- Department of Neurosurgery, Ospedale Belcolle, Viterbo, Italy
- Department of Neurosurgery, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) San Gerardo dei Tintori, Monza, Italy
- Department of Neurosurgery, Azienda Ospedaliera Di Perugia, Perugia, Italy
- Department of Vascular and Interventional Radiology, Unit of Radiology, Ospedale Belcolle, Viterbo, Italy.
Correspondence Address:
Vittorio Ricciuti, Department of Neurosurgery, IRCCS San Gerardo dei Tintori, Monza, Italy.
DOI:10.25259/SNI_666_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Serena Pagano1, Vittorio Ricciuti2, Fabrizio Mancini3, Francesca Romana Barbieri1, Fabrizio Chegai4, Alessandra Marini3, Daniele Marruzzo1, Riccardo Paracino3, Riccardo Antonio Ricciuti1. Eagle syndrome: An updated review. 03-Nov-2023;14:389
How to cite this URL: Serena Pagano1, Vittorio Ricciuti2, Fabrizio Mancini3, Francesca Romana Barbieri1, Fabrizio Chegai4, Alessandra Marini3, Daniele Marruzzo1, Riccardo Paracino3, Riccardo Antonio Ricciuti1. Eagle syndrome: An updated review. 03-Nov-2023;14:389. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12622
Abstract
Background: This work aims to review the current literature and our experience on vascular Eagle syndrome (ES) that can present misleading clinical presentations and better understand the possible therapeutic strategies.
Methods: We reviewed the existing literature on PubMed from January 1, 2017, to December 31, 2022, including the sequential keywords “vascular AND Eagle syndrome,” “vascular AND styloid syndrome,” “vascular AND elongated styloid process,” “vascular AND stylocarotid syndrome,” and “Eagle syndrome AND carotid artery dissection.”
Results: 38 vascular ES cases, including our experience, were analyzed. The most frequent clinical onset was hemiparesis (n 21, 57%), but other regular clinical presentations were aphasia, loss of consciousness, amaurosis, headache, or a combination of the latter. Massive oral bleeding was reported only once in the literature before our case. Twelve patients were treated with only antiplatelet therapy, either single or double. Nine patients were treated with anticoagulation therapy only. In 14 patients, a carotid artery stent was used, associated with anticoagulation or antiplatelet therapy. In 17 cases, a styloid process (SP) resection was performed.
Conclusion: ES has many clinical presentations, and carotid artery dissection resulting in oral bleeding seems rare. Literature results and our experience make us believe that when dealing with vascular ES, the best treatment strategy is endovascular internal carotid artery stenting with antiplatelet therapy, followed by surgical removal of the elongated SP to prevent stent fracture.
Keywords: Eagle syndrome, Elongated styloid process, Internal carotid artery dissection, Stylocarotid syndrome, Vascular Eagle syndrome
INTRODUCTION
Eagle syndrome (ES) is a rare condition with different clinical presentations. First described by Eagle in 1937, it refers to various symptoms caused by the conflict of an elongated styloid process (ESP) – unilateral or bilateral – and/or calcified styloid ligament (CSL) with the surrounding anatomical structures. Originally, Eagle described this condition as a unilateral throat pain associated with the sensation of a foreign body in the throat.[
