- Operative Unit of Neurosurgery, San Salvatore Hospital, University of L’Aquila, L’Aquila, Italy
- Department of Pathology, San Salvatore Hospital, University of L’Aquila, L’Aquila, Italy
- MESVA Department, University of L’Aquila, L’Aquila, Italy
Correspondence Address:
Soheila Raysi Dehcordi
Operative Unit of Neurosurgery, San Salvatore Hospital, University of L’Aquila, L’Aquila, Italy
DOI:10.4103/2152-7806.188914
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Dehcordi SR, Ricci A, Chiominto A, Paulis DD, Vitantonio HD, Galzio RJ. Dorsal extradural meningioma: Case report and literature review. Surg Neurol Int 23-Aug-2016;7:76
How to cite this URL: Dehcordi SR, Ricci A, Chiominto A, Paulis DD, Vitantonio HD, Galzio RJ. Dorsal extradural meningioma: Case report and literature review. Surg Neurol Int 23-Aug-2016;7:76. Available from: http://surgicalneurologyint.com/surgicalint_articles/dorsal-extradural-meningioma-case-report-literature-review/
Abstract
Background:Extradural spinal mass lesions are most commonly metastatic tumors. Extradural meningiomas are rare, accounting for approximately 2.5–3.5% of spinal meningiomas; intraoperatively, they are easily mistaken for malignant tumors, especially in the en plaque variety, resulting in inadequate surgical treatment.
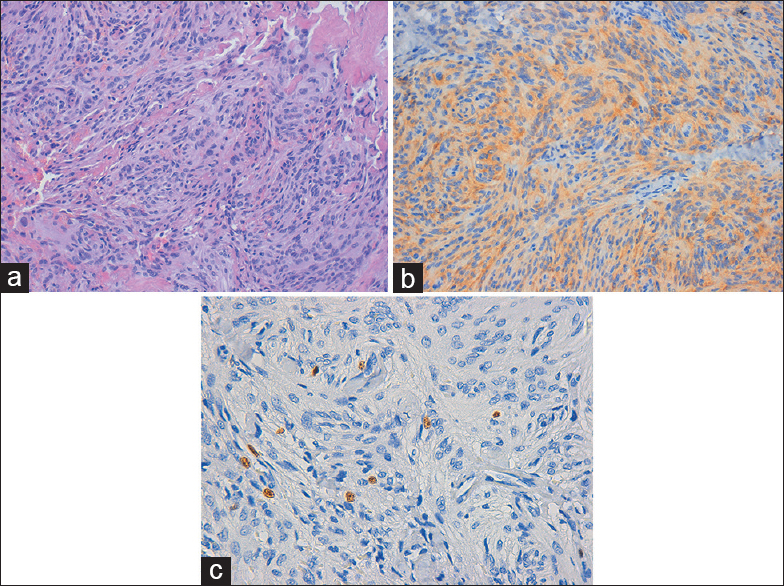
Case Description:Our case is one of the first to describe a patient with two purely extradural meningiomas, one each between D3–D4 and between D5–D6 vertebral levels. Surgical resection was radical, and pathologically both lesions were meningothelialmeningiomas.
Conclusions:Reviewing the literature, we discuss the pathogenesis, treatment strategies, and long-term behavior of these uncommon lesions.
Keywords: Extradural extramedullary neoplasms, extradural meningioma, extradural spinal tumors
INTRODUCTION
Vertebromedullary tumors are classified as either extradural or intradural. Intradural tumors are further divided into intramedullary or extramedullary. The most common intradural extramedullary neoplasms are schwannomas, neurofibromas, and meningiomas. Extradural tumors are most commonly metastatic lesions.[
Meningiomas account for 25–46% of primary spinal tumors,[
We report a rare case of two purely extradural thoracic spine meningiomas in a young woman suffering from meningiomatosis. We discuss the features and clinical management of entirely extradural meningiomas.
CASE REPORT
A 39-year-old woman, suffering from meningiomatosis, was operated in our institute several times. The first operation was performed in 2006, when she underwent exeresis of a paramedian meningioma (meningothelialmeningioma) arising in the right paramedian region. In 2009, she presented with a gran mal seizure and left hemiparesis; magnetic resonance imaging (MRI) revealed multicentric meningiomas in the right parietal paramedian and bilateral falcine regions. These lesions were partially removed and the postoperative course was good, with an improvement in her seizures and weakness. In addition, in this case, the histological diagnosis was meningothelialmeningioma. Therefore, after operation, the patient was subjected to radiotherapy and a close neuroradiologic follow-up. Since February 2015, she noted progressive numbness and weakness in both lower extremities with gait disturbance. She denied sphincter disturbance.
