- Department of Neurosurgery, National Hospital Organization Himeji Medical Center, Himeji, Hyogo, Japan
Correspondence Address:
Masaomi Koyanagi
Department of Neurosurgery, National Hospital Organization Himeji Medical Center, Himeji, Hyogo, Japan
DOI:10.4103/2152-7806.196371
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masaomi Koyanagi, Tamaki Kobayashi, Masashi Oda, Osamu Narumi. Dural arteriovenous fistula in the falx cerebri treated with transarterial embolization using n-butyl cyanoacrylate. 21-Dec-2016;7:
How to cite this URL: Masaomi Koyanagi, Tamaki Kobayashi, Masashi Oda, Osamu Narumi. Dural arteriovenous fistula in the falx cerebri treated with transarterial embolization using n-butyl cyanoacrylate. 21-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/dural-arteriovenous-fistula-in-the-falx-cerebri-treated-with-transarterial-embolization-using-n%e2%80%91butyl-cyanoacrylate/
Abstract
Background:A dural arteriovenous fistula in the falx cerebri is a relatively rare lesion, with only two cases reported till date. One was treated with direct surgery, and the other was followed-up conservatively. Advances in catheter design and embolic materials have made safe and curative transarterial embolization of dural arteriovenous fistulas possible in the current era.
Case Description:We describe a 67-year-old man with left putaminal hemorrhage who was diagnosed with an arteriovenous fistula in the anterior part of the falx cerebri that was treated with curative transarterial glue embolization through the middle meningeal artery by using n-butyl cyanoacrylate.
Conclusion:Although the procedure was safely performed, understanding the potential risks of the migration of embolic materials into the ophthalmic and anterior cerebral artery system is mandatory.
Keywords: Dural arteriovenous fistula, embolization, falx cerebri, meningeal arteries
INTRODUCTION
Intracranial dural arteriovenous fistulas (AVFs) are often located in the cavernous and transverse-sigmoid sinuses, however, relatively rarely in the falx cerebri. To our knowledge, only two cases of dural AVFs in the falx cerebri have been reported till date.[
Transarterial embolization with the endovascular technique is often considered the first-line treatment for dural AVFs. Liquid embolic agents including n-butyl cyanoacrylate (n-BCA; Codman, Raynham, Massachusetts, USA) and ethylene vinyl alcohol copolymer (ONYX; ev3, Irvine, California, USA) are the main tools for this transarterial treatment. Although a recent study suggested a lower recurrence rate of dural AVFs treated with Onyx, n-BCA is still valuable because of its long-term efficacy and lower complication rate.[
CASE REPORT
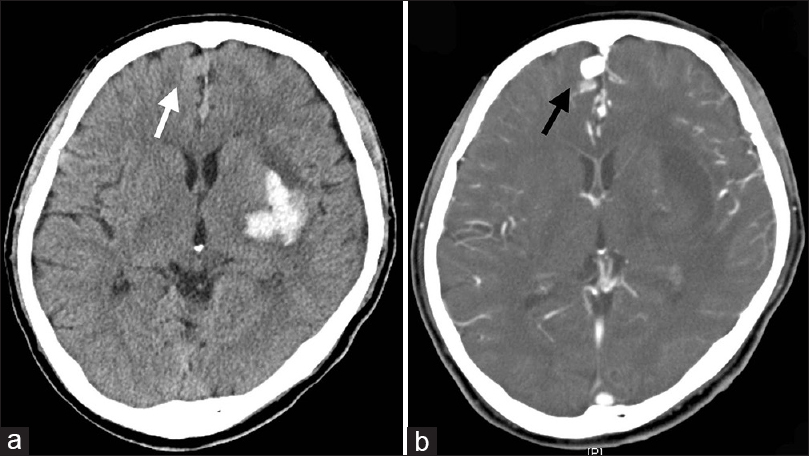
A 67-year-old man without a history of head trauma and neurosurgical procedures was transferred to our hospital when he presented with the sudden onset of right hemiparesis and speech disturbance. On computed tomography, a left putaminal hematoma and smooth round masses in the anterior part of the interhemispheric fissure were found [
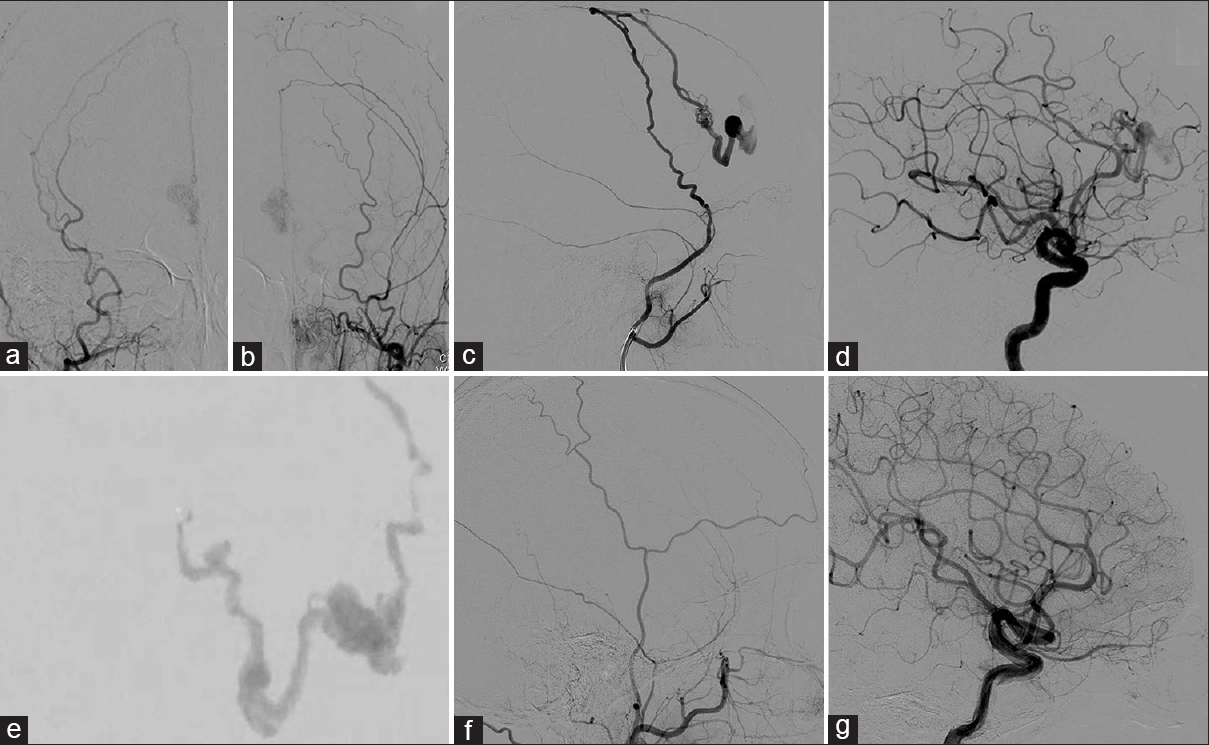
Selective angiography revealed an AV shunt located in the falx cerebri that was supplied by the anterior branch of the bilateral middle meningeal artery [Figure
Figure 2
(a, b) Anteroposterior views of right (a) and left (b) external carotid arteries showing an arteriovenous fistula fed with bilateral middle meningeal arteries. (c, d): Lateral views of the right external (c) and internal carotid (d) arteries showing an arteriovenous fistula in the falx cerebri. (e) Image showing embolization of the shunt performed with a mixture of 12.5% n-butyl cyanoacrylate and lipiodol. (f, g): Lateral views of the right external (f) and internal (g) carotid arteries on 3-month control angiography showing a complete obliteration of the arteriovenous fistula
