- Department of Neurosurgery, Brain Research Institute, University of Niigata, Niigata, Japan
Correspondence Address:
Masafumi Fukuda
Department of Neurosurgery, Brain Research Institute, University of Niigata, Niigata, Japan
DOI:10.4103/2152-7806.162483
Copyright: © 2015 Fukuda M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Fukuda M, Saito A, Takao T, Hiraishi T, Yajima N, Fujii Y. Drainage patterns of the superficial middle cerebral vein: Effects on perioperative managements of petroclival meningioma. Surg Neurol Int 07-Aug-2015;6:130
How to cite this URL: Fukuda M, Saito A, Takao T, Hiraishi T, Yajima N, Fujii Y. Drainage patterns of the superficial middle cerebral vein: Effects on perioperative managements of petroclival meningioma. Surg Neurol Int 07-Aug-2015;6:130. Available from: http://surgicalneurologyint.com/surgicalint_articles/drainage-patterns-of-the-superficial-middle-cerebral-vein-effects/
Abstract
Background:Although the superficial middle cerebral vein (SMCV) usually connects with the cavernous sinus, there are several anatomical variations. We determined whether differences in SMCV drainages patterns affected the perioperative management of petroclival meningioma.
Methods:The subjects included 17 patients (4 men; 13 women) who underwent resection of a petroclival meningioma. SMCV drainage patterns were classified into four groups according to angiographic findings: (1) The SMCV connected with the cavernous sinus (Group A); (2) The SMCV was either absent or connected directly with the superior sagittal or transverse sinus through the cortical veins (Group B); (3) The SMCV turned downward and connected with the pterygoid plexus through the sphenobasal vein (SpBV, Group C); and (4) The SMCV ran across the bottom of the middle fossa and connected with transverse sinus via the sphenopetrosal sinus (SpPS, Group D).
Results:In all 9 patients in Group A, the SMCV drainage pattern did not affect any aspect of perioperative management. In contrast, SMCV drainage patterns in 3 of 4 patients in Group B and both patients in Groups C and D had an effect on perioperative management, indicating a significant impact of variations in SMCV drainage patterns (P
Conclusions:In cases, where the SMCV directly connects with superior sagittal or transverse sinus, SpBV or SpPS, surgeons have to meticulously select a safe and effective approach and take measures to preserve the SpBV or SpPS during surgery.
Keywords: Petroclival meningioma, petrosal approach, sphenobasal vein, sphenopetrosal sinus, superficial middle cerebral vein
INTRODUCTION
