- David Geffen School of Medicine at UCLA, Los Angeles, California, United States,
- University of California, Los Angeles, California, United States,
- Department of Neurosurgery, Shanghai Children’s Medical Center Affiliated to Shanghai Jiaotong University School of Medicine, Shanghai, China,
- Department of Neurosurgery, David Geffen School of Medicine at UCLA, Los Angeles, California, United States.
Correspondence Address:
Jorge Lazareff
David Geffen School of Medicine at UCLA, Los Angeles, California, United States,
Department of Neurosurgery, David Geffen School of Medicine at UCLA, Los Angeles, California, United States.
DOI:10.25259/SNI_358_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Julia Zhuyu Guo1, Ning Yao2, Nan Bao3, Jorge Lazareff1,4. Effects of parental level of income and visual presentation of spina bifida occulta in decision making process. 05-Sep-2020;11:271
How to cite this URL: Julia Zhuyu Guo1, Ning Yao2, Nan Bao3, Jorge Lazareff1,4. Effects of parental level of income and visual presentation of spina bifida occulta in decision making process. 05-Sep-2020;11:271. Available from: https://surgicalneurologyint.com/surgicalint-articles/10246/
Abstract
Background: Parents are active participants in the referral process of children with non-life-threatening surgical pathologies. Nonetheless, there is scarce literature about the influence of parent’s level of income and perception of their children’s conditions on their decision process. Our study aims at expanding our knowledge about this parameter. We focused our research on parents of children spina bifida occulta (SBO), a condition that with a broad clinical impact and that often requires timely referral.
Methods: Questionnaires in Mandarin were administered to parents of patients presenting to the neurosurgery clinic of a children’s hospital in Shanghai. Participants were grouped according to the level of income, above and below 50,000 Yuan. The SBO was classified into two groups, with and without evident subcutaneous mass.
Results: One hundred and forty-five participants completed the questionnaire. Regardless of the type of lesion, families with lower income attributed their concerns for seeking care to their local physicians and the lack of health resources. Families with higher income exhibited fear of treatment. The lower income cohort presented for treatment at an older age than a higher income group. Patients with subcutaneous mass presented for treatment at a younger age than those that did not exhibit mass.
Conclusion: Parental social economic background and visual presentation of SBO have to be factored when analyzing their decision-making process when seeking care for their children. Parental factors can be barriers to surgical care. Healthcare providers must bring parents to the forefront of the treatment process.
Keywords: Barriers to care, Parental perception, Socioeconomic status, Spina bifida occulta
INTRODUCTION
Medical literature has explored the physician parental interaction in cases where life and death decisions are required, such as hospice care or experimental treatment for cerebral neoplasm.[
Neurosurgical textbooks define the treatment algorithm for neural tube defects (NTDs): spina bifida aperta (SBA) has to be repaired as soon as feasible, whereas children born with spina bifida occulta (SBO) do not carry a similar level of urgency. SBO does not represent an immediate threat to the child’s life, as could be with SBA. Nonetheless, the presence of an SBO implies the almost certain danger of neurological disorder secondary to tethering of the spinal cord later on. The debate about the indications of preventive untethering of the cord is still current with two diametral opposed lines of thought.[
MATERIALS AND METHODS
Participants
The study was approved by the Institutional Review Board and conducted at the one of the children’s hospitals in Shanghai, People’s Republic of China (PRC). This hospital is one of the tertiary care centers for pediatric neurosurgery in the PRC. Parents of the pediatric patients presenting to the neurosurgery clinic for any stage of treatment of SBO were eligible for the study.
