- Department of Neurosurgery, Fundación Clínica Shaio, Colombia
- Neurosurgery Program, Universidad El Bosque, Bogotá, Colombia
- Medicine Program, Universidad Militar, Bogotá, Colombia
Correspondence Address:
Oscar Iván Molina-Romero, Department of Neurosurgery, Fundación Clínica Shaio, Neurosurgery Program, Universidad El Bosque, Bogotá, Colombia.
DOI:10.25259/SNI_562_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Juan Pablo Leal-Isaza1,2, Oscar Iván Molina-Romero1,2, Juan Carlos Diez-Palma1, Andrés Fonnegra-Caballero1, Andrés Segura Hernández1, Laura Daniela Ramirez-Melo3, Julio Roberto Fonnegra-Pardo1. Effectiveness of thalamotomy with Gamma Knife radiosurgery as a multitarget strategy in patients with complex trigeminal neuralgia. 08-Nov-2024;15:403
How to cite this URL: Juan Pablo Leal-Isaza1,2, Oscar Iván Molina-Romero1,2, Juan Carlos Diez-Palma1, Andrés Fonnegra-Caballero1, Andrés Segura Hernández1, Laura Daniela Ramirez-Melo3, Julio Roberto Fonnegra-Pardo1. Effectiveness of thalamotomy with Gamma Knife radiosurgery as a multitarget strategy in patients with complex trigeminal neuralgia. 08-Nov-2024;15:403. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13212
Abstract
Background: In the setting of refractory neuralgia or other complex facial pains, the intensity of the pain does not decrease despite medical and even surgical interventions. This report aims to describe the experience of an institution in the management of refractory trigeminal neuralgia and other complex facial pains with Gamma Knife radiosurgery (GKR), including thalamotomy as a multitarget strategy.
Methods: We conducted a retrospective observational study. Data were obtained from 50 patients with complex trigeminal neuralgia treated with GKR, in whom the thalamus was included as a target. The Visual Analog Scale (VAS) and the Barrow Neurological Institute (BNI) scale were considered before treatment and at the follow-up. The Wilcoxon test was used to compare the VAS scores and the McNemar test for the BNI scale.
Results: The mean age was 62.7 years (standard deviation = 16.3). The indications for management with thalamotomy were neuralgia refractory to medical management (68%), recurrent pain after previous rhizolysis with GKR (20%), atypical deafferentation-type pain in patients with radiofrequency background (10%), and anatomical deformation of the trigeminal nerve by a tumor (2%). Before treatment, all patients were classified as BNI V. At follow-up, a satisfactory response to treatment was described in 82.05% of cases (P = 0.001 McNemar). The median preoperative pain evaluated with VAS was 10 (interquartile range [IQR] = 10–10), while at follow-up, it was 6 (IQR = 1–7) (P = 0.001 Wilcoxon).
Conclusion: The thalamus is a versatile, effective, and safe therapeutic target for ablative management in patients with complex facial pain.
Keywords: Facial pain, Trigeminal neuralgia, Trigeminal nerve, Thalamotomy, Gamma Knife radiosurgery, Stereotactic radiosurgery
INTRODUCTION
Trigeminal neuralgia is a condition characterized by a high intensity and short-duration pain distributed in one or more divisions of the trigeminal nerve. It is recurrent with an abrupt onset and electrical nature. The symptom tends to be debilitating with a significant effect on the quality of life of the patients.[
Medical management with neuronal membrane-stabilizing drugs is the first-line treatment. The effectiveness in symptom control can be up to 90%; however, this effect may not be permanent and side effects can arise in up to 23% of cases, entailing the suspension of treatment in most of these cases.[
Gamma Knife radiosurgery (GKR) allows a noninvasive treatment of the intracranial structures responsible for the conduction and interpretation of pain. In the setting of refractory neuralgia or other complex facial pains, its usefulness lies in the possibility of treating not only the trigeminal nerve as a unique target (rhizolysis) but also other structures, such as the thalamus. This report aims to describe an institution’s experience in managing refractory trigeminal neuralgia and other complex facial pains with GKR, including thalamotomy as a multitarget strategy, analyzing its indications, results, and complications attributable to the treatment.
