- Department of Neurology, Mother Theresa University Hospital Center, Tirana, Albania.
- Department of Biomedical and Experimental Faculty of Medicine, University of Medicine, Tirana, Albania.
- Department of Neurosciences, Faculty of Medicine, University of Medicine, Tirana, Albania.
DOI:10.25259/SNI_362_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sokrat Xhaxho1, Gentian Vyshka2, Jera Kruja3. Eagle syndrome presenting as a neurological emergency: A case report. 07-Jun-2021;12:257
How to cite this URL: Sokrat Xhaxho1, Gentian Vyshka2, Jera Kruja3. Eagle syndrome presenting as a neurological emergency: A case report. 07-Jun-2021;12:257. Available from: https://surgicalneurologyint.com/surgicalint-articles/10870/
Abstract
Background: Eagle syndrome, due to the elongation of the styloid process as well as the calcification of the stylohyoid ligament, rarely presents itself with a major neurological disorder such as a brain infarct.
Case Description: Authors describe the case report of a previously healthy 64-year-old Caucasian male that complained of inability to control his right upper and lower extremity of an acute nature. Imaging at the emergency department (magnetic resonance of the brain and computerized angiography) showed the presence of elongated styloid process bilaterally with clear predomination at the left side. The brain ischemia (left temporal brain infarct) was due to carotid artery dissection, and the left internal carotid artery was not visualized during the contrast-enhanced angiography. The patient was hospitalized at a neurological facility and thereafter referred to surgery for styloidectomy.
Conclusion: The present case underscores the need for a prompt diagnosis and an enhanced awareness of this syndrome, especially among emergency department professionals.
Keywords: Brain infarct, Carotid artery, Eagle syndrome, Stylohyoid ligament, Styloid process
INTRODUCTION
The styloid process and the stylohyoid ligament, part of the neck structures, may present a variety of anatomical changes whose appearance can be purely innocuous as well as causing severe medical occurrences related to these alterations. It is not an unknown medical condition, although the first quoted source comes from an anatomist: Dominicus de Marchettis.[
The pioneering work of de Marchettis has been widely cited, as the first author to note that the styloid process might reach the “horns of the hyoid bone: cornua ossis hyoidei.”[
Details of the condition were reported approximately three centuries later, when Eagle in 1937 described the homonymous syndrome.[
We report the case of an Eagle syndrome with bilateral elongation of stylohyoid process that presented with ischemic stroke, in a previously healthy male patient.
CASE DESCRIPTION
The patient was a Caucasian male aged 64 years, reporting no relevant risk factors and an otherwise healthy life before the event. He presented at the emergency department of our hospital after two episodes of fainting, headache, and right eye amaurosis.
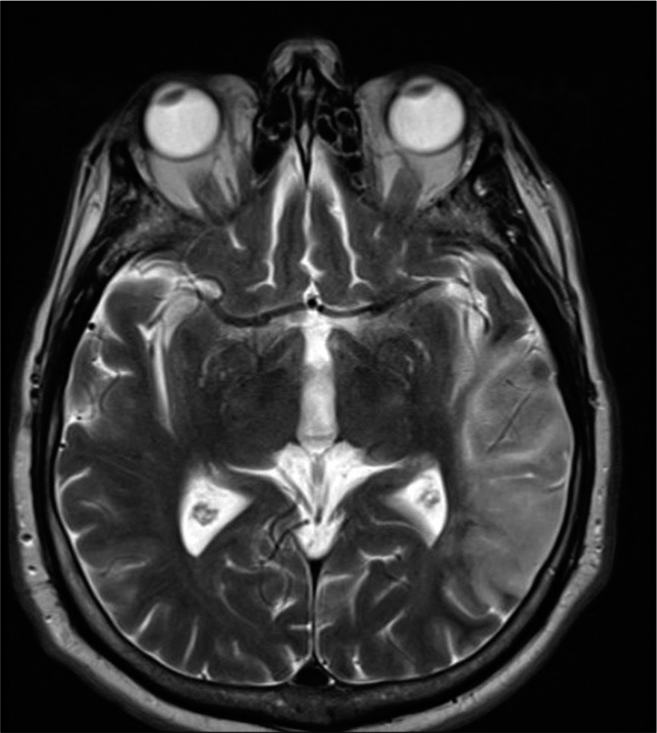
A computerized angiography of the head and neck as well as a brain magnetic resonance imaging (MRI) was performed the same day of his admission. A left temporal brain infarct was visualized [
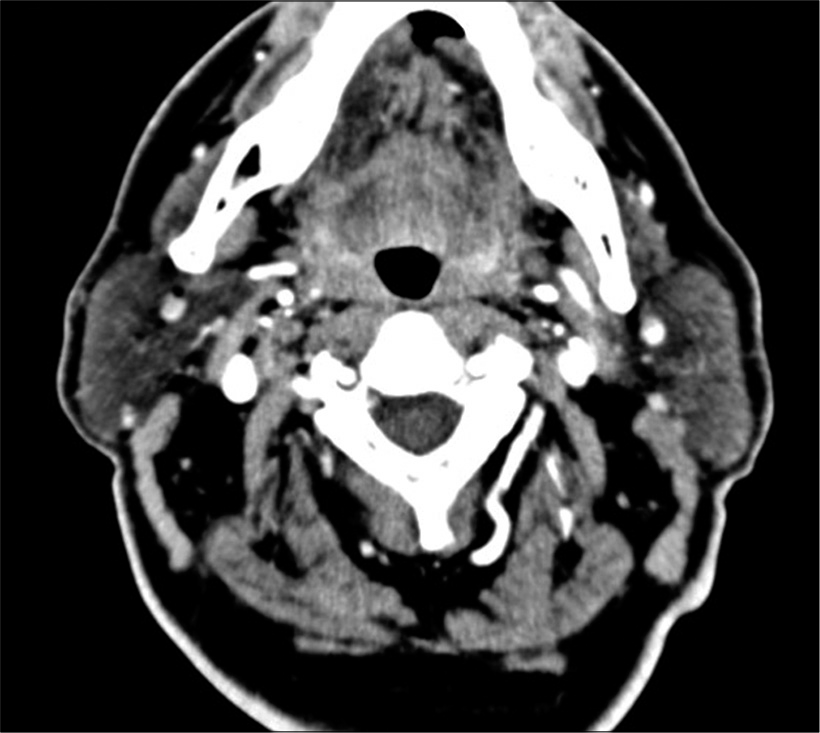
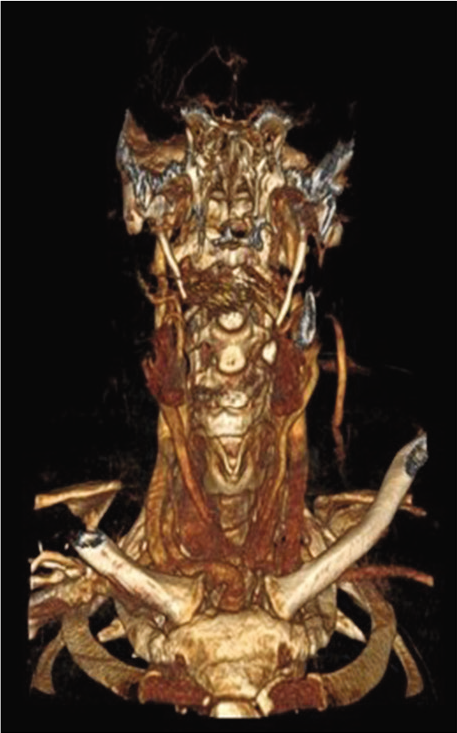
While slicing the neck structures in the computerized tomography, the presence of an elongated styloid process was detected in the axial imaging [