Questionnaire administration
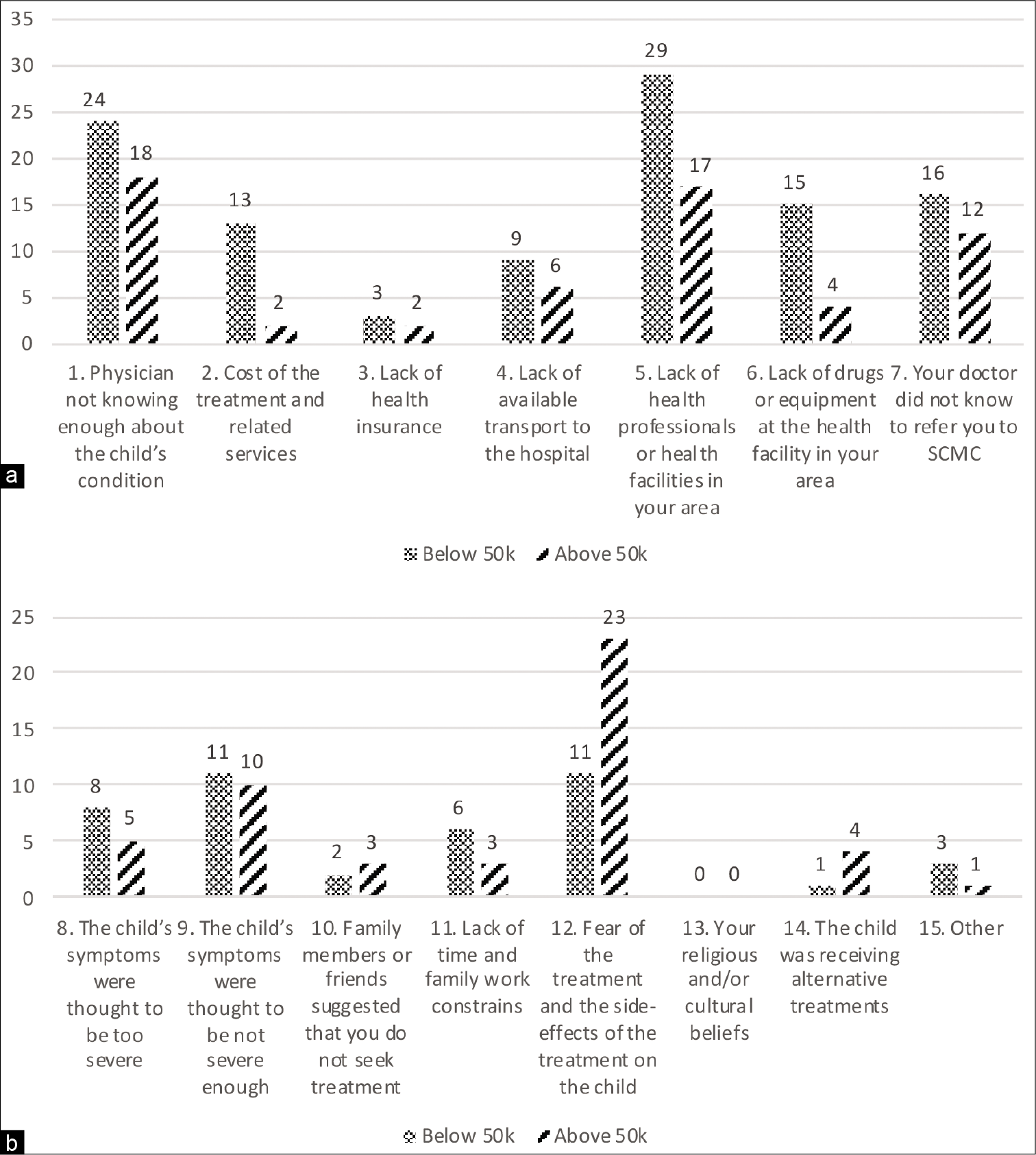
The questionnaire was written in Chinese and administered to the participants along with proper verbal consent. Two interviewers fluent in Mandarin Chinese conducted the questionnaire. The questionnaire was completely anonymous, and participants were instructed to not include any identifiers. The participants were allowed to select as many concerns as they deemed appropriate regarding seeking care for their children with SBO. Concerns #1–7 are classified as infrastructural while #8–14 are classified as personal [
Classification of SBO groups and income
The SBO presentations were classified into Group 1, conditions with subcutaneous mass (lipomyelomeningocele, meningocele, and spinal lipoma), and Group 2, conditions without a subcutaneous mass (caudal agenesis, dermal cyst, dermal sinus, diastematomyelia, intradural lipoma, tethered spinal cord, and tight filum terminale). Parents were classified into lower income (LI, annual household income below 50,000 Yuan) versus higher income (HI, annual household income above 50,000 Yuan).
RESULTS
Demographics
A total of 145 questionnaires were completed. Seventy-six cases fell into Group 1 while 69 cases belonged to Group 2. Fifty-four cases (37%) reported an annual household income to be <50,000 Yuan while 83 cases (57%) reported an annual household income to be more than 50,000 Yuan. Eight cases (6%) did not report the annual household income. Seven (13%) of the 54 LI cases were from Shanghai, while 47 (87%) of the LI cases were from non-Shanghai areas. Nineteen (23%) of the 83 HI cases were from Shanghai, and 64 (77%) of HI cases were from non- Shanghai areas.