MATERIALS AND METHODS
We conducted a retrospective observational study. Data were collected from Fundación Clínica Shaio in Bogotá, Colombia. We obtained the approval of the Institution’s Ethics Committee (DIB23-09). Data were obtained from 50 patients with complex trigeminal neuralgia treated with GKR, in whom the thalamus was included as a therapeutic target.
Pretreatment clinical variables, data from the radiation treatment, and follow-up data were collected from medical charts and phone interviews. For clinical outcomes, the Visual Analog Scale (VAS) and the Barrow Neurological Institute (BNI) scale were considered before treatment and at the follow-up time. Complications were described during the 1st-month posttreatment (acute complications) and in the last clinical control (chronic complications).
The data were analyzed using the statistical program STATA 17.0. For quantitative variables, normality in the distribution of the data was verified by graphs, the Shapiro-Wilk test, and kurtosis. According to the results, measures of central tendency were applied, mainly median with interquartile range (IQR) and mean with standard deviation (SD). For qualitative variables, proportions were calculated. The Wilcoxon test was used to compare the VAS scores and the McNemar test for the BNI scale. For this last scale, a satisfactory response was considered for BNI I, II, and III, and unsatisfactory for BNI IV and V. The cut-off point to establish statistical significance was 0.05 in both tests.
RESULTS
Fifty patients with refractory, secondary, or atypical trigeminal neuralgia in whom the thalamus was selected as a therapeutic target for ablative treatment through GKR were included. These patients were treated with Gamma Knife Perfexion between August 2015 and April 2022. 70% of the patients were women, while 30% were men. The mean age was 62.7 years (SD = 16.3). 38% of the patients had a background of previous surgical management (microvascular decompression), 24% of previous radiosurgery, and 48% of previous percutaneous management [
The specific thalamic target selected for treatment with GKR was the central median nucleus of the thalamus, which we located having as the reference the intermediate point of the inter-commissural line, 10 mm posterior in the (y) axis, 10 mm lateral in the (x) axis, and 3.5 mm higher on the (z) axis [
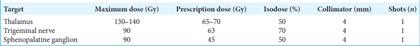
Figure 1:
GKR treatment planning images. a) Coronal slide of T1-weighted MRI shows the prescription dose area of the right trigeminal nerve (63 Gy) (blue arrow) and the planning axis of the left thalamus (green cross) located lateral and superior to the posterior inter-commissural line (PC) (red box). b) Sagittal slide of the T1-weighted MRI shows the sphenopalatine ganglion prescription dose area (45 Gy) (blue arrow) and the thalamus prescription dose area (70 Gy) (yellow arrow). The anterior (red box - AC) and posterior (red box - PC) limits of the inter-commissural line can also be observed. c) Axial slide of heavily T2-weighted MRI shows a tumor in the right cerebellopontine angle (red asterisk) deforming the right trigeminal nerve, which is not observed, unlike the left trigeminal nerve (blue arrow). d) Coronal slide of T1-weighted MRI of the same patient in image c, shows the tumor of the right cerebellopontine angle (red asterisk), with the prescription dose of 12 Gy (yellow circle) and the safety dose of 10 Gy (green circle). The prescription dose of the thalamus (70 Gy) is shown in the yellow circle indicated by the yellow arrow and the green circle around it corresponds to the safety dose (10 Gy).