The neurological examination of the patient showed a right hemiparesis as well as ipsilateral hemi-spatial neglect. The angiographic study suggested a lack of visualization of the left internal carotid artery compatible with a dissection that led to the temporal ischemia [
With a patient having no other risk factors (he was not suffering from hypertension, diabetes, and hyperlipidemia; was not a smoker; presented a normal BMI; and was drinking alcohol only casually in social doses), we concluded that the Eagle syndrome was directly related to the internal carotid artery dissection.
The patient received a 10-day conservative therapy for the brain ischemic stroke and was eventually referred to a neurosurgical facility where a transcervical styloidectomy was performed. In a follow-up 3 months after the episode, the patient showed consistent improvement in the overall medical condition, with a remaining slight difficulty into performing fine movements with the right hand.
DISCUSSION
As a relatively new diagnostic construction, Eagle syndrome is something easily missed during routine neurological visits; furthermore, an important part of the complaints belongs to the specialties dealing with oral problems. This is as much as true especially when the syndrome presents in its “classical” form, with sore throat, otalgia, tinnitus, and dysphagia among other.[
The second form, which falls into the scope of neurological specialty and as such has a much more serious clinical picture, is the stylocarotid variant. The carotid artery might be impinged when the styloid process is elongated and calcified, leading to arterial dissection and following neurological injuries.[
It is unclear how and when the elongated, calcified styloid process will affect so seriously the carotid artery as to dissect it, especially as long as the event is acute. Minor neck traumas before the episode have been reported mainly when discussing the posterior cerebral circulation, in the so-called “beauty parlor syndrome” that affects vertebral arteries.[
Worth mentioning is the fact that all patients initially reported from Eagle himself had a tonsillectomy before the appearance of the syndrome, with a dense postoperative scar, that logically should have influenced into the calcification of the styloid process during the installation of the symptomatology.[
The issue of neck trauma as a contributing factor has been widely discussed, vis-à-vis a variety of changes it might produce, such as completing the ossification of the stylohyoid ligament, the pseudoaneurysm formation, and at last, the dissection itself of the carotid artery.[
While reviewing the literature, casuistic and reported therapies, one should take into account as well the considerable number of synonyms describing almost the same syndrome: stylohyoid syndrome, styloid syndrome, stylocarotid syndrome, long styloid process syndrome, calcified styloid process syndrome, hyoid bone syndrome, carotidynia, and Eagle syndrome.[
The preventive option of a styloidectomy is unclear and not recommended among asymptomatic patients.[
CONCLUSION
Eagle syndrome due to the styloid process elongation has a variety of clinical presentations. Although rarely, the condition might affect seriously the internal carotid artery causing its impingement, wall tear, pseudoaneurysm formation, as well as its complete dissection. In these cases, the syndrome will become a neurological emergency, with the patient suffering immediate and long-term consequences of a brain ischemic infarct.
