- Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Jazan University, Jazan, Saudi Arabia,
- Division of Neurosurgery, Department of Surgery, University of Alberta, Edmonton, Alberta, Canada.
Correspondence Address:
Yahya H. Khormi
Division of Neurosurgery, Department of Surgery, University of Alberta, Edmonton, Alberta, Canada.
DOI:10.25259/SNI_192_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yahya H. Khormi, Andrew Nataraj. Effect of length time to surgery on postoperative hospital length of stay among neurosurgical patients. 06-Jun-2020;11:144
How to cite this URL: Yahya H. Khormi, Andrew Nataraj. Effect of length time to surgery on postoperative hospital length of stay among neurosurgical patients. 06-Jun-2020;11:144. Available from: https://surgicalneurologyint.com/surgicalint-articles/10072/
Abstract
Background: In most hospitals, inpatient urgent surgery is triaged based on the degree of urgency and time of surgical booking. A longer wait for semi-urgent surgery due to sharing resources between specialties might impact the postoperative course. The objective of this study is to determine the effect of length time to semi- urgent surgery on postoperative hospital length of stay among neurosurgical patients.
Methods: A retrospective cohort study was conducted included all admitted adult patients placed on semi-urgent University of Alberta Hospital surgical list between 2008 and 2013. Linear and logistic regression analyses were performed. The main exposure variable was time from surgical booking to the time of surgery, and the outcome variable was time from surgery to discharge.
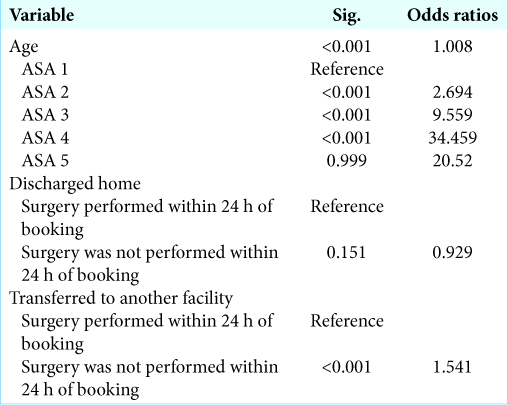
Results: A total of 1367 neurosurgical cases were included in the study. The mean age was 54.3 years. The mean length of time in the hospital before and after surgery was 1.2 and 12.5 days, respectively. Overall, the time from booking to surgery did not affect the time from surgery to discharge. Increased age, higher ASA score, and surgeries performed after 24 h from booking in the group of patients who were discharged to another facility were associated with a longer postoperative stay.
Conclusion: Neurosurgery patients booked for surgery to be done within 24 h waited longer to have their procedure completed. Overall, there was no significant association between length of time waiting for surgery and postoperative stay, although there was an increase in postoperative stays among patients who were discharged to another facility and had their surgeries performed after 24 h.
Keywords: Early surgery, Hospital length of stay, Late surgery, Postoperative stay, Waiting time
INTRODUCTION
In most Canadian hospitals, inpatient urgent surgery is triaged based on the degree of urgency and time of surgical booking. Hospitals have various systems whereby surgeons specify the former. These typically include three tiers: emergent (must be done within 1 h), urgent (must be done within 4–8 h depending on the institution), and semi-urgent (must be done within 24 h). The “life or limb threatened” nature of the first tier ensures that they are done within the specified hour.
A longer wait for semi-urgent surgery due to sharing resources between specialties might impact postoperative course: as an example, patients harboring active surgical infections such as abscesses for a longer period of time might require longer to clear the infection and to recover from the effects of an infection, longer periods of mandated bed rest for certain conditions such as fractures could result in an increased risk of venous thromboembolism. As a result, they may ultimately have a worse clinical outcome, increased length of postoperative stay, and overall increased cost related to their presenting condition.[
In a system with fixed health-care resources, it is important to invest in both effective and cost-effective methods.[
This objective of this study is to determine the effect of length time on semi-urgent surgery on postoperative hospital length of stay for neurosurgery patient.
MATERIALS AND METHODS
A retrospective cohort study was conducted included all admitted patients over age 17 placed on semi-urgent (E24) University Hospital emergency surgical list, Edmonton, Alberta, between 2008 and 2013. The main exposure variable was time from surgical booking to time of skin incision in hours, and the outcome variable was mean time from surgery to discharge. The potential confounders age, sex, procedure type, and patient comorbidities (ASA class) were included in the study.
Data were obtained from combining the surgical database (date of the booking, date of surgery, procedure type, surgical time, age, sex, and ASA class) and admissions database (date of discharge and discharge disposition). Time to surgery of 5 days or longer was unusual and thus graded into a single category.
Linear and logistic regression analyses were performed, with the dependent variable being the time from surgery to discharge. Subgroup analysis by age, ASA score, and discharge disposition were also performed.
