- Department of Neurosurgery, Kobe University School of Medicine, Kusunoki-cho, 7-5-2, Chuo-ku, Kobe, Japan
- Department of Neurosurgery, NTT Medical Center Tokyo, Tokyo, Japan
- Department of Neurosurgery, Osaka City University Graduate School of Medicine, Osaka, Japan
- Department of Neurosurgery, Nippon Medical School, Tokyo, Japan
Correspondence Address:
Noriaki Minami
Department of Neurosurgery, Nippon Medical School, Tokyo, Japan
DOI:10.4103/2152-7806.132562
Copyright: © 2014 Minami N This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Minami N, Kimura T, Uda T, Ochiai C, Kohmura E, Morita A. Effectiveness of zigzag Incision and 1.5-Layer method for frontotemporal craniotomy. Surg Neurol Int 15-May-2014;5:69
How to cite this URL: Minami N, Kimura T, Uda T, Ochiai C, Kohmura E, Morita A. Effectiveness of zigzag Incision and 1.5-Layer method for frontotemporal craniotomy. Surg Neurol Int 15-May-2014;5:69. Available from: http://surgicalneurologyint.com/surgicalint_articles/effectiveness-of-zigzag-incision-and-1-5%e2%80%91layer-method-for-frontotemporal-craniotomy/
Abstract
Background:In this era of minimally invasive treatment, it is important to make operative scars as inconspicuous as possible, and there is a great deal of room for improvement in daily practice. Zigzag incision with coronal incision has been described mainly in the field of plastic surgery, and its applicability for skin incision in general neurosurgery has not been reported.
Methods:Zigzag incision with 1.5-layer method was applied to 14 patients with unruptured cerebral aneurysm between April 2011 and August 2012. A questionnaire survey was administered among patients with unruptured aneurysm using SF-36v2 since April 2010. The results were compared between patients with zigzag incision and a previous cohort with traditional incision.
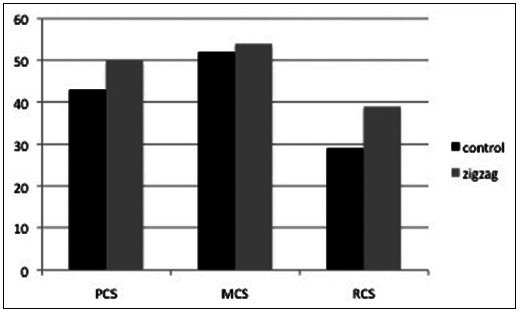
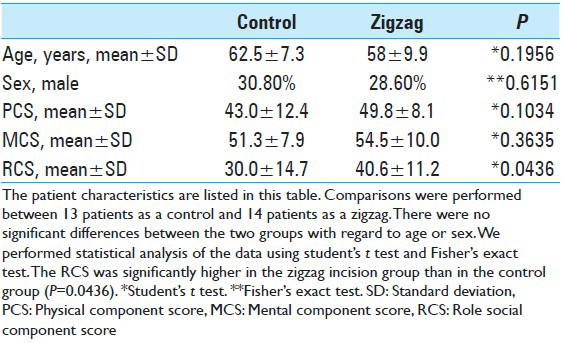
Results:There were no cases of complications associated with the operative wound. In the questionnaire survey, all parameters tended to be better in the patients with zigzag incision, and role social component score (RCS) was significantly higher in the zigzag group than in the traditional incision group (P =0.0436).
Conclusion:Zigzag incision using the 1.5-layer method with frontotemporal craniotomy seems to represent an improvement over the conventional curvilinear incision with regard to cosmetic outcome and RCS.
Keywords: SF36v2, unruptured cerebral aneurysm, zigzag incision, 1.5-layer technique
INTRODUCTION
There has been a great deal of recent progress in both techniques and instruments for use in the field of neurosurgery. Endovascular coiling is no longer an alternative for clipping surgery, and has become the mainstream form of treatment for cerebral aneurysms. This method does not involve manipulation of complex and fragile brain tissue and it does not leave scarring in the skin, both of which contribute to its superiority for endovascular surgery. Neurosurgeons are required to be more conscious of invasiveness in this era of minimally invasive surgery; in addition to basic neurosurgical techniques, care should be taken with regard to esthetic issues. Although neurosurgeons generally attempt to render operative scars as inconspicuous as possible, there is still room for improvement in many aspects.