In 85% of the cases, treatment included the retrogasserian portion of the ipsilateral trigeminal nerve and the contralateral posteromedial thalamus (ipsilateral rhizolysis plus contralateral thalamotomy), being refractory neuralgia, and deafferentation-type pain, as the two main indications. In 10% of cases, the selected targets were the ipsilateral sphenopalatine ganglion and the posteromedial thalamus, mainly in patients with refractory pain and autonomic manifestations. In 5% of cases, the contralateral posteromedial thalamus was the only target when an anatomical deformation of the nerve was described. All procedures were performed in one session on an outpatient basis. The median time per fraction was 120 min (IQR 100–142). The median hospital stay was 4.4 h (IQR 3.7–5.8). Other treatment variables are described in
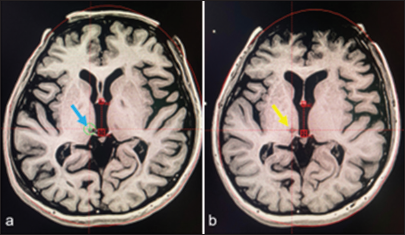
Regarding follow-up, data from 39 patients were obtained with a mean follow-up of 38.5 months (SD = 19.1). Before treatment, all these patients were classified as BNI V. At follow-up, 10.2% were classified as BNI I, 5.1% as BNI II, 66.6% as BNI III, and 17.9% as BNI IV. Any case was classified as BNI V after treatment. A satisfactory response to treatment was described in 82.05% of cases (P = 0.001 McNemar). The median preoperative pain evaluated with VAS was 10 (IQR 10–10), while at follow-up, it was 6 (IQR 1–7) (P = 0.001 Wilcoxon). The ablative effect was verified in magnetic resonance imaging 1 year after treatment [
Figure 2:
Ablative effect of GKR. (a) Sagittal slide of T1-weighted MRI planning radiation dose delivery to the right thalamus (blue arrow). (b) control image one year after treatment shows a hypointense area at the treatment site (yellow arrow) confirming the ablative effect at the level of the right posteromedial thalamus. The upper red box (AC) corresponds to the anterior limit of the inter-commissural line, and the lower red box (PC) to the posterior limit.
Concerning acute complications, 74.3% of patients did not present any complications. 23% had a transient headache, 7.6% had pain at the frame’s fixation points, and 2.5% had nausea. All manifestations responded satisfactorily to medical treatment. At the time of the last follow-up, there were no cases of painful anesthesia or corneal ulcers. Paraesthesias were the only complication described in 17.9% of patients.
DISCUSSION
Although the majority of cases of trigeminal neuralgia have a satisfactory response to medical treatment, there are some cases in which there is a failure of this treatment modality or the adverse effects force to consider interventional alternatives. Microvascular decompression is the most effective in symptom control, but it has a potential risk of complications such as infection, hemorrhages, fistula, and injury of nervous structures. Other options, such as radiofrequency, neurolysis with glycerol, or compression with a balloon, although less invasive, tend to have variable effectiveness and also have a potential risk of complications, with painful anesthesia as the most prominent.[
Stereotactic thalamotomy through thermal ablation radiofrequency has been used for the treatment of pain since shortly after the beginning of stereotaxy application.[
Ablative thalamotomy can be used for the management of different oncologic and nononcologic painful syndromes.[
In this series of patients with complex facial pain, we emphasize not only the effectiveness of GKR in terms of reducing the intensity of facial pain but also the versatility of this method when selecting the therapeutic target depending on the clinical characteristics or the patient’s needs. As it is noninvasive management that combines the principles of stereotaxy with ionizing radiation, we can consider multitarget management, including structures that participate in the transmission and interpretation of pain, such as the trigeminal nerve, thalamus, sphenopalatine ganglion, and even the cingulum.[
Data reported in the literature suggest that thalamotomy with GKR can produce an initial pain reduction in 43.3–100% of the patients; however, in some cases, it fails to provide long-term pain control [
Although the technique is considered safe with an estimated risk of complications of <5%, some reports have described complications attributable to radiation such as headache, nausea, vomiting, diplopia, contralateral weakness of upward gaze, vertigo, hemianesthesia, paresthesia, and progressive hemiparesis.[
Limitations
Even though the most frequent and representative indication was refractory neuralgia, other indications were described and included in the final analysis. This can generate some grade of heterogeneity in the sample despite having as a common feature the ablative management in the thalamus.