This review focused on the vascular form, a rare condition caused by the contact between ESP and/or CSL and the extracranial carotid artery. This conflict can lead to neurological symptoms (ischemia of downstream cerebral territories) due to compression, especially during rotational movement, or due to dissection and/or dissecting aneurysms of the carotid artery itself. We also present a case of a 48-year-old man without vascular risk factors contributing to mass oral bleeding and a later episode of transient dysarthria diagnosed with ES and treated with dual antiplatelet therapy (DAPT) therapy, endovascular flow-diverter (FD), and surgical SP removal. Since there is significant variability in clinical presentations and there is not a clear consensus on the management of this condition, we aim to summarize the current literature and to make a systematic review of cases of ES and CAD, considering articles from January 1, 2017, to December 31, 2022, expanding a previous study published in 2020 by Baldino et al.[
MATERIALS AND METHODS
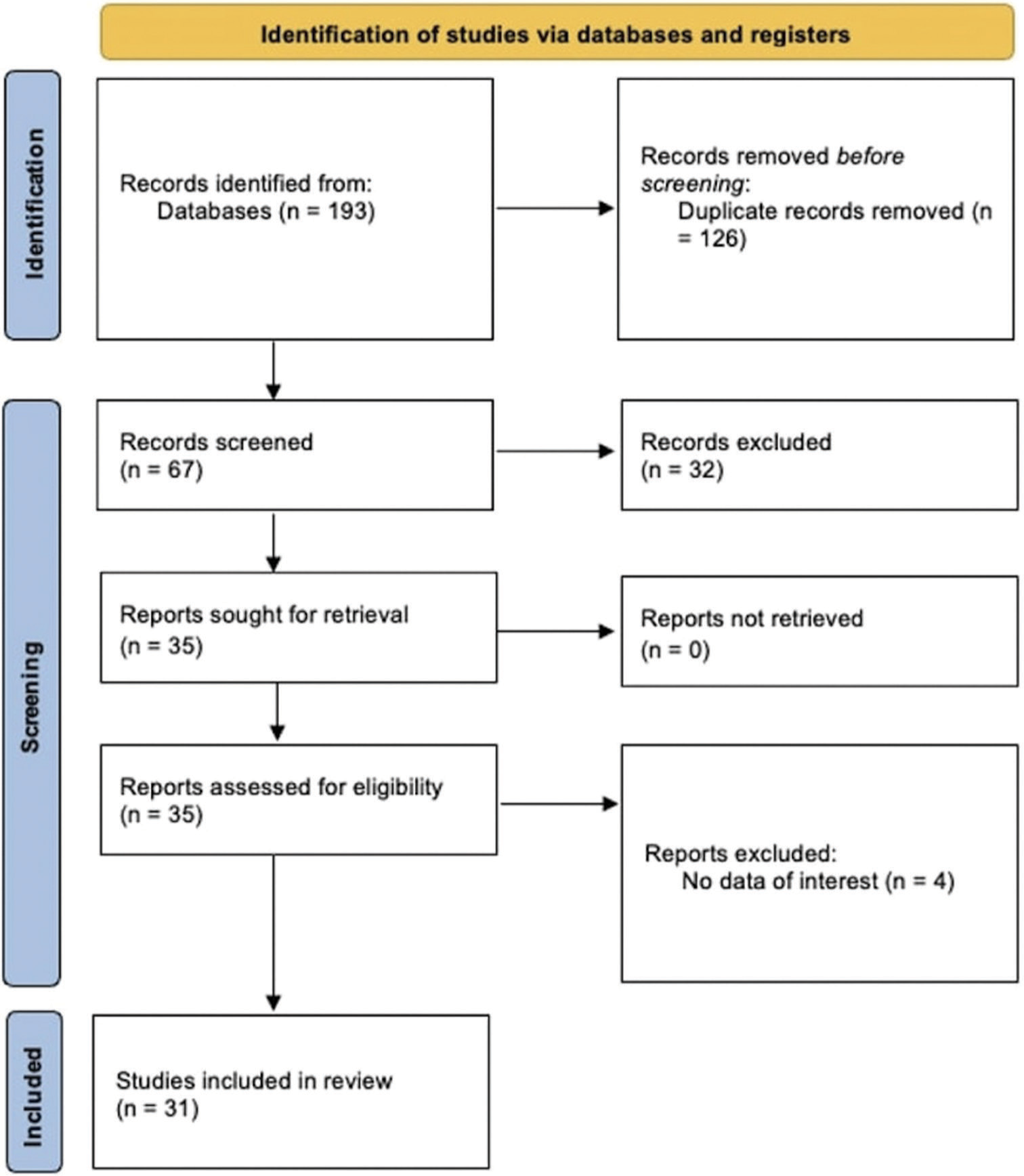
We reviewed the existing literature on PubMed from January 1, 2017, to December 31, 2022, without restrictions about the paper publication status, according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement.[
We researched PubMed for the literature regarding patients with an ESP and/or ligament calcification causing either cervical ICA dissection or cervical ICA dissecting aneurysms. The following sequential keywords were used: “vascular AND Eagle syndrome,” “vascular AND styloid syndrome,” “vascular AND elongated styloid process,” “vascular AND stylocarotid syndrome,” and “Eagle syndrome AND carotid artery dissection.”
Inclusion criteria included articles in English published between January 1, 2017, and December 31, 2022, and considering ES only associated with ICA dissection or dissecting aneurysms. Exclusion criteria were articles focused on ES presenting with clinical features other than ICA dissection, articles in different languages or only abstracts available, pure reviews (without new cases), or editorials.
We analyzed different features:
Population characteristics such as sex and age Symptoms of onset Laterality and length of ESPs Initial and eventual additional treatment Time of follow-up.
RESULTS
Through literature research on PubMed, between January 1, 2017, and December 31, 2022, 51 articles were found using the words “vascular AND Eagle syndrome, 48 articles using the words “vascular AND styloid syndrome,” 53 articles using the words “vascular AND elongated styloid process,” ten articles using the words “vascular AND stylocarotid syndrome,” and 31 articles using the words “Eagle syndrome AND carotid artery dissection.” Excluding repetitions, 67 original articles were screened through analysis of title and abstract. Thirty-two articles were then, excluded based on inclusion criteria cited before. A total of 35 articles were analyzed through full-text reading, and four more articles were excluded due to non-interesting data. In summary, 31 articles were used for this review [PRISMA graph in
This paper reports an additional case of CAD associated with an ESP, treated at Belcolle Hospital in Viterbo in September 2018.