The zigzag coronal incision has been reported for this purpose, mainly in the field of plastic surgery.[
MATERIALS AND METHODS
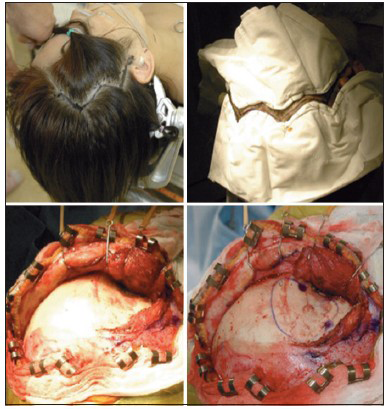
From April 2010 to March 2011, we had 35 patients who underwent clipping surgery for unruptured aneurysms with conventional curvilinear incision at NTT Medical Center Tokyo. Then, between April 2011 and August 2012, zigzag incision with 1.5 layer technique was applied in 14 consecutive patients with unruptured cerebral aneurysm who were otherwise in good health at the same facility. The description of the zigzag incision with 1.5-layer method is as follows: After induction of general anesthesia and fixation of the patient's head with a Mayfield® three-point frame, ordinary curvilinear incision behind the hairline is designed to expose McCarty's keyhole. The zigzag line can be drawn behind this curvilinear line [
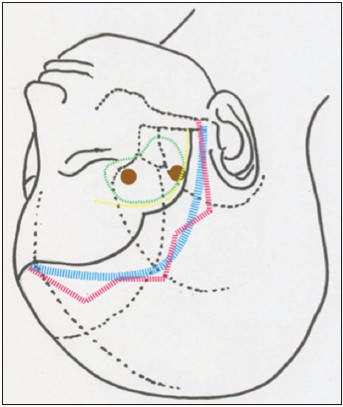
Figure 1
Green line indicates craniotomy area. Blue line is the conventional curvilinear incision behind the hairline, which is designed to expose McCarty's keyhole and lateral orbital rim. Based on the blue line, the zigzag line can be drawn. The angle between each short linear line (4-5 cm) is approximately 120°–150°
After the procedure, standard craniotomy and microsurgical manipulation can begin. In closing, the temporal fascia is approximated with nonabsorbable sutures. Then, the skin is sutured where the angles of the zigzag meet.
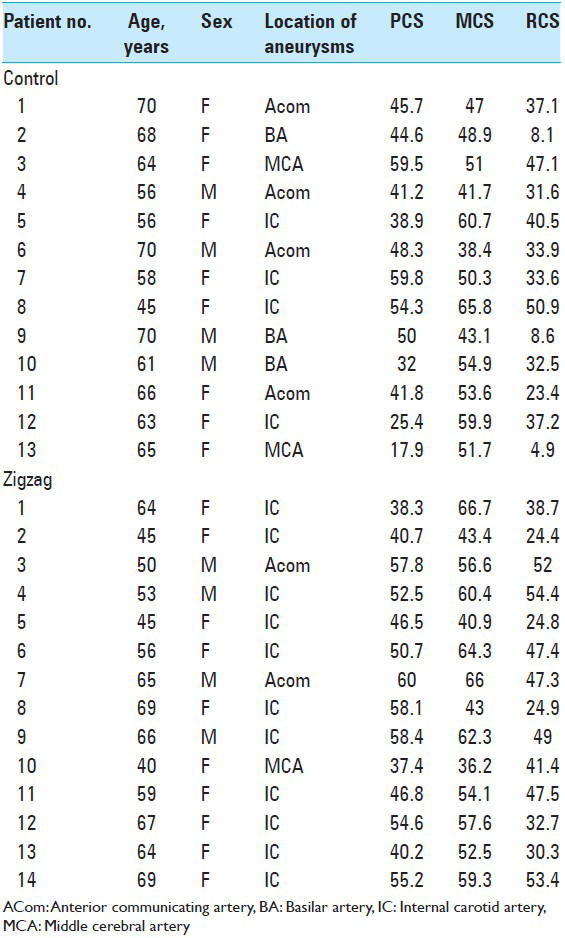
In this era of minimally invasive surgery, neurovascular surgeons are required to be more conscious of invasiveness especially in treating unruptured aneurysms. However, it is sometimes difficult to measure patients’ satisfaction through doctors’ subjective eyes. To evaluate it objectively, a questionnaire survey has been administered using SF-36v2 scoring system regarding quality of life (QOL) for all cases of unruptured aneurysm one month after surgery in our facility since April 2010. SF36v2 questionnaire sheet consists of only 36 questions, which yields an 8-scale profile of functional health. The 8-scale profile indicates, physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH). Summary scores, that is, physical component score (PCS), mental component score (MCS), and role social component score (RCS), are calculated from the 8-scale profile. Concretely, PCS reflects PF, RP, BP, and GH. MCS reflects VT, SF, RE, and MH. RCS reflects RP, GH, SF, and RE. The summary score can be compared with norm, and the standard score of the norm is 50. The data were compared between patients treated with zigzag incision and those patients treated with conventional curvilinear incision. Twenty-nine questionnaires were returned, among which two were excluded because of incomplete data. Comparisons were performed between 13 patients as a control group (median age, 62 years; range, 45-70 years; 9 females, 4 males) and 14 patients as a zigzag group (median age, 58 years; range 40-69 years; 10 females, 4 males). We calculated a 3-component summary score, consisting of the PCS, MCS, and RCS, and performed statistical analysis of the data using Student's t-test and Fisher's exact test. Before using Student's t-test, we confirmed that the null hypothesis that the data with each component score from SF36v2 had come from a normally distributed population could not be rejected using the Shapiro-Wilk test.