Because we considered the shunt point as technically accessible through the middle meningeal artery, transarterial embolization was performed under general anesthesia. A marathon microcatheter (ev3) was used to superselectively catheterize the right middle meningeal artery to achieve wedge catheterization. Warmed, highly diluted glue (12.5% n-BCA diluted using ethiodized oil) was injected to fill the shunt, with penetration into the pathological venous segment including the venous ectasia [
The final angiography during the procedure showed almost complete occlusion of the shunt. The patient was discharged without any additional neurological deficits 3 days after the procedure. Control digital subtraction angiography performed 3 months after the operation revealed complete occlusion of the AVF [Figure
DISCUSSION
Dural AVFs in the falx cerebri are relatively rare. Herein, we present a case of dural AVF in the falx cerebri that was treated with transarterial embolization using n-BCA. The arterial supply of the anterior part of the falx cerebri derives from the middle meningeal artery, anterior falcine artery from the ophthalmic artery system, and dural branch of the anterior cerebral arteries.[
Various treatment options are available for treating AVFs; however, we favored the transarterial access for treatment in our case. A few key techniques exist for safe and curative transarterial embolization with n-BCA. The first involves obtaining the wedged position. The wedged position provides the ideal flow-arrest state for controlled delivery of embolic agents through the AVF toward the venous side to occlude the AV shunt.[
Open surgical disconnection of the fistulas is another treatment option. Some patients with dural AVFs were eventually cured by surgical disconnection. Nonetheless, surgery does carry risks and the inconvenience inherent to craniotomy. Transarterial embolization could be performed safely as we have shown. However, because the dural AVF in the anterior part of falx cerebri has a potential risk of occluding the ophthalmic and pericallosal artery systems during the transarterial embolization as described above, the knowledge of angioarchitecture, experience of handling embolic materials, and reliable techniques are mandatory.
To our knowledge, this is the first case report of a dural AVF in the falx cerebri treated with transarterial embolization using n-BCA. Transarterial embolization technique with n-BCA was found to be a good option for the treatment of this rare lesion.
CONCLUSION
Dural AVF in the falx cerebri could be safely managed with transarterial embolization. Understanding the angioarchitecture of the falx cerebri is mandatory. n-BCA is a valuable agent for endovascular treatment for dural AVFs; however, operator experience is essential.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Kakarla UK, Deshmukh VR, Zabramski JM, Albuquerque FC, McDougall CG, Spetzler RF. Surgical treatment of high-risk intracranial dural arteriovenous fistulae: Clinical outcomes and avoidance of complications. Neurosurgery. 2007. 61: 447-57
2. Kothbauer K, Huber P. Dural arteriovenous fistula in the falx cerebri. Neuroradiology. 1994. 36: 616-8
3. Lee SK, Hetts SW, Halbach V, terBrugge K, Ansari SA, Albani B. Standard and Guidelines: Intracranial Dural Arteriovenous Shunts. J Neurointerv Surg. 2015. p.
4. Martins C, Yasuda A, Campero A, Ulm AJ, Tanriover N, Rhoton AJ. Microsurgical anatomy of the dural arteries. Neurosurgery. 2005. 56: 211-51
5. Nelson PK, Russell SM, Woo HH, Alastra AJ, Vidovich DV. Use of a wedged microcatheter for curative transarterial embolization of complex intracranial dural arteriovenous fistulas: Indications, endovascular technique, and outcome in 21 patients. J Neurosurg. 2003. 98: 498-506
6. Ratliff J, Voorhies RM. Arteriovenous fistula with associated aneurysms coexisting with dural arteriovenous malformation of the anterior inferior falx. J Neurosurg. 1999. 91: 303-7