Parental concerns based on income
Within the LI cohort, the two most chosen concerns were #1 (n = 24, physician not knowing enough about the child’s condition) and #5 (n = 29, lack of health professionals or health facilities in your area). In families with HI, concern #12 (n = 23, fear of treatment and side-effects of treatment on the child) was the most commonly chosen [
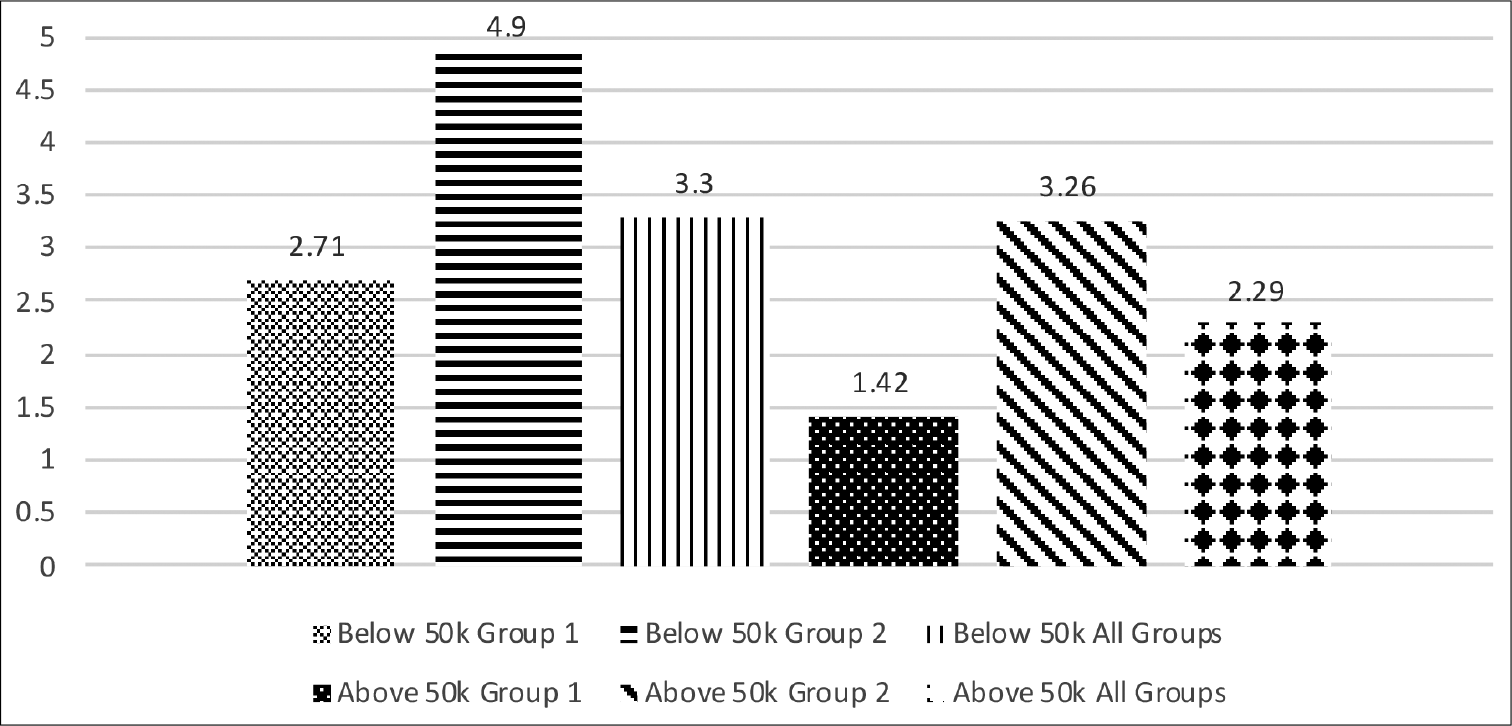
Age of presentation to the hospital based on income and SBO group
The average age of presentation to this hospital for the treatment of SBO for the LI cohort was 3.3 years, while that of the HI cohort was 2.29 years. Within the LI cohort, patients with Group 1 SBOs presented at 2.71 years while Group 2 SBO patients presented at 4.9 years. Within the HI cohort, Group 1 patients presented on average at the age of 1.42 years while Group 2 patients presented at the age of 3.26 years [
DISCUSSION
We conducted our study at a children’s hospital in Shanghai, PRC. The PRC has one of the highest incidences of NTDs.[
Our results revolve around a well-known concept; the SES of patients links to the gradients of health.[
Parental income in relation to types of parental concerns
The infrastructural concerns, #1 (lack of knowledge by the physicians) and #5 (lack of health professionals or health facilities), yielded the highest responses in the LI group. If we assume that each parent is an active participant in their child’s care, we understand that it is reasonable to view them as a potential barrier to care. Grimes et al. emphasized that the lack of infrastructure and insufficient knowledge from the local physician looped together with insufficient anesthesiologist are the main impediments to successful treatment.[
HI parents focused on concern #12 (fear of the treatments), a non infrastructural concern. These parents were fearful of the treatment and its side effects of on their children. We speculate that when parents have less socioeconomic resources, they prioritize having access to care for their children, beyond the issues related to a single child with a unique pathology. With more advantageous socioeconomic status, the quality of treatment to the individual becomes more important to the parents.
Presentation of SBO in relation to age of presentation
The physical appearance of the lesion likely contributes to the parental perception of the urgency to obtain treatment, which plays a crucial role in the speed of diagnosis. The innocent appearance of the skin over some of the SBO lesions belies its importance to the parents and often leads to delayed arrival to a tertiary treatment center. Understandably, patients with visible subcutaneous mass presented to the clinic at a younger age than those that did not have a subcutaneous mass. The economic divide was present here, too; patients from families with higher income presented to the clinic at a younger age than patients with lower parental income. In fact, children from HI group had a visible subcutaneous lesion presented