: 497-503
37. Tokumitsu N, Sako K, Shirai W, Aizawa S. Anterior inferior cerebellar artery aneurysm at the internal auditory meatus: Report of 2 cases. Surg Cereb Stroke. 2004. 32: 61-5
38. Willms JF, Baltsavias G, Burkhardt JK, Ernst S, Tarnutzer AA. Missed anterior inferior cerebellar artery aneurysm mimicking vestibular neuritis-clues to prevent misdiagnosis. J Stroke Cerebrovasc Dis. 2016. 25: e231-2
39. Yamada M, Kitahara T, Kurata A, Fujii K, Miyasaka Y. Intracranial vertebral artery dissection with subarachnoid hemorrhage: Clinical characteristics and outcomes in conservatively treated patients. J Neurosurg. 2004. 101: 25-30
40. Yamakawa H, Hattori T, Tanigawara T, Sahashi Y, Ohkuma A. Intracanalicular aneurysm at the meatal loop of the distal anterior inferior cerebellar artery: A case report and review of the literature. Surg Neurol. 2004. 61: 82-8
41. Zager EL, Shaver EG, Hurst RW, Flamm ES. Distal anterior inferior cerebellar artery aneurysms. Report of four cases. J Neurosurg. 2002. 97: 692-6