The superficial middle cerebral vein (SMCV) typically either connects with the proximal sphenoparietal sinus and then flows into the cavernous sinus or directly drains into the cavernous sinus.[
A transpetrosal approach has been widely used in surgical treatment for petroclival meningioma. A key procedure of this operation is cutting the cerebellar tentorium and dura along the bottom of the middle fossa to create a wide exposure of both supra- and infra-tentorial regions. In a patient with an SMCV connection to the SpPS, incision of the tentorium is likely to disturb the SpPS drainage from the temporal lobe.[
PATIENTS AND METHODS
Patient population
The study included 17 patients (4 men, 13 women) with petroclival meningioma, who were treated surgically at the University of Niigata during a period, from November 2005 to December 2013. Clinical data for patients are outlined in
Superficial middle cerebral vein drainage patterns
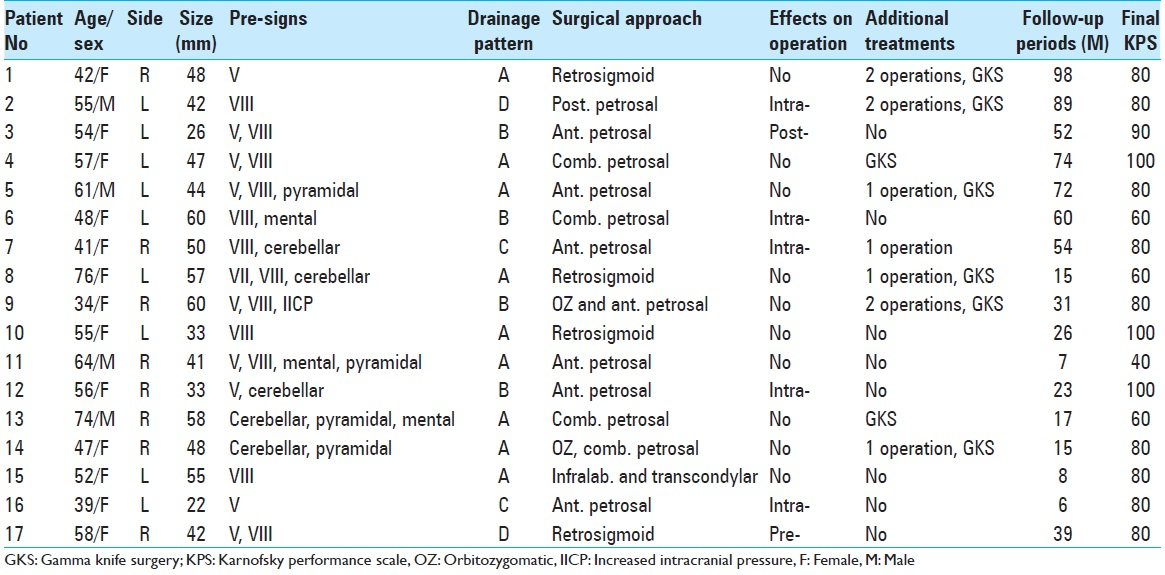
Conventional angiography was performed in all patients. SMCV drainage patterns were classified into four groups according to these angiographic findings [
Figure 1
Examples of the four types of superficial middle cerebral vein drainage patterns. (a) Carotid angiogram in venous phase showing the superficial middle cerebral vein draining into the cavernous sinus (arrow). (b) Image of a superficial middle cerebral vein connecting with the superior sagittal sinus via the cortical bridging vein (arrow). (c) Image of a superficial middle cerebral vein turning downward and connecting with the pterygoid plexus via the sphenobasal vein (arrow). (d) Image of a superficial middle cerebral vein running across the bottom of the middle fossa and connecting with the transverse sinus via the sphenopetrosal sinus (arrow)
Surgical procedures
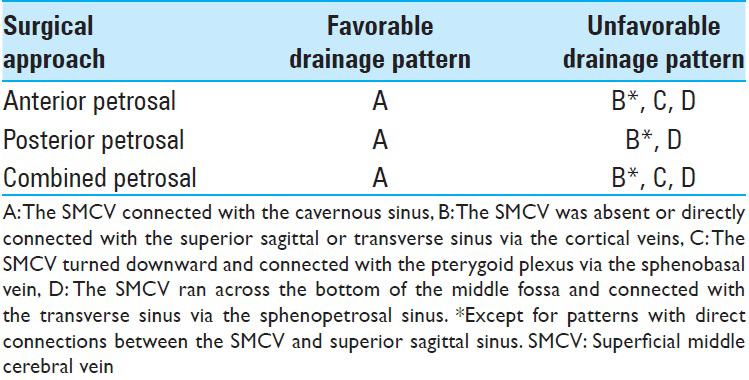
Based on the tumor location and size, SMCV drainage patterns, and preoperative symptoms, a range of surgical approaches were considered for each patient [
Evaluations
We retrospectively determined whether SMCV drainage patterns (four groups) affected perioperative management based on each patient's medical records. Perioperative management comprised preoperative selection of the surgical approach, limitations of surgical fields or changes in surgical manipulation to ensure preservation of the drainage veins during surgery, unusual venous bleeding intraoperatively, and unpredictable postoperative events that were likely attributable to injury to drainage veins of the SMCV. For statistical analysis, a χ2 test and Fisher's exact probability test were used. A P < 0.05 was defined as significant.