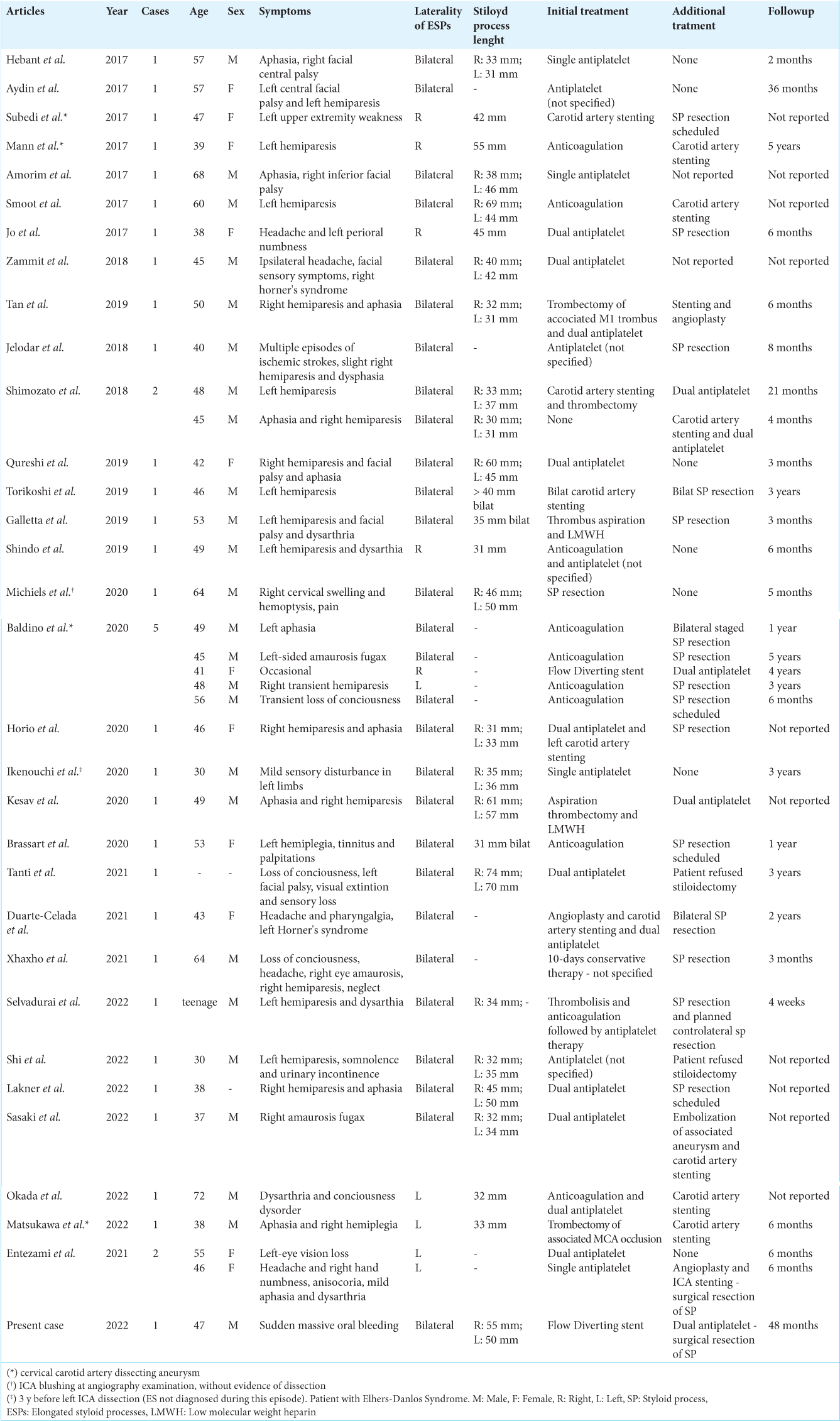
Our review of the literature shows that between 2017 and 2022, 37 cases of internal CAD have been caused by the vascular variant of ES. The demographic, clinical characteristics, treatment strategies, and follow-up of the patients are summarized in
The mean age of the patients was 48.2 years (range 30–72). In an article, one patient was described as a “teenager” but was not used for statistical evaluation. The prevalence was higher in men (n = 24, 69%) than in women (n = 11, 31%). In two cases, sex was not specified. In only one case, internal CAD was found occasionally, while an acute onset was described in all other cases. The most frequent clinical onset was hemiparesis (n = 21, 57%), but other frequent clinical presentations were aphasia, loss of consciousness, amaurosis, headache, or a combination of the latter. Bleeding from the oral cavity with hemoptysis was reported in only one case, resulting in a rare clinical presentation.
In the literature, there is a significant variability of treatment strategies. There is not a strong consensus on whether to prefer anticoagulation or antiplatelet therapy. In these cases, 12 patients were treated with only antiplatelet therapy, either single or double. Nine patients were treated with anticoagulation therapy only, with previous thrombus aspiration in two of these cases. In 14 patients, a carotid artery stent was used, associated with anticoagulation or antiplatelet therapy. In two cases, thrombectomy of MCA occlusion was necessary before stenting. In three cases, angioplasty was used before stenting. In 17 cases, a SP resection was performed. Only in one case, SP resection was used as the only treatment, while, in all other cases, it was used as a secondary procedure after the resolution of the CAD to eliminate the mechanical cause and prevent recurrence.