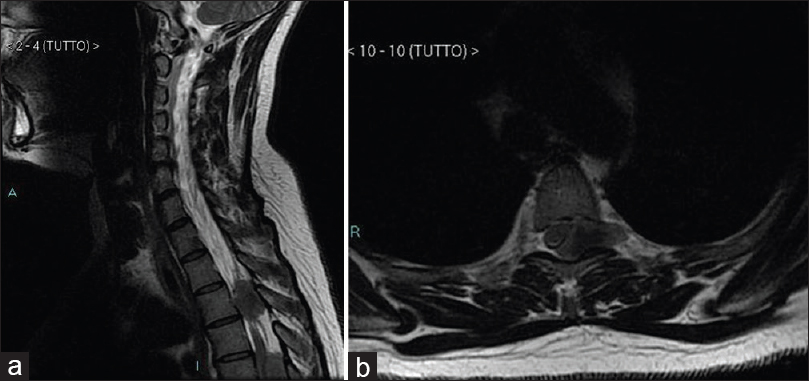
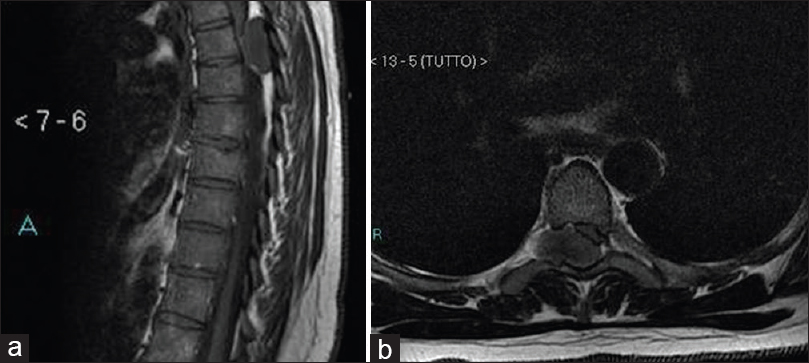
Spine magnetic resonance imaging (MRI) showed an extramedullary mass, located between D3–D4 vertebral levels, extending to the left D3–D4 foramen [
Neurological examination revealed a severe paraparesis with motor strength of 2/5 in both legs (left more than right) and a T6 sensory level bilaterally. A mild weakness in her arm was also noted (outcome of previous intervention). The following deep tendon reflexes were exaggerated: Bilateral knee jerk, bilateral ankle jerk, and bilateral medial hamstrings. Left-sided Babinski reflex was noted. General physical examination was normal.
Operation
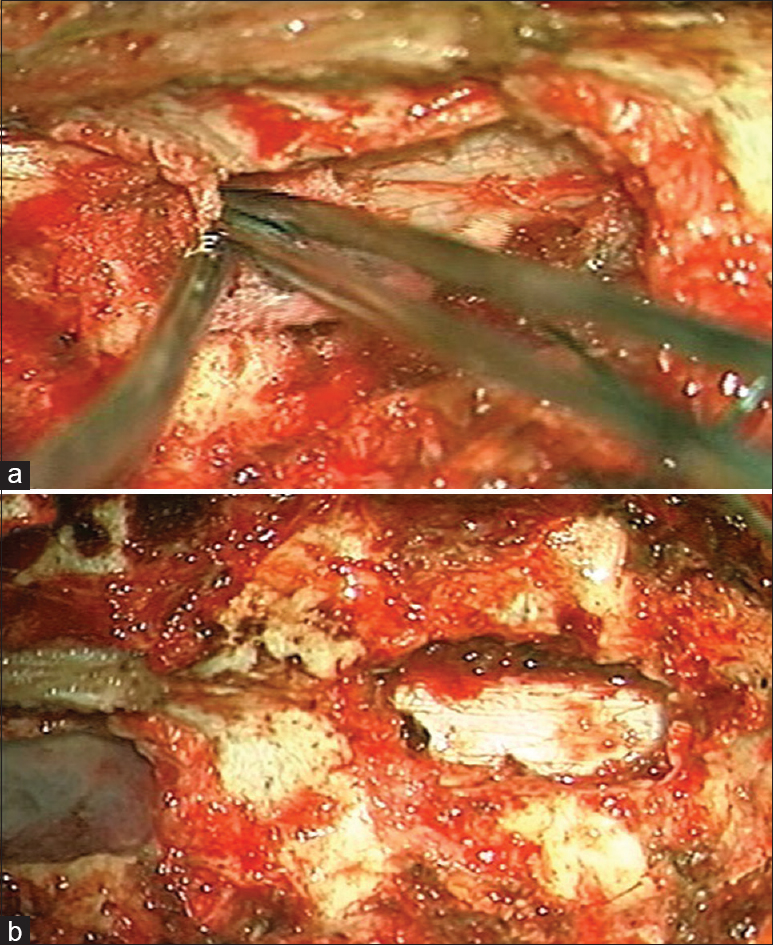
Using an operative microscope, the patient underwent a radical surgical excision of both lesions by D4 laminectomy and D5 left partial hemilaminectomy. Two purely extradural tumors were found intraoperatively; lesions were found to be gray, with hard consistency, along with calcifications and signs of bone erosion. Intraoperative findings were suggestive of a metastatic extradural and vertebral secondary location (even if no primary lesion was found in the preoperative laboratory and radiological evaluation). Extradural masses were completely removed and dural basements were cauterized [Figures
Postoperatively, there was a marked improvement in the muscle strength of the lower extremities; follow-up neuroimaging revealed complete removal of lesions and no spinal instability. No apparent tumor recurrence or regrowth was detected in a follow-up study 6 months later.
DISCUSSION
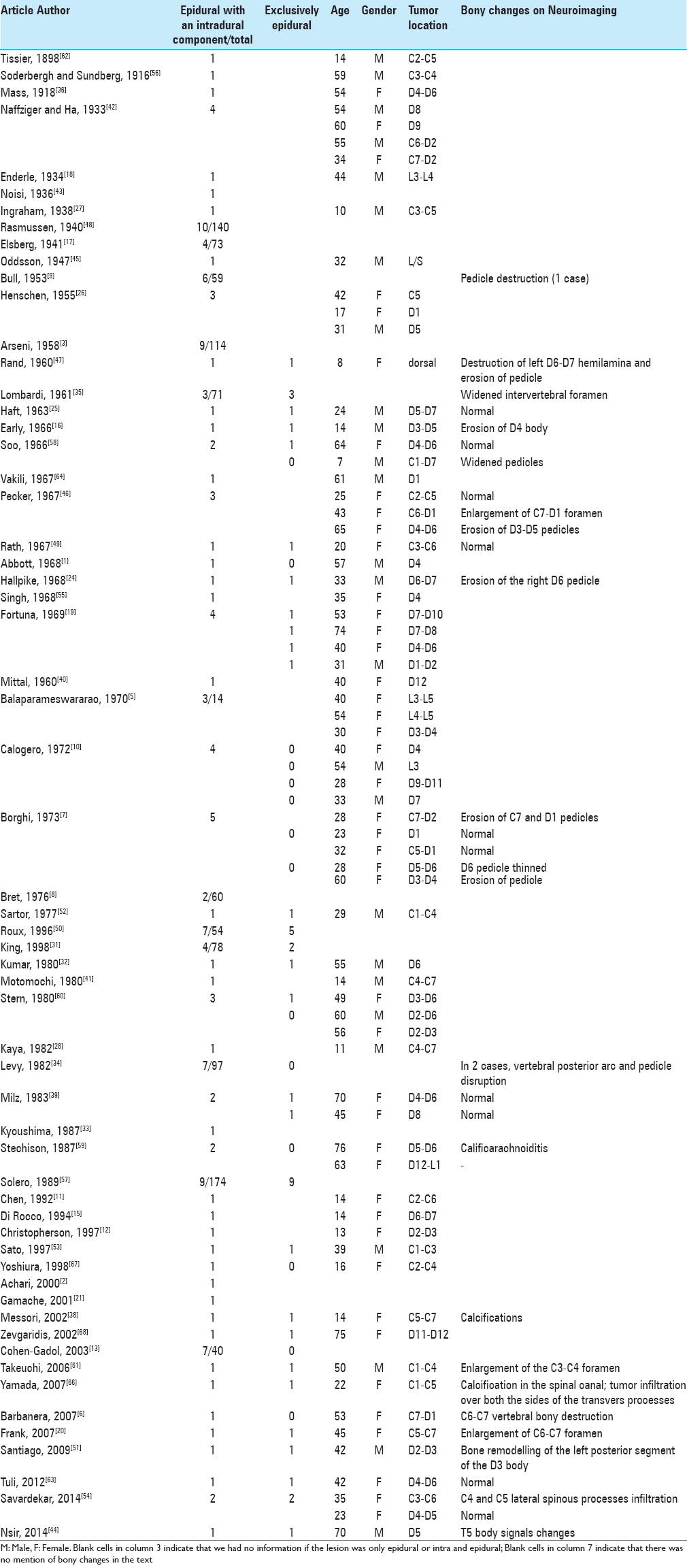
Exclusively extradural meningiomas are very rare, accounting for 2.5–3.5% of spinal meningiomas.[