In all analyses, P < 0.05 was taken to indicate statistical significance.
RESULTS
The method described here had excellent cosmetic results. The average additional time to perform this procedure was about 20 min, which was mainly due to elongation of the scar. No complications associated with wounds, such as infection or leakage of cerebrospinal fluid (CSF) occurred. All cases included in this study is listed in
Figure 3
SF36v2 summary score PCS: Physical Component score MCS: Mental Component score RCS: Role Social Component score The bar chart indicates the component summary score based on the norm. The average score based on the norm is 50. RCS is significantly higher in the zigzag group than the control group (P = 0.0436)
DISCUSSION
With the development of novel instruments and deeper knowledge of anatomy, treatment of neurological disorders is becoming less invasive. Interventional radiology is no longer an alternative to clipping surgery, and has become the mainstream form of treatment for cerebral aneurysms. This method is less invasive in that it does not manipulate the complex and fragile brain tissue directly. However, cosmetic issues in that do not leave scarring of the skin, which contributes largely to patients’ preference for endovascular surgery, although radiation-induced permanent alopecia due to endovascular treatment occurs in a considerable proportion of cases.[
Zigzag bicoronal incisions have been reported for cosmetic purposes, and they were mainly for the maneuvering of skin and bone pathology. Munro et al. first described zigzag incision in 1993.[
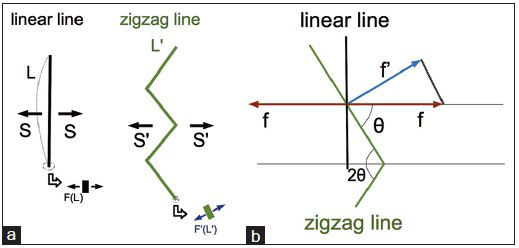
Figure 4
a: The total stress (S) needed to reapproximate the total length of the linear skin incision (L) can be described as linear integration of the stress (F(L)) at each very short length of the incision (dL) S = ∫L F(L)dL. If the condition of the skin on each side of the scar is the same, as the total length of the zigzag incision (L') becomes larger, the f’(L’)dL can be smaller, as the total stress (S’) is equal to S. f’(L’)
Fisher et al. addresses the main disadvantage of this zigzag incision; in that it takes a longer time to perform, and devised a simple reproducible method to plan the incision and part the hair using a template.[
There are two conventional methods for frontotemporal craniotomy, that is, the single-layer method and the two-layer method. In the single-layer method, the skin, galea, temporal muscle, and periosteum are simultaneously cut along the same line by a scalpel or monopolar electrode, and the periosteum is then dragged and the skin flap is turned over. In contrast, the two-layer method requires full exposure of the anterior part of the temporal muscle and fascia, and then provides adequate exposure of the temporopolar lesion or temporal base. However, it sometimes causes moderate or severe atrophy of the temporal muscle.[
Therefore, we combined 1.5-layer method with zigzag incision as mentioned earlier. It is also beneficial to prevent infection of the surgical site compared with the conventional single-layer technique, as the closure line changes with each anatomical layer. SF36v2 Health Survey consists of 36 questions to measure functional health and wellbeing from the patient's point of view. It is a practical, reliable, and valid measure of physical and MH. Moreover, it is a norm-based scoring, which enables us to compare specific groups with general population. The two-component model gave PCS scores and MCS, while the three-component model gave PCS, MCS, and also the third component, the RCS.