Clinical case
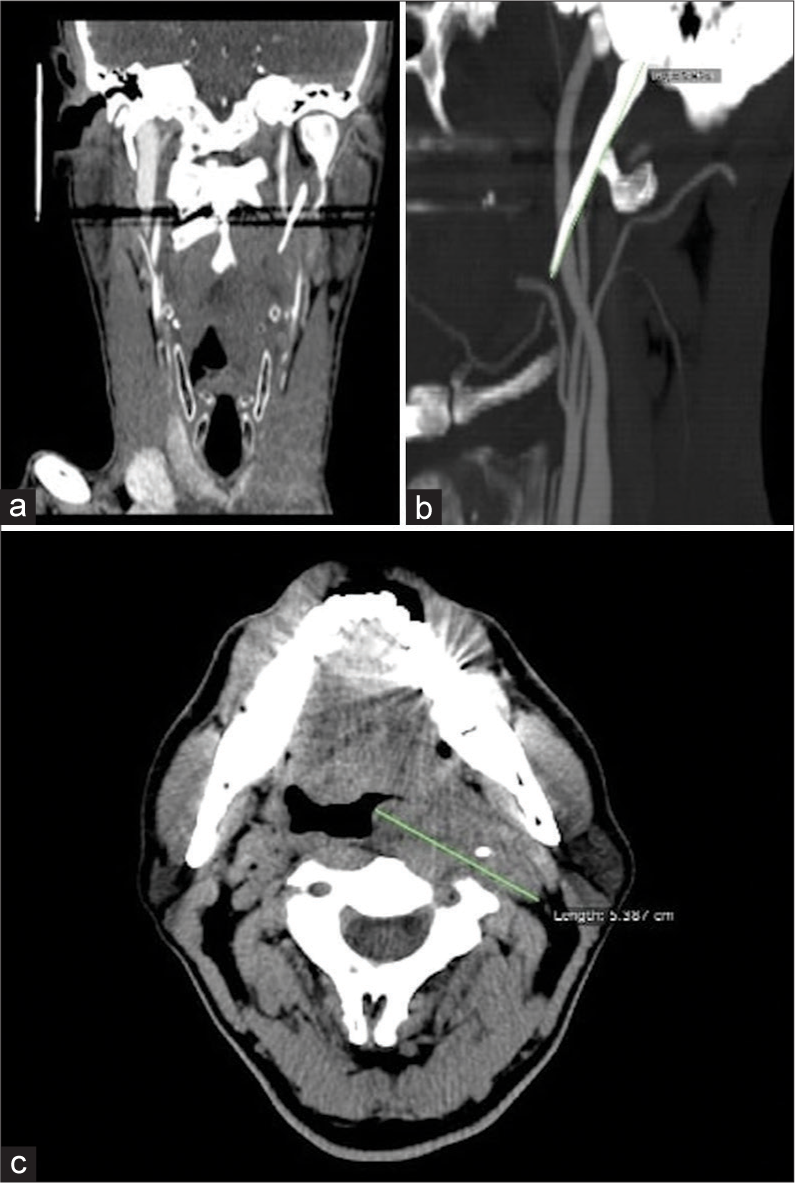
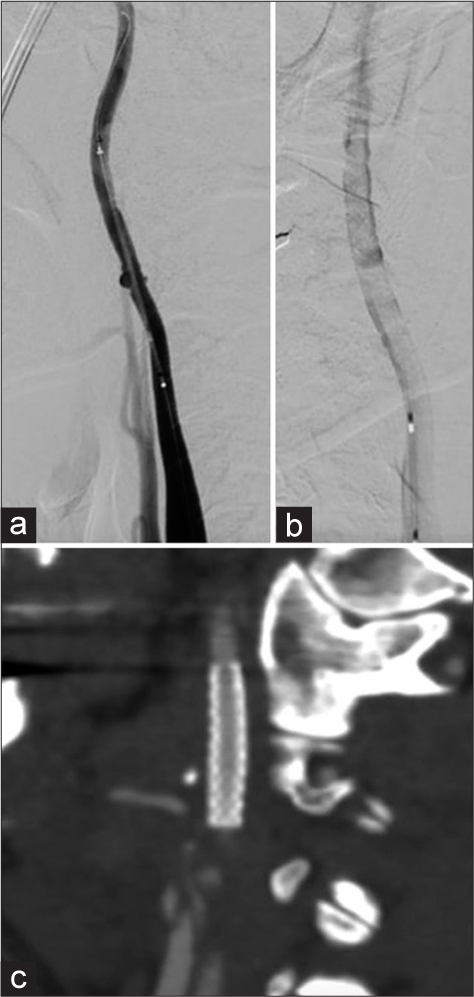
In September 2018, a 48-year-old man without any history of vascular and neurovascular risk factors was admitted to our Emergency Room due to a sudden massive oral bleeding and a slight spatial and temporal disorientation. Contrast enhancement computed tomography (CT) scan showed a large portion of hypodense tissue with poor enhancement in the left retropharyngeal space, with an axial diameter of about 5 × 3 cm [