Several theories have been postulated for the pathogenesis of purely extradural meningiomas. They are believed to arise from ectopic arachnoid cells around the periradicular nerve root sleeve, where the spinal meninx merges directly into the dura,[
Concerning neuroimaging, MRI is the technique of choice for the diagnosis of spinal meningiomas; it clearly defines the mass and its relation to the spinal cord.[
Various studies have provided contradicting reports for the long-term prognosis of patients with extradural spinal meningiomas. Some authors have asserted the aggressive behavior of these tumors, others have demonstrated these meningiomas to be benign.[
CONCLUSION
Purely extradural meningiomas are very infrequent but they should be included in the differential diagnosis of extradural lesions. They are easily mistaken pre and intraoperatively for metastatic tumors, with possible consequences on the proposed surgical treatment, and therefore, on the morbidity. Because prognosis is related to the extent of resection, we believe it would be better to completely remove the lesion, if considered safe. In case of doubts, an intraoperative pathology support could be useful. Finally, because of opposing views in the long-term prognosis and rate of surgical cure, it is very important to be aware of these lesions, undergoing patients to very close follow-ups.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abbott M, Killeffer FA, Crandall PH. Melanotic meningioma: Case report. J Neurosurg. 1968. 29: 283-6
2. Achari G, Behari S, Mishra A, Pandey R, Jain VK. Extradural meningioma en-plaque of the cervical cord. Neurol Res. 2000. 22: 351-3
3. Arseni MC, Ionesco S. Spinal cord compression caused by intraspinal tumors; clinico-statistical study of 362 cases. J Chir. 1958. 75: 582-94