Suzukamo et al. confirmed the validity of this three-component scale in 2011.[
Pitfalls and complications
There were no complications associated with wounds in this aneurysm surgery cohort, but as the skin incision was longer than the conventional curvilinear incision, the operation time was longer. There was also an increase in oozing from the skin, and therefore subcutaneous epinephrine injection and meticulous hemostasis were required. In conventional aneurysm surgery, the STA or inherent collateral arterial network of the scalp is sufficient to supply the skin flap, even when a zigzag design is employed. However, if the aneurysm requires some revascularization with the STA, which is not unusual in this endovascular era, it would be better to adopt the conventional skin incision as the tip of the angle may become ischemic after depletion of the STA.
Limitations
The primary limitations of this study were the small sample size and the statistical comparison with a historical cohort. It would be better to design a randomized control trial to compare the QOL according to the method of skin incision.
CONCLUSION
Zigzag incision with 1.5-layer method is an easy, safe, feasible, and useful method to increase the cosmetic satisfaction of patients.
References
1. Akita S, Hirano A. Modified coronal incision: Distribution of stress in the scalp and cranium. Cleft Palate Craniofac J. 1993. 30: 382-6
2. Borges AF. Unsatisfactory forehead scar following face lift. Plast Reconstr Surg. 1986. 78: 526-7
3. de Andrade Junior FC, de Andrade FC, de Araujo Filho CM, Carcagnolo Filho J. Dysfunction of the temporalis muscle after pterional craniotomy for intracranial aneurysms. Comparative, prospective and randomized study of one flap versus two flaps dieresis. Arq Neuropsiquiatr. 1998. 56: 200-5
4. Fisher DM, Goldman BE, Mlakar JM. Template for a zigzag coronal incision. Plast Reconstr Surg. 1995. 95: 614-5
5. Fox AJ, Tatum SA. The coronal incision: Sinusoidal, sawtooth, and postauricular techniques. Arch Facial Plast Surg. 2003. 5: 259-62
6. Kaplan B, Potter T, Moy RL. Scar revision. Dermatol Surg. 1997. 23: 435-42
7. Leach P, Rutherford S, Likhith A, Leggate J. Zig-zag bicoronal scalp incision for cranio-facial cases in paediatric neurosurgery. Childs Nerv Syst. 2004. 20: 483-4
8. Mori K, Osada H, Yamamoto T, Nakao Y, Maeda M. Pterional keyhole approach to middle cerebral artery aneurysms through an outer canthal skin incision. Minim Invasive Neurosurg. 2007. 50: 195-201
9. Mori K, Yamamoto T, Nakao Y, Oyama K, Esaki T, Watanabe M. Lateral supraorbital keyhole approach to clip unruptured anterior communicating artery aneurysms. Minim Invasive Neurosurg. 2008. 51: 292-7
10. Munro IR, Fearon JA. The coronal incision revisited. Plast Reconstr Surg. 1994. 93: 185-7
11. Nathal E, Gomez-Amador JL. Anatomic and surgical basis of the sphenoid ridge keyhole approach for cerebral aneurysms. Neurosurgery. 2005. 56: 178-85
12. Park J, Hwang YH, Kim Y. Extended superciliary approach for middle cerebral artery embolectomy after unsuccessful endovascular recanalization therapy: Technical note. Neurosurgery. 2009. 65: E1191-4
13. Peterson EC, Kanal KM, Dickinson RL, Stewart BK, Kim LJ. Radiation-induced complications in endovascular neurosurgery: Incidence of skin effects and the feasibility of estimating risk of future tumor formation. Neurosurgery. 2013. 72: 566-72
14. Sekiya T, Iwabuchi T, Okabe S, Takiguchi M, Oda N. Facial nerve preservation in the region of the zygomatic arch. No Shinkei Geka. 1990. 18: 1029-33
15. Suzukamo Y, Fukuhara S, Green J, Kosinski M, Gandek B, Ware JE. Validation testing of a three-component model of Short Form-36 scores. J Clin Epidemiol. 2011. 64: 301-8
16. Wilbrand JF, Schaaf H, Howaldt HP, Christophis P. Sinusoidal coronal incision. J Craniofac Surg. 2011. 22: 2278-80