CONCLUSION
The thalamus is a versatile, effective, and safe therapeutic target for ablative management in patients with complex facial pain. It can be part of a multitarget strategy adaptable together with other structures involved in the pain pathway, which can increase effectiveness compared to treatment with a single target.
Ethical approval
The Institutional Ethics Committee approval is obtained , No:DIB23-09.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Belvis R, Mas N, Roig C. Novedades en la reciente clasificacion Internacional de las Cefaleas: Clasificacion ICHD-III beta [Changes introduced into the recent International classification of headache disorders: ICHD-III beta classification]. Rev Neurol. 2015. 60: 81-9
2. Bendtsen L, Zakrzewska JM, Abbott J, Braschinsky M, Di Stefano G, Donnet A. European Academy of Neurology guideline on trigeminal neuralgia. Eur J Neurol. 2019. 26: 831-49
3. Bendtsen L, Zakrzewska JM, Heinskou TB, Hodaie M, Leal PR, Nurmikko T. Advances in diagnosis, classification, pathophysiology, and management of trigeminal neuralgia. Lancet Neurol. 2020. 19: 784-96
4. Burchiel KJ, Raslan AM. Contemporary concepts of pain surgery. J Neurosurg. 2019. 130: 1039-49
5. Dougherty P, Lee J, Dimitiou T, Lenz F, editors. Medial thalamotomy. Pain surgery. New York: Thieme; 2001. p.
6. Franzini A, Attuati L, Zaed I, Moosa S, Stravato A, Navarria P. Gamma Knife central lateral thalamotomy for the treatment of neuropathic pain. J Neurosurg. 2020. 135: 228-36
7. Franzini A, Rossini Z, Moosa S, Tropeano MP, Milani D, Attuati L. Medial thalamotomy using stereotactic radiosurgery for intractable pain: A systematic review. Neurosurg Rev. 2022. 45: 71-80
8. Hariz MI, Bergenheim AT. Thalamic stereotaxis for chronic pain: Ablative lesion or stimulation?. Stereotact Funct Neurosurg. 1995. 64: 47-55
9. Haridas A, Mathewson C, Eljamel S. Long-term results of 405 refractory trigeminal neuralgia surgeries in 256 patients. Zentralbl Neurochir. 2008. 69: 170-4
10. Jarrahi A, Cantrell R, Norris C, Dhandapani K, Barrett J, Vender J. Trigeminal neuralgia treatment outcomes following gamma knife stereotactic radiosurgery. Int J Transl Med. 2022. 2: 543-54
11. Jeanmonod D, Morel A, editors. The central lateral thalamotomy for neuropathic pain. Textbook of stereotactic and functional neurosurgery. Berlin: Springer; 2009. p. 2081-96
12. Lovo EE, Torres B, Campos F, Caceros V, Reyes WA, Barahona KC. Stereotactic gamma ray radiosurgery to the centromedian and parafascicular complex of the thalamus for trigeminal neuralgia and other complex pain syndromes. Cureus. 2019. 11: e6421
13. Molina-Romero OI, Segura-Hernandez A, Fonnegra-Caballero A, Carlos Diez-Palma J, Cortés-Muñoz F, Fonnegra-Pardo JR. Gamma Knife radiosurgery-12 years of experience in a high-complexity center of a middle-income country. Surg Neurol Int. 2022. 13: 582
14. Molina-Romero OI, Carlos Diez-Palma J, Fonnegra-Caballero A, Segura-Hernandez A, Leal-Isaza Juan P, Fonnegra-Pardo JR. Bilateral anterior cingulotomy with Gamma Knife radiosurgery: Another alternative for the treatment of non-oncologic intractable chronic pain. J Radiosurg SBRT. 2024. 9: 165-9
15. Steiner L, Forster D, Leksell L, Meyerson BA, Boethius J. Gammathalamotomy in intractable pain. Acta Neurochir (Wien). 1980. 52: 173-84
16. Weigel R, Krauss JK. Center median-parafascicular complex and pain control. Review from a neurosurgical perspective. Stereotact Funct Neurosurg. 2004. 82: 115-26