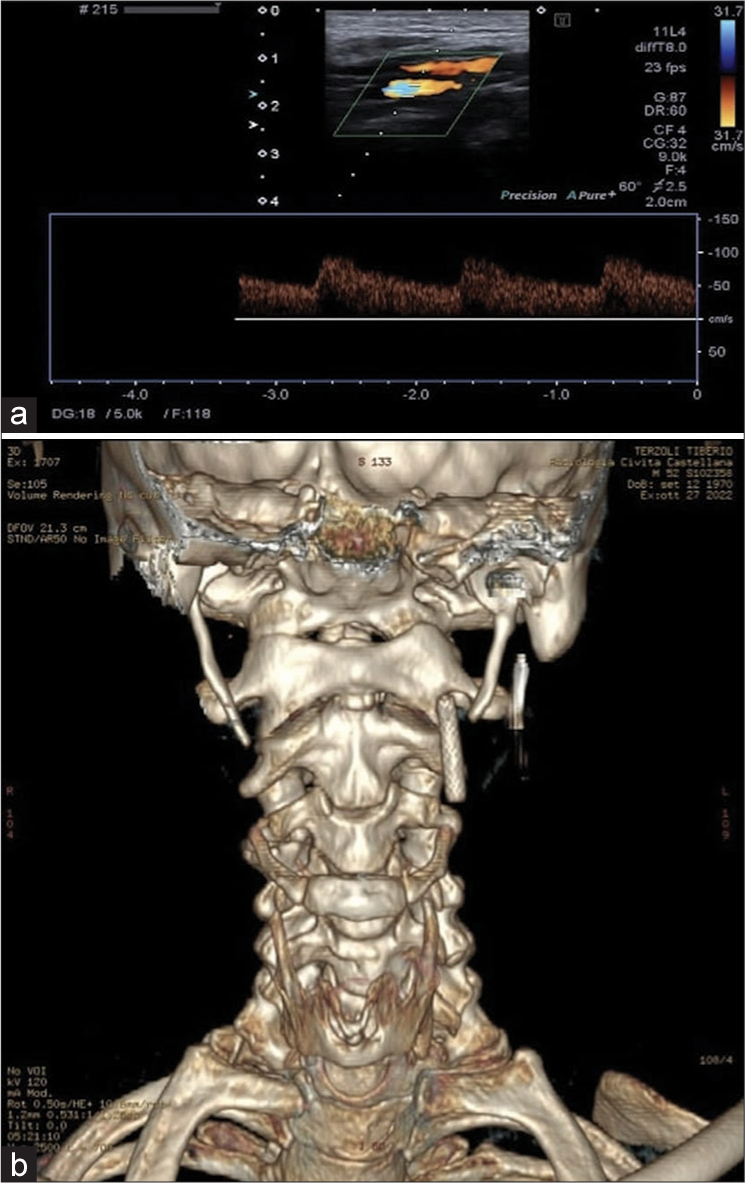
Figure 5:
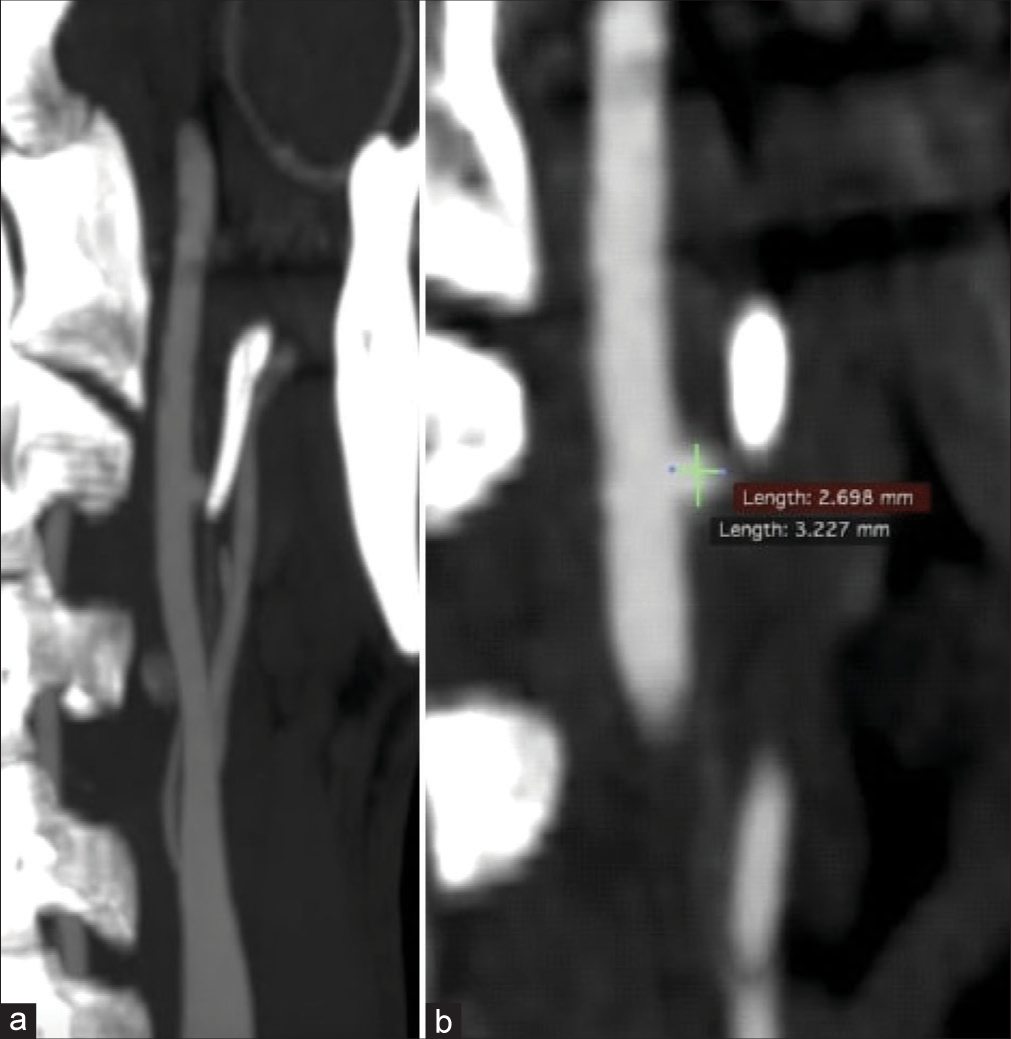
(a) The echo-color-Doppler examination of the left internal carotid artery documents the presence of the flow-diverter stent, which appears in the correct position and patent with an intra-stent sampled velocity index in range. (b) Postoperative 3D reconstruction computed tomography scan; reducing the styloid process length avoids impingement with the stent.