4. Arslantas A, Artan S, Oner U, Durmaz R, Müslümanoglu H, Atasoy MA. Detection of chromosomal imbalances in spinal meningiomas by comparative genomic hybridization. Neurol Med Chir. 2003. 43: 12-9
5. Balaparameswararao S, Dinakar I, Srinivasarao K. Spinal epidural meningiomas. Neurol India. 1970. 18: 126-30
6. Barbanera A, Nina P, Serchi E, Ascanio F. Aggressive recurrence of intra-extradural cervico-thoracic meningothelial meningioma. Acta Neurochir. 2007. 149: 83-6
7. Borghi G. Extradural spinal meningiomas. Acta Neurochir. 1973. 29: 195-202
8. Bret P, Lecuire J, Lapras C, Deruty R, Dechaume JP, Assaad A. Intraspinal meningiomas. A series of 60 cases. Neurochirurgie. 1976. 22: 5-22
9. Bull JW. Spinal meningiomas and neurofibromas. Acta Radiol. 1953. 40: 283-300
10. Calogero JA, Moossy J. Extradural spinal meningiomas: Report of four cases. J Neurosurg. 1972. 37: 442-7
11. Chen HJ, Lui CC, Chen L. Spinal epidural meningioma in a child. Childs Nerv Syst. 1992. 8: 465-7
12. Christopherson LA, Finelli DA, Wyatt-Ashmead J, Likavec MJ. Ectopic extraspinal meningioma: CT and MR appearance. AJNR Am J Neuroradiol. 1997. 18: 1335-7
13. Cohen-Gadol AA, Zikel OM, Koch CA, Scheithauer BW, Krauss WE. Spinal meningiomas in patients younger than 50 years of age: A 21-year experience. J Neurosurg. 2003. 98: 258-63
14. Dagain A, Dulou R, Lahutte M, Dutertre G, Pouit B, Delmas JM. Extradural spinal meningioma: Case report. Neurochirurgie. 2009. 55: 565-8
15. Di Rocco C, Iannelli A, Colosimo C. Spinal epidural meningiomas in childhood: A case report. J Neurosurg Sci. 1994. 38: 251-4
16. Early CB, Sayers MP. Spinal epidural meningioma. Case report. J Neurosurg. 1966. 25: 571-3
17. Elsberg C.editorsSurgical Diseases of the Spinal Cord, Membranes and Nerve Roots. Symptoms, Diagnosis and Treatment. New York: P. B. Hoeber; 1941. p.