The prevalence of the syndrome is not well defined, with sources suggesting that a styloid process longer than 3 cm is found in 4% of the population, but only 0.2% are symptomatic.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Baldino G, di Girolamo C, de Blasis G, Gori A. Eagle syndrome and internal carotid artery dissection: Description of 5 cases treated in 2 vascular institutions and review of the literature. Eur J Vasc Endovasc Surg. 2019. 58: e781-2
2. Brassart N, Deforche M, Goutte A, Wery D. A rare vascular complication of Eagle syndrome highlight by CTA with neck flexion. Radiol Case Rep. 2020. 15: 1408-12
3. Dao A, Karnezis S, Lane JS, Fujitani RM, Saremi F. Eagle syndrome presenting with external carotid artery pseudoaneurysm. Emerg Radiol. 2011. 18: 263-5
4. David J, Lieb M, Rahimi SA. Stylocarotid artery syndrome. J Vasc Surg. 2014. 60: 1661-3
5. de Marchettis D.editors. Anatomia, Patavii. 1652. p. 205
6. Dwight T. IX. Stylo-hyoid Ossification. Ann Surg. 1907. 46: 721-35
7. Eagle WW. Elongated styloid process; symptoms and treatment. AMA Arch Otolaryngol. 1958. 67: 172-6
8. Galletta K, Granata F, Longo M, Alafaci C, de Ponte FS, Squillaci D. An unusual internal carotid artery compression as a possible cause of Eagle syndrome-a novel hypothesis and an innovative surgical technique. Surg Neurol Int. 2019. 10: 174
9. Gruber W. Über enorm lange Processus styloides der Schläfenbeine. Arch Pathol Anat Physiol Klin Med. 1870. 50: 232-4
10. Jewett J, Moriarity R. Eagle syndrome: An incidental finding in a trauma patient: A case report. J Emerg Med. 2014. 46: e9-12
11. Langstaff LE, Abed T, Philpott J. Massively enlarged styloid process presenting as a submandibular mass. BMJ Case Rep. 2012. 2012:
12. Li Z, Hua Y, Yang J, Li J. Ultrasound evaluation of transient ischemic attack caused by styloid process elongation: A case report. Front Neurol. 2019. 10: 26
13. Lisan Q, Rubin F, Werner A, Guiquerro S, Bonfils P, Laccourreye O. Management of stylohyoid syndrome: A systematic review following PRISMA guidelines. Eur Ann Otorhinolaryngol Head Neck Dis. 2019. 136: 281-7
14. Lorman JG, Biggs JR. The Eagle syndrome. AJR Am J Roentgenol. 1983. 140: 881-2
15. Oluseisi AD. Traumatic Eagle syndrome: Does neck trauma result in complete ossification in partially ossified stylohyoid ligament. Int J Otorhinolaryngol. 2006. 4: 2
16. Qureshi S, Farooq MU, Gorelick PB. Ischemic stroke secondary to stylocarotid variant of eagle syndrome. Neurohospitalist. 2019. 9: 105-8
17. Shaqiri E, Vyshka G, Sinamati A, Ymaj B, Ismaili Z. Fatal basilar thrombosis possibly related to minor cervical trauma: A case report. Case Rep Med. 2010. 2010: 401978
18. Subedi R, Dean R, Baronos S, Dhamoon A. Carotid artery dissection: A rare complication of Eagle syndrome. BMJ Case Rep. 2017. 2017: bcr2016218184
19. Worden CP, Bhandari SS, Cable BB, Kuehl DR. Eagle syndrome: A rare case of atraumatic, painful cervical neck swelling. Clin Pract Cases Emerg Med. 2020. 4: 197-200
20. Zammit M, Chircop C, Attard V, D’Anastasi M. Eagle’s syndrome: A piercing matter. BMJ Case Rep. 2018. 11: e226611