DISCUSSION
Massive oral bleeding is a rare and nonspecific clinical presentation related to traumatic events, upper gastrointestinal tract tumors or inflammatory processes, ulceration, rupture of esophageal varices, use of anticoagulation therapy, and many other underlying issues. When bleeding occurs in healthy young patients without comorbidities nor apparent triggers, it arouses concerns and attention. One rarely reported cause of oral cavity bleeding can be CAD associated with vascular ES.[
First described by Eagle in 1937, ES is a rare condition characterized by an abnormal length and/or slope of SP or a CSL.[
SP physiological length is around 20–25 mm, and 3 cm is usually the upper limit. A length of 4 cm is highly associated with symptoms, varying from pain in the lateral cervical area alone to severe vascular or nervous complications. In the presented case, SP length was 5 cm on the left side and 5.5 cm on the right. The incidence of elongated SP in the general population is 4–10%, but only approximately 4% of these cases are symptomatic; therefore, ES is <2% in the general population. As we can also notice in our case, even if the SP on the right side was longer, it did not conflict with neurovascular structures, highlighting that the length itself is insufficient to provoke the symptoms. In this small percentage of cases, the anatomical abnormality determines symptoms that define two pictures commonly recognized as “neurological variant” and “vascular variant” due to conflict with the adjacent anatomical structures. Indeed, in its course from the temporal bone posteriorly to the mastoid apex toward the maxillo-vertebro-pharyngeal recess, SP has a relationship with many important vascular (carotid arteries, and internal jugular vein) and nervous structures (facial, vagus, glossopharyngeal, and hypoglossal nerves). Based on clinical presentation, Eagle classified the syndrome into two subgroups: classic and vascular type. The classic type includes odynophagia, dysphagia, and/or cervical or facial pain elicited by head rotational movements. The vascular form, also known as stylocarotid syndrome, is a quite rare condition in which an elongated SP compresses the extracranial carotid artery and results in parietal or periorbital pain, and neurological symptoms such as headache, dizziness, transient visual loss, syncope, and stroke, often caused by compression or by the dissection of the carotid artery itself. In our case, oral bleeding was the first clinical presentation. This uncommon presentation has been described only once in the literature [
Despite its benign nature, ES can lead to potentially severe complications. In the literature, many reports of transient ischemic attacks (TIAs) and strokes of the downstream territories of ICA are described, as an elongated SP has been recognized as a risk factor for CAD.[
The collection of medical, clinical, and radiological data can guide the diagnosis of vascular ES. Imaging, particularly a CT scan, is helpful in identifying the anatomical abnormalities and the presence of a neurovascular conflict. CT angiography is the gold standard and can provide further information regarding carotid flow, especially if stroke or dissection is suspected, and can be aided by 3D reconstructed images.[
Regarding treatment strategies, if patients with the classic form can be managed conservatively with analgesics, steroids, or local anesthetic, a surgical approach is preferred in cases of major vascular and neurological complications. A styloidectomy can be performed, and a transoral or transcervical method can be chosen.[
Patients with symptomatic CAD presenting with ischemic stroke, TIA, retinal ischemia, or local symptoms only and without subarachnoid hemorrhage should be treated according to the ESO guidelines for managing extracranial and intracranial artery dissection.[
There is no firm recommendation on whether to use emergency stenting of the dissected carotid artery. One study[
We suggest that stenting of the ICA is advisable to achieve CAD correction in case of persistent ischemic symptoms, as in our case (dysarthria). Stenting can lower the risk of persisting vessel damage caused by the ESP while guaranteeing successful reperfusion of the downstream territories. As a result of recent literature, endovascular management of ICA dissection can provide good results, with a low rate of periprocedural complication and good long-term follow-up. [
CONCLUSION
ES has many clinical presentations, as evidenced by the multitude of nonspecific symptoms reported in the literature. The pathophysiologic mechanism of ES is related to the compression of the surrounding neurovascular structures.
The classic form of ES is described when nerve compression leads to craniofacial and cervical pain, and the sympathetic plexus’s irritation around the ICA’s cervical segment can cause vertigo and syncope. On the other hand, the vascular form is caused by direct compression of the extracranial ICA by the elongated SP, resulting in TIA or stroke and sometimes in CAD. CAD resulting in oral bleeding seems to be a rare clinical presentation, and the exact mechanism remains unclear. Literature results and our experience make us believe that when dealing with vascular ES, the best treatment strategy is endovascular stenting of ICA with antiplatelet therapy, followed by surgical removal of the elongated SP to prevent stent fracture.