RESULTS
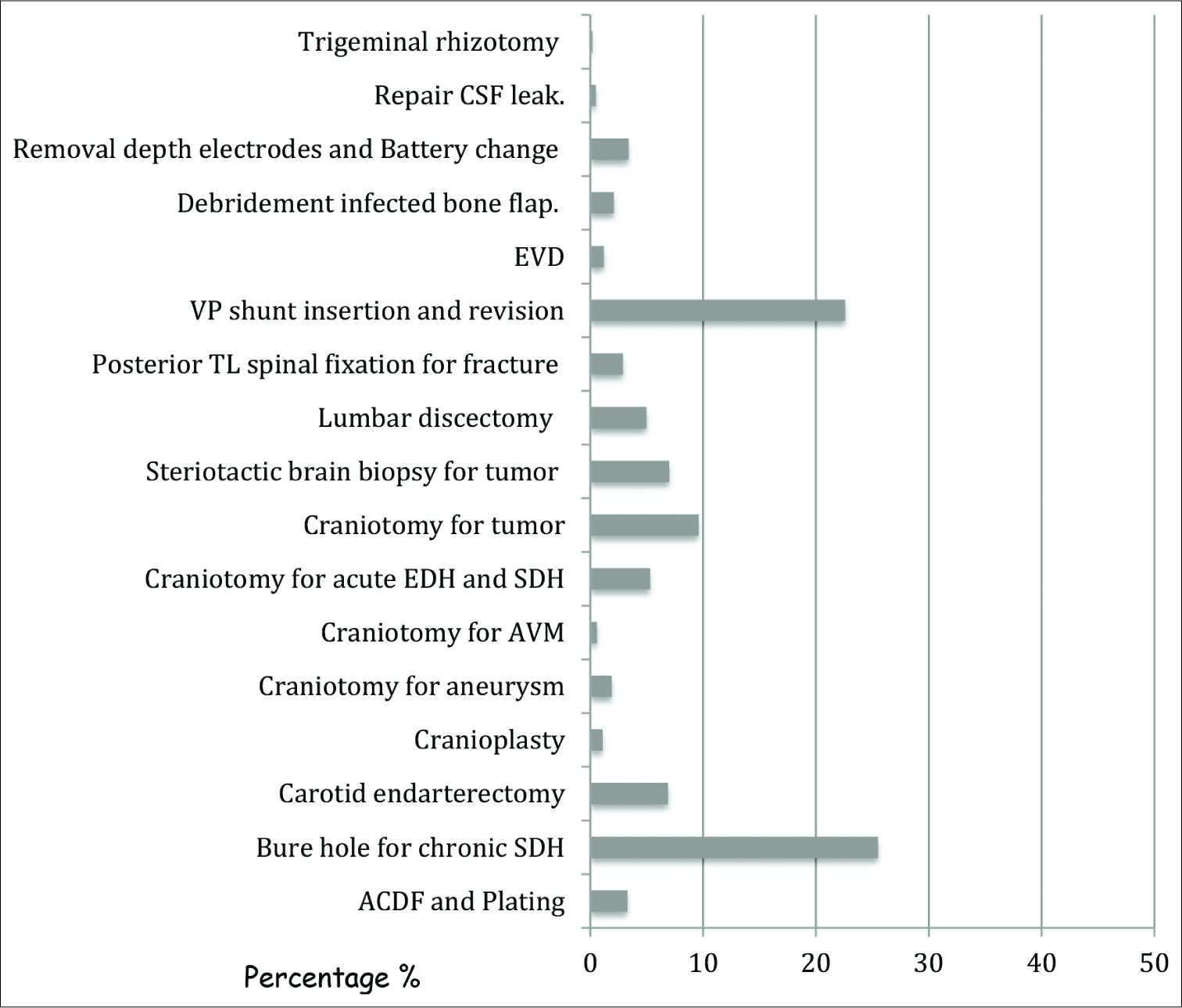
There were 1367 neurosurgical cases, which constitute 7.22 % of all surgical specialties’ cases;
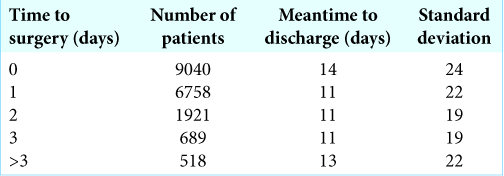
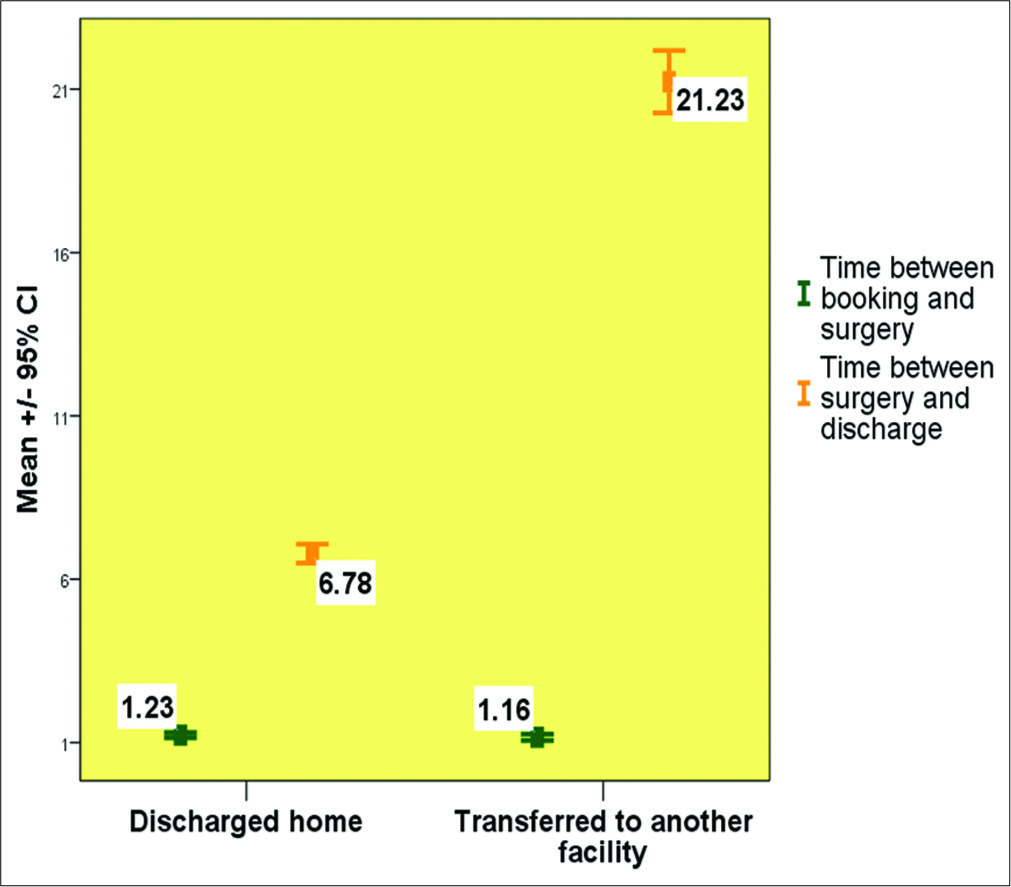
There were 351 patients (26%) who were transferred to an acute care facility, 208 (15%) to continuing care facility, 111 (8%) to home with help, and 695 (51%) to home with no help. The mean length of stay after surgery was 6.78 days if the patient discharged home and 21.23 if discharged to another facility [
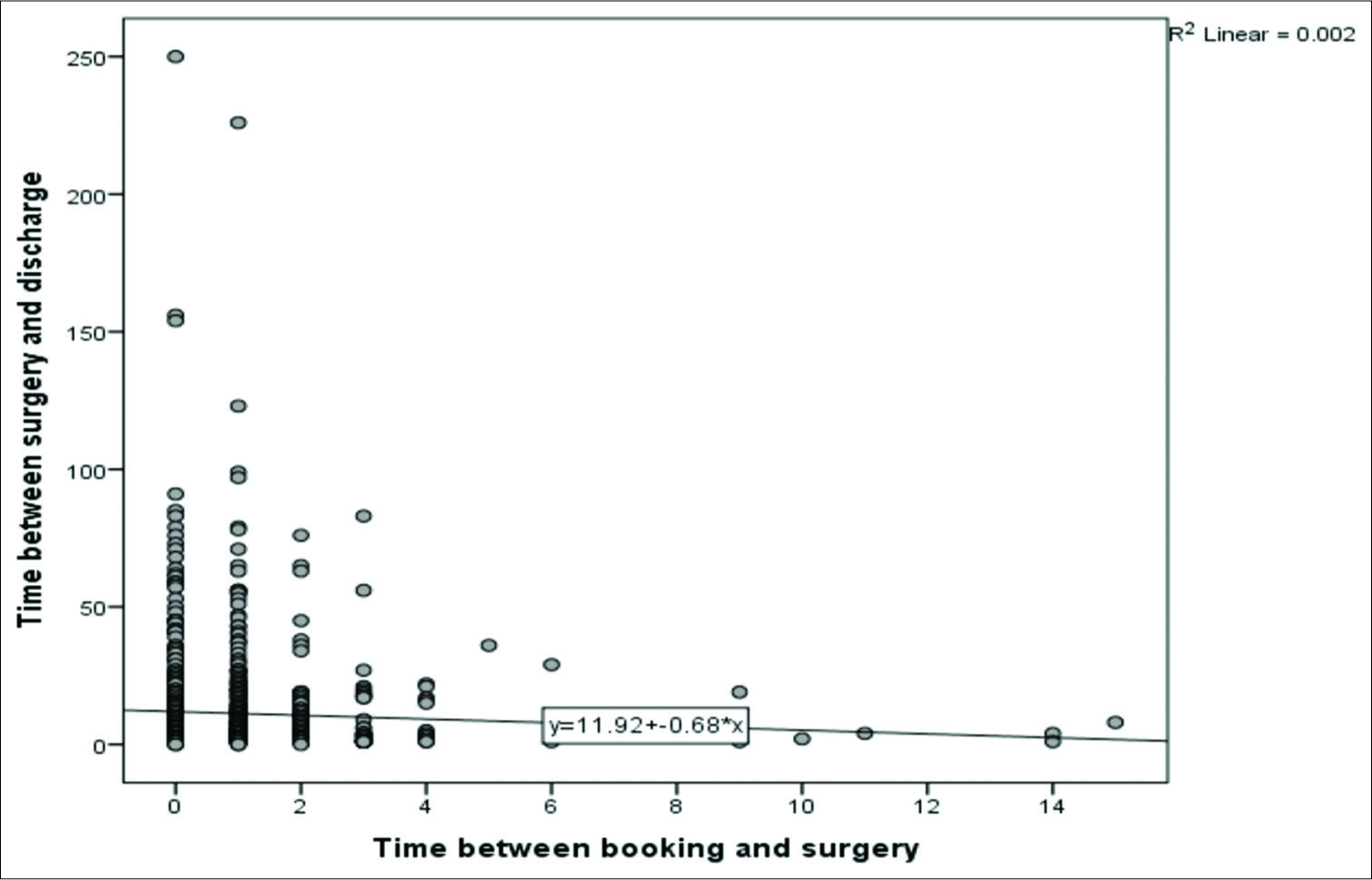
In the regression model, including all patients, overall, the time from booking to surgery did not affect the time from surgery to discharge [
DISCUSSION
This study showed that neurosurgery patients booked for surgery to be done within 24 h waited longer to have their procedure completed. Overall, there was no significant association between length of time waiting for surgery and postoperative stay after adjusting for confounders, although the subgroup analysis revealed an increase in postoperative stays in the group of patients who were discharged to another facility if their surgery was delayed more than 24 h. Few studies have investigated the effect of delay in surgery on postoperative outcomes. Munster et al. noted a significant decrease in hospital LOS for burn care as a function of more aggressive and urgent surgical closure of the burn wound.[