RESULTS
Surgical results
Total tumor removal was achieved in only 1 of 17 patients [Patient 3 in
Effects of superficial middle cerebral vein drainage patterns on perioperative managements
In all 9 patients assigned into Group A, the SMCV drainage patterns did not affect any aspects of perioperative management. In contrast, SMCV drainage patterns affected perioperative management in 3 of 4 patients in Group B and all patients in Groups C and D indicating a significant effect of SMCV drainage patterns (P < 0.005). In total, no patients in Group A versus 7 of 8 patients (87.5%) in the other groups had at least one adverse event or surgical complication during perioperative management (P < 0.001).
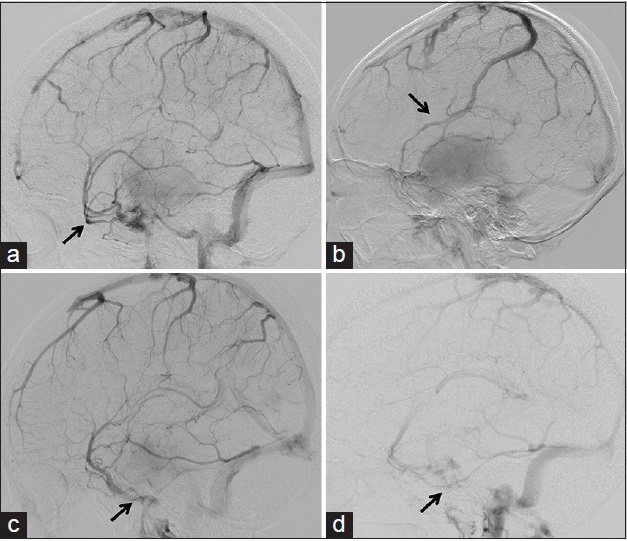
In Group B, Patient 3 [
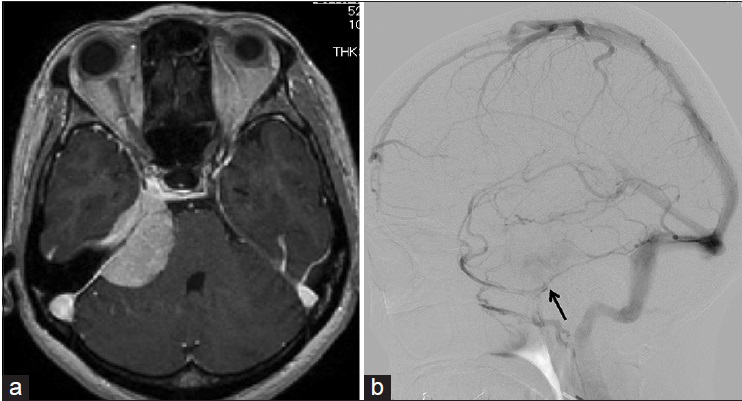
Figure 2
Example of a case in which the superficial middle cerebral vein was absent. (a) T1-weighted magnetic resonance imaging with contrast medium showing a right petroclival meningioma (Patient 12). (b) Right carotid angiogram in the venous phase showing that the superficial middle cerebral vein is absent, and the basal vein runs into the cerebellar tent and connects with the transverse sinus (arrow). (c) The Rosenthal basal vein (blue arrow) running into the cerebellar tent is visualized. (d) Tentorium incision with preservation the basal vein exposed the tumor and trochlear nerve (blue arrow)
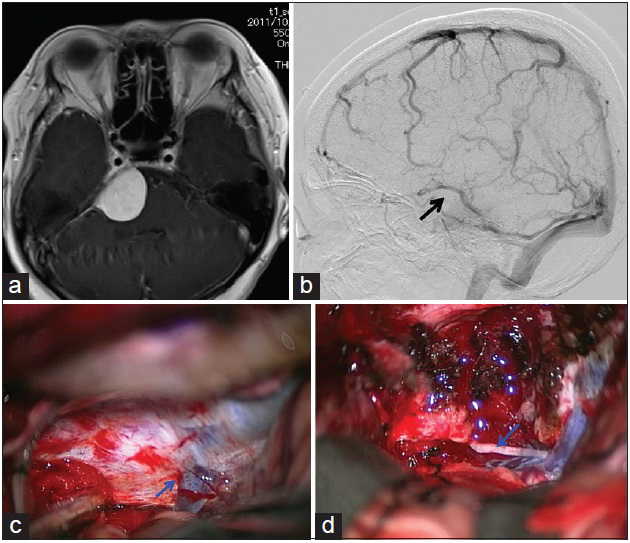
In both patients assigned to Group C (Patients 7 and 16), we were unable to attain a wider operative field and required access via drilling the petrous bone, because an epidural approach was not used around the foramen ovale due to the presence of a SpBV connection. In Patient 7, in particular, it was difficult to arrest venous bleeding around the foramen ovale due to the SpBV connection [Figure