We want to highlight that our experience may contribute to identifying a rare possible complication of vascular ES. Furthermore, the vascular form of ES should always be considered in the differential diagnosis in the presence of spontaneous nontraumatic CAD.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Amorim JM, Lopes M, Ferreira C, Pinho J. Carotid artery dissection associated with long styloid process. Vasc Med. 2017. 22: 245
2. Aydin E, Quliyev H, Cinar C, Bozkaya H, Oran I. Eagle syndrome presenting with neurological symptoms. Turk Neurosurg. 2016. 28: 219-25
3. Badhey A, Jategaonkar A, Anglin Kovacs AJ, Kadakia S, De Deyn PP, Ducic Y. Eagle syndrome: A comprehensive review. Clin Neurol Neurosurg. 2017. 159: 34-8
4. Balcioglu HA, Kilic C, Akyol M, Ozan H, Kokten G. Length of the styloid process and anatomical implications for Eagle’s syndrome. Folia Morphol (Warsz). 2009. 68: 265-70
5. Baldino G, Di Girolamo C, De Blasis G, Gori A. Eagle syndrome and internal carotid artery dissection: Description of five cases treated in two Italian institutions and review of the literature. Ann Vasc Surg. 2020. 67: 565.e17-24
6. Brassart N, Deforche M, Goutte A, Wery D. A rare vascular complication of Eagle syndrome highlight by CTA with neck flexion. Radiol Case Rep. 2020. 15: 1408-12
7. Camarda AJ, Deschamps C, Forest D. I. Stylohyoid chain ossification: A discussion of etiology. Oral Surg Oral Med Oral Pathol. 1989. 67: 508-14
8. Debette S, Mazighi M, Bijlenga P, Pezzini A, Koga M, Bersano A. ESO guideline for the management of extracranial and intracranial artery dissection. Eur Stroke J. 2021. 6: XXXIX-LXXXVIII
9. Demirtaş H, Kayan M, Koyuncuoğlu HR, Çelik AO, Kara M, Şengeze N. Eagle syndrome causing vascular compression with cervical rotation: Case report. Pol J Radiol. 2016. 81: 277-80
10. Duarte-Celada WR, Jin D, Neves G, Windisch T. Bilateral carotid dissection due to Eagle syndrome in a young female. eNeurologicalSci. 2021. 24: 100353
11. Eagle WW. Elongated styloid process; further observations and a new syndrome. Arch Otolaryngol (1925). 1948. 47: 630-40
12. Eagle WW. Elongated styloid process; symptoms and treatment. AMA Arch Otolaryngol. 1958. 67: 172-6
13. Engelter ST, Traenka C, Gensicke H, Schaedelin SA, Luft AR, Simonetti BG. Aspirin versus anticoagulation in cervical artery dissection (TREAT-CAD): An open-label, randomised, non-inferiority trial. Lancet Neurol. 2021. 20: 341-50
14. Entezami P, Entezami P, Field NC, Nourollah-Zadeh E, Pinheiro-Neto CD, Dalfino JC. Neurosurgical management of vascular compression presenting as visual symptoms secondary to elongated styloid processes (Eagle syndrome). Br J Neurosurg. 2021. 35: 1-4
15. Galletta K, Granata F, Longo M, Alafaci C, De Ponte FS, Squillaci D. An unusual internal carotid artery compression as a possible cause of Eagle syndrome-a novel hypothesis and an innovative surgical technique. Surg Neurol Int. 2019. 10: 174
16. Hebant B, Guegan-Massardier E, Macaigne V, TriquenotBagan A. Ischemic stroke due to internal carotid artery dissection associated with an elongated styloid process (Eagle syndrome). J Neurol Sci. 2017. 372: 466-7
17. Hooker JD, Joyner DA, Farley EP, Khan M. Carotid stent fracture from stylocarotid syndrome. J Radiol Case Rep. 2016. 10: 1-8
18. Horio Y, Fukuda K, Miki K, Hirao N, Iwaasa M, Abe H. Dynamic assessment of internal carotid artery and elongated styloid process in a case of bilateral carotid artery dissection. Surg Neurol Int. 2020. 11: 163
19. Ikenouchi H, Takagi M, Nishimura A, Yamaguchi E, Koge J, Saito K. Bilateral carotid artery dissection due to Eagle syndrome in a patient with vascular Ehlers-Danlos syndrome: A case report. BMC Neurol. 2020. 20: 285
20. Jelodar S, Ghadirian H, Ketabchi M, Ahmadi Karvigh S, Alimohamadi M. Bilateral ischemic stroke due to carotid artery compression by abnormally elongated styloid process at both sides: A case report. J Stroke Cerebrovasc Dis. 2018. 27: e89-91
21. Jo H, Choi EH, Song J, Chung JW, Bang OY. Carotid artery dissection caused by Eagle syndrome. Precis Future Med. 2017. 1: 173-6
22. Kazmierski R, Wierzbicka M, Kotecka-Sowinska E, Banaszewski J, Pawlak MA. Expansion of the classification system for Eagle syndrome. Ann Intern Med. 2018. 168: 746-7
23. Kesav P, Hussain SI, Dogar MA, John S. Stylo-carotid syndrome causing bilateral cervical carotid artery dissection requiring endovascular intervention. Clin Neurol Neurosurg. 2020. 195: 105943
24. Lakner K, Savšek L. Carotid artery type of Eagle syndrome: An uncommon cause of ischemic stroke. Wien Klin Wochenschr. 2022. 135: 158-61
25. Landeen KC, Morse J, Mannion K. Spontaneous rupture of the internal carotid artery owing to an aberrant styloid process in an identical twin. JAMA Otolaryngol Head Neck Surg. 2020. 146: 385-6
26. Langlais RP, Miles DA, Van Dis ML. Elongated and mineralized stylohyoid ligament complex: A proposed classification and report of a case of Eagle’s syndrome. Oral Surg Oral Med Oral Pathol. 1986. 61: 527-32
27. Mann A, Kujath S, Friedell ML, Hardouin S, Wood C, Carter R. Eagle syndrome presenting after blunt trauma. Ann Vasc Surg. 2017. 40: 295.e5-8