18. Enderle C. La diagnosi dei tumori extradurali del midollo spinale. Policlinico. 1934. 41: 483-9
19. Fortuna A, Gambacorta D, Occhipinti EM. Spinal extradural meningiomas. Neurochirurgia. 1969. 12: 166-80
20. Frank BL, Harrop JS, Hanna A, Ratliff J. Cervical Extradural Meningioma: Case Report and Literature Review. J Spinal Cord Med. 2008. 31: 302-5
21. Gamache FW, Wang JC, Deck M, Heise C. Unusual appearance of an en plaque meningioma of the cervical spinal canal. A case report and literature review. Spine. 2001. 26: E87-9
22. Gottfried ON, Gluf W, Hinojosa AQ, Kan P, Schmidt MH. Spinal meningiomas: Surgical management and outcome. Neurosurg Focus. 2003. 14: 1-7
23. Greenberg M.editorsSpine and spinal cord tumors. Handbook of neurosurgery. New York: Thieme; 2006. p. 507-
24. Hallpike JF, Stanley P. A case of extradural spinal meningioma. J Neurol Neurosurg Psychiat. 1968. 31: 195-7
25. Haft H, Shenkin HA. Spinal epidural meningioma: Case report. J Neurosurg. 1963. 20: 801-4
26. Henschen F.editorsTumoren des zentralnervensystems und seiner Hullen. Berlin: Springer Verlag; 1955. 13:
27. Ingraham F. Intraspinal tumors in infancy and childhood. Am J Surg. 1938. 39: 342-76
28. Kaya U, Ozden B, Turantan MI, Aydin Y, Barlas O. Spinal epidural meningioma in childhood: A case report. Neurosurgery. 1982. 10: 746-7
29. Klekamp J, Samii M. Surgical results for spinal meningiomas. Surg Neurol. 1999. 52: 552-62
30. Ketter R, Henn W, Niedermayer I, Steilen-Gimbel H, König J, Zang KD. Predictive value of progression-associated chromosomal aberrations for the prognosis of meningiomas: A retrospective study of 198 cases. J Neurosurg. 2001. 95: 601-7
31. King AT, Sharr MM, Gullan RW, Bartlett JR. Spinal meningiomas: A 20-year review. Br J Neurosurg. 1998. 12: 521-6
32. Kumar S, Kaza RC, Maitra TK, Chandra M. Extradural spinal meningioma arising from a nerve root: Case report. J Neurosurg. 1980. 52: 728-9
33. Kyoushima K, Nishiura I, Koyama T. Spinal epidural meningioma—A case report with special reference to neuroradiological findings. No Shinkei Geka. 1987. 15: 443-9
34. Levy W, Bay J, Dohn D. Spinal cord meningioma. J Neurosurg. 1982. 57: 804-12
35. Lombardi G, Passerini A. Spinal cord tumors. Radiology. 1961. 76: 381-92
36. Mass O. Bemerkenswerter Krankheitsverlauf bei Geschwulsten des Zentralnervensystems. Deutsch Z Nervenheilk. 1918. 59: 231-77
37. McPhee SJ, Papadakis MA, Tierney LM, Gonzales R, Zeiger R.editorsCurrent Medical Diagnosis & Treatment. New York: The McGraw-Hill Companies; 2007. p.
38. Messori A, Rychlicki F, Salvolini U. Spinal epidural enplaque meningioma with an unusual pattern of calcification in a 14-year-old girl: Case report and review of literature. Neuroradiology. 2002. 44: 256-60
39. Milz H, Hamer J. Extradural spinal meningiomas. Report of two cases. Neurochirurgia. 1983. 26: 126-9
40. Mittal MM, Gupta NC, Sharma ML. Spinal epidural meningioma associated with increased intracranial pressure. Neurology. 1970. 20: 818-20
41. Motomochi M, Makita Y, Nabeshima S, Aoyama I. Spinal epidural meningioma in childhood. Surg Neurol. 1980. 13: 5-7
42. Naffziger H, Ha B. Hour glass tumors of the spine. Arch Neurol Psychiat. 1933. 29: 561-84
43. Noisi F. Sopra due casi di tumore spinale. Minerva Med. 1936. 1: 513-23
44. Nsir AB, Boughamoura M, Mahnoudi H, Kilani M, Hattab N. Uncommon progression of an extradural spinal meningioma. Case Rep Surg 2014. 2014. p. 630876-