Figure 3
Example of a superficial middle cerebral vein connecting to the sphenobasal vein. (a) T1-weighted magnetic resonance imaging with contrast medium showing a left petrocalival meningioma (Patient 7). (b) Left carotid angiogram in venous phase showing the superficial middle cerebral vein connecting with the pterygoid venous plexus via the sphenobasal vein (arrow)
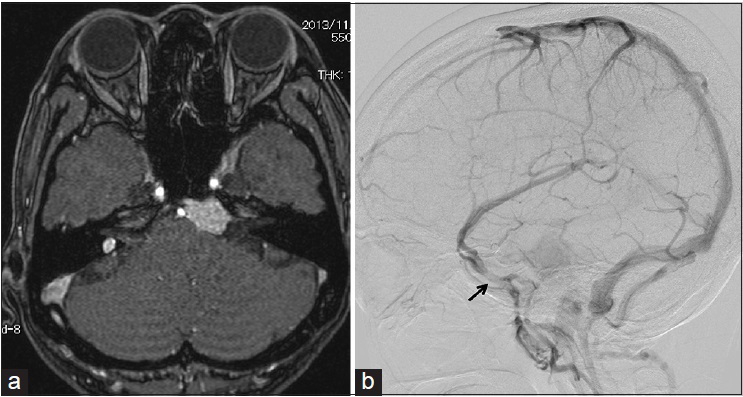
In Patient 2 in Group D, we attempted to remove the tumor through a posterior transpetrosal approach, but the operating field was too narrow as the middle fossa dura was not cut in order to preserve the SpPS. In the other Group D patient (Patient 17), we did not select an anterior transpetrosal approach because the SpPS was identified preoperatively [Figure
Figure 4
Example of a superficial middle cerebral vein connecting the sphenopetrosal sinus. (a) T1-weighted magnetic resonance imaging with contrast medium showing a right petrocalival meningioma (Patient 17). (b) Right carotid angiogram in venous phase showing the superficial middle cerebral vein connecting with the transverse sinus via the sphenopetrosal sinus (arrow)
DISCUSSION
In the present study, no petroclival meningioma cases in which the SMCV connected with the cavernous sinus manifested any complications of pre-, intra-, or post-operative management of surgical treatment. In contrast, the complications of perioperative management were almost always encountered for patients with a SpBV or SpPS connection, or an SMCV that directly connected with either the superior sagittal or transverse sinus. In patients with these latter patterns, the surgical procedure was complicated by the need to meticulously select an appropriate approach for removal of the petroclival meningioma that preserved the SpBV or SpPS.