One of the aims of the study was to identify factors that are associated with longer hospital stays to potentially target them as a cost-saving measure. However, time to being ready for discharge is an important variable to include in future studies and that could precisely determine the actual postoperative length of stay needed.
Certain procedures, higher ASA class, and increase age were significantly associated with longer postoperative stays.
CONCLUSION
Neurosurgery patients booked for surgery to be done within 24 h waited longer to have their procedure completed. There was no significant association between length of time waiting for surgery and postoperative stay, although there was a significant increase in postoperative stays in the group of patients who were discharged to another facility and had their surgeries performed after 24 h. Higher ASA class and increase age were significantly associated with longer postoperative stays.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bellelli G, Mazzola P, Corsi M, Zambon A, Corrao G, Castoldi G. The combined effect of ADL impairment and delay in time from fracture to surgery on 12-month mortality: An observational study in orthogeriatric patients. J Am Med Dir Assoc. 2012. 13: 664.e9-14
2. Chipman JG, Deuser WE, Beilman GJ. Early surgery for thoracolumbar spine injuries decreases complications. J Trauma. 2004. 56: 52-7
3. Findlay JM. Canadian health care explained to U.S. colleagues: The good, the bad and the ugly. Can J Neurol Sci. 2010. 37: 310-2
4. Kerwin AJ, Frykberg ER, Schinco MA, Griffen MM, Murphy T, Tepas JJ. The effect of early spine fixation on non-neurologic outcome. J Trauma. 2005. 58: 15-21
5. Kim L, Tan ST. Economic impact of untimely surgical intervention for acute plastic surgery patients. N Z Med J. 2008. 121: 26-32
6. Munster AM, Smith-Meek M, Sharkey P. The effect of early surgical intervention on mortality and cost-effectiveness in burn care, 1978-91. Burns. 1994. 20: 61-4
7. Schinkel C, Frangen TM, Kmetic A, Andress HJ, Muhr G. German Trauma Registry. Timing of thoracic spine stabilization in trauma patients: Impact on clinical course and outcome. J Trauma. 2006. 61: 156-60
8. Still JM, Law EJ, Belcher K, Thiruvaiyarv D. Decreasing length of hospital stay by early excision and grafting of burns. South Med J. 1996. 89: 578-82