45. Oddsson B.editorsSpinal Meningioma. Copenhagen: Munksgaard; 1947. p.
46. Pecker MJ, Javalet A, Simon J, Loussouarn Y. Benign epidural tumors of the spinal cord. Neurochirurgie. 1967. 13: 647-60
47. Rand R, Rand C.editorsIntraspinal Tumors of Childhood. Springfield: Charles C Thomas; 1960. p.
48. Rasmussen TB, Kernohan JW, Adson AW. Pathologic classification, with surgical consideration, of intraspinal tumors. Ann Surg. 1940. 111: 513-30
49. Rath S, Mathai KV, Chandy J. Multiple meningiomas of the spinal canal. Case report. J Neurosurg. 1967. 26: 639-40
50. Roux FX, Nataf F, Pinaudeau M, Borne G, Devaux B, Meder JF. Intraspinal meningiomas: Review of 54 cases with discussion of poor prognosis factors and modern therapeutic management. Surg Neurol. 1996. 46: 458-63
51. Santiago BM, Rodeia P, Cunha E Sa M. Extradural thoracic spinal meningioma. Neurol India. 2009. 57: 98-
52. Sartor K, Fliedner E, Pfingst E. Angiographic demonstration of cervical extradural meningioma. Neuroradiology. 1977. 14: 147-9
53. Sato N, Sze G. Extradural spinal meningioma: MRI. Neuroradiology. 1997. p. 39,450-2
54. Savardekar A, Chatterjee D, Chatterjee D, Dhandapani S, Mohindra S, Salunke P. Totally extradural spinal en plaque meningiomas-Diagnostic dilemmas and treatment strategies. Surg Neurol Int. 2014. 5: 291-4
55. Singh R, Coerkamp G, Luyendijk W. Spinal epidural meningiomas. Acta Neurochir. 1968. 18: 237-45
56. Soderbergh G, Sundberg C. Atrophy of the small muscle of the hand through compression of upper cervical cord. Hygiea. 1916. 78: 417-36
57. Solero CL, Fornari M, Giombini S, Lasio G, Oliveri G, Cimino C. Spinal meningiomas: Review of 174 operated cases. Neurosurgery. 1989. 25: 153-60
58. Soo LY. Spinal epidural meningioma. South Med J. 1966. 59: 141-4
59. Stechison MT, Tasker RR, Wortzman G. Spinal meningioma en plaque. Report of two cases. J Neurosurg. 1987. 67: 452-5
60. Stern J, Whelan MA, Correll JW. Spinal extradural meningiomas. Surg Neurol. 1980. 14: 155-9
61. Takeuchi H, Kubota T, Sato K, Hirose S. Cervical extradural meningioma with rapidly progressive myelopathy. J Clin Neurosci. 2006. 13: 397-400
62. Tissier H. Compression lente de la moelle. Bull Soc Anat Paris. 1898. 73: 304-8
63. Tuli J, Drzymalski DM, Lidov H, Tuli S. Extradural En-Plaque Spinal Meningioma with Intraneural Invasion. World Neurosurg. 2012. 77: e5-13
64. Vakili H.editorsThe Spinal Cord. New York: International Medical Book Co; 1967. p.
65. Vargas MI, Abu Eid M, Bogorin A, Beltechi R, Boyer P, Javier RM. Spinal extradural meningiomas: MRI findings in two cases. J Neuroradiol. 2004. 31: 214-9
66. Yamada S, Kawai S, Yonezawa T, Masui K, Nishi N, Fujiwara K. Cervical extradural en-plaque meningioma. Neurol Med Chir. 2007. 47: 36-9
67. Yoshiura T, Shrier DA, Pilcher WH, Rubio A. Cervical spinal meningioma with unusual MR contrast enhancement. AJNR Am J Neuroradiol. 1998. 19: 1040-2
68. Zevgaridis D, Thomé C. Purely epidural spinal meningioma mimicking metastatic tumor: Case report and review of literature. Spine. 2002. 27: E403-5