Patients in whom the SMCV directly connected with the superior sagittal sinus via the cortical vein seemed to have the advantage of it being relatively simple to preserve venous drainage of the temporal lobe using an anterior or posterior transpetrosal approach. Patient 9 provides an example of this drainage pattern, and there were no problems encountered with venous drainage in the temporal lobe during surgery. In contrast, preventing bleeding during operations in which there was an unusual SMCV venous pattern was challenging. Indicating that this is a fairly common clinical issue, a study that classified SMCV variations using 3DCT reported a 9% incidence of undeveloped SMCV,[
Although the basal veins flowed into the great vein of Galen in most cases, these veins rarely course along the medial edge, center, or lateral edge of the tentorium. However, basal vein drainage flow into medial or lateral tentorial sinus was observed in 5% of subjects in a 3DCT angiography study.[
The SpBV is the main drainage vessel of the SMCV in 11–18% of individuals.[
In 2–10% patients, a SpPV connection is present, in which case the SMCV runs across the bottom of the middle fossa and connects with transverse sinus via the SpPS.[
Based on the results, there likely are disadvantages in an anterior petrosal approach for patients in Groups B, C, and D. For patients in Groups B and D, a posterior petrosal approach likely has disadvantages, as well [
CONCLUSIONS
Except for patients in whom the SMCV connects with the cavernous sinus, venous drainage patterns of the temporal lobe likely lead to more complicated pre-, intra-, and post-operative management of surgical treatments for petroclival meningioma. When a SpBV connection is present, surgeons should consider strategies that do not injure the vein around to the foramen ovale during an anterior petrosal approach. In cases, in which a SpPS connection is present, a tentorial incision that preserves venous drainage and a transpetrosal approach are needed.
References
1. Almefty R, Dunn IF, Pravdenkova S, Abolfotoh M, Al-Mefty O. True petroclival meningiomas: Results of surgical management. J Neurosurg. 2014. 120: 40-51
2. Hacker H, Newton TH, Potts DG.editors. Normal supratentorial veins and dural sinsus. Radiology of the Skull and Brain: Angiography. Saint Louis: CV Mosby; 1974. p. 1851-77
3. Hayashi N, Sato H, Tsuboi Y, Nagai S, Kuwayama N, Endo S. Consequences of preoperative evaluation of patterns of drainage of the cavernous sinus in patients treated using the anterior transpetrosal approach. Neurol Med Chir (Tokyo). 2010. 50: 373-7
4. Ichimura S, Yoshida K, Kagami H, Inaba M, Orii M, Kitamura Y. Epidural anterior petrosectomy with subdural visualization of sphenobasal vein via the anterior transpetrosal approach – Technical case report. Neurosurg Rev. 2012. 35: 609-13
5. Kaku S, Miyahara K, Fujitsu K, Hataoka S, Tanino S, Okada T. Drainage pathway of the superior petrosal vein evaluated by CT venography in petroclival meningioma surgery. J Neurol Surg B. 2012. 73: 316-20
6. Sakata K, Al-Mefty O, Yamamoto I. Venous consideration in petrosal approach: Microsurgical anatomy of the temporal bridging vein. Neurosurgery. 2000. 47: 153-60
7. Suzuki Y, Ikeda H, Shimadu M, Ikeda Y, Matsumoto K.editors. Variations of the basal vein: Identification using three-dimensional CT angiography. AJNR Am J Neuroradiol. 2001. 22: 670-6
8. Suzuki Y, Matsumoto K.editors. Variations of the superficial middle cerebral vein: Classification using three-dimensional CT angiography. AJNR Am J Neuroradiol. 2000. 21: 932-8
9. Tanoue S, Kiyosue H, Okahara M, Sagara Y, Hori Y, Kashiwagi J. Para-cavernous sinus venous structures: Anatomic variations and pathologic conditions evaluated on fat-suppressed 3D fast gradient-echo MR images. AJNR Am J Neuroradiol. 2006. 27: 1083-9
10. Yamakami I, Hirai S, Yamaura A, Ono J. Venous system playing a key role in transpetrosal approach. No Shinkei Geka. 1998. 26: 699-707