28. Markus HS, Levi C, King A, Madigan J, Norris J. Antiplatelet therapy vs anticoagulation therapy in cervical artery dissection: The cervical artery dissection in stroke study (CADISS) randomized clinical trial final results. JAMA Neurol. 2019. 76: 657-64
29. Marnat G, Lapergue B, Sibon I, Gariel F, Bourcier R, Kyheng M. Safety and outcome of carotid dissection stenting during the treatment of tandem occlusions: A pooled analysis of TITAN and ETIS. Stroke. 2020. 51: 3713-8
30. Matsukawa S, Ishibashi R, Kitamura K, Sugiyama J, Yoshizaki W, Motoie R. Carotid micromesh stent for the cervical carotid artery dissecting aneurysm in a patient with vascular Eagle syndrome. J Stroke Cerebrovasc Dis. 2022. 31: 106487
31. Michiels TD, Marsman MS, van Veen A, Vriens PW, Lauret GJ, Heyligers JM. Eagle syndrome: A unique cause of carotid bleeding. JACC Case Rep. 2020. 2: 449-53
32. Moffat DA, Ramsden RT, Shaw HJ. The styloid process syndrome: Aetiological factors and surgical management. J Laryngol Otol. 1977. 91: 279-94
33. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009. 6: e1000097
34. Monsour PA, Young WG. Variability of the styloid process and stylohyoid ligament in panoramic radiographs. Oral Surg Oral Med Oral Pathol. 1986. 61: 522-6
35. Murtagh RD, Caracciolo JT, Fernandez G. CT findings associated with Eagle syndrome. AJNR Am J Neuroradiol. 2001. 22: 1401-2
36. Ohara N, Sakaguchi M, Okazaki S, Nagano K, Kitagawa K. Internal carotid artery dissection caused by an elongated styloid process: Usefulness of transoral ultrasonography. J Stroke Cerebrovasc Dis. 2012. 21: 918.e7-8
37. Okada Y, Mitsui N, Ozaki H, Sanada T, Yamamoto S, Saito M. Carotid artery dissection due to elongated styloid process treated by acute phase carotid artery stenting: A case report. Surg Neurol Int. 2022. 13: 183
38. Qureshi S, Farooq MU, Gorelick PB. Ischemic stroke secondary to stylocarotid variant of Eagle syndrome. Neurohospitalist. 2019. 9: 105-8
39. Raser JM, Mullen MT, Kasner SE, Cucchiara BL, Messé SR. Cervical carotid artery dissection is associated with styloid process length. Neurology. 2011. 77: 2061-6
40. Razak A, Short JL, Hussain SI. Carotid artery dissection due to elongated styloid process: A self-stabbing phenomenon. J Neuroimaging. 2014. 24: 298-301
41. Renard D, Azakri S, Arquizan C, Swinnen B, Labauge P, Thijs V. Styloid and hyoid bone proximity is a risk factor for cervical carotid artery dissection. Stroke. 2013. 44: 2475-9
42. Sasaki K, Komatsu F, Kato Y, Hirose Y. Carotid artery dissection and aneurysm with styloid process fracture. Neurol India. 2022. 70: 366-8
43. Selvadurai S, Williamson A, Virk JS, Clarke P. Eagle syndrome and carotid artery dissection: A rare skull base cause of stroke. BMJ Case Rep. 2022. 15: e247954
44. Shi D, Liu C, Wang L, Cao Y, Shi J. Bilateral carotid artery dissection associated with Eagle syndrome in a drug-addicted young adult with stroke: A case report. Neurol Sci. 2022. 43: 6105-9
45. Shimozato R, Hayashi M, Niimura M, Kugasawa K, Uemura H, Hidaka Y. Two patients with cerebral infarction who underwent endovascular treatment for internal carotid artery dissection related to an elongated styloid process. J Neuroendovasc Ther. 2018. 12: 355-61
46. Shindo T, Ito M, Matsumoto J, Miki K, Fujihara F, Terasaka S. A case of juvenile stroke due to carotid artery dissection from an elongated styloid process-revisiting conservative management. J Stroke Cerebrovasc Dis. 2019. 28: 104307
47. Smoot TW, Taha A, Tarlov N, Riebe B. Eagle syndrome: A case report of stylocarotid syndrome with internal carotid artery dissection. Interv Neuroradiol. 2017. 23: 433-6
48. Song JH, Ahn SK, Cho CB. Elongated styloid process as a cause of transient ischemic attacks. JAMA Neurol. 2013. 70: 1072-3
49. Steinmann EP. Styloid syndrome in absence of an elongated process. Acta Otolaryngol. 1968. 66: 347-56
50. Subedi R, Dean R, Baronos S, Dhamoon A. Carotid artery dissection: A rare complication of Eagle syndrome. BMJ Case Rep. 2017. 2017: bcr2016218184
51. Tan D, Crockett MT, Chiu AH. Delayed tine displacement of a CASPER carotid artery stent due to styloid process compression. Clin Neuroradiol. 2019. 29: 567-9
52. Tanti M, Smith A, Warren DJ, Idrovo L. Internal carotid artery dissection due to elongated styloid process. BMJ Case Rep. 2021. 14: e245908
53. Todo T, Alexander M, Stokol C, Lyden P, Braunstein G, Gewertz B. Eagle syndrome revisited: Cerebrovascular complications. Ann Vasc Surg. 2012. 26: 729.e1-5
54. Torikoshi S, Yamao Y, Ogino E, Taki W, Sunohara T, Nishimura M. A staged therapy for internal carotid artery dissection caused by vascular Eagle syndrome. World Neurosurg. 2019. 129: 133-9
55. Xhaxho S, Vyshka G, Kruja J. Eagle syndrome presenting as a neurological emergency: A case report. Surg Neurol Int. 2021. 12: 257
56. Xianjun H, Zhiming Z. A systematic review of endovascular management of internal carotid artery dissections. Interv Neurol. 2012. 1: 164-70
57. Zammit M, Chircop C, Attard V, D’Anastasi M. Eagle’s syndrome: A piercing matter. BMJ Case Rep. 2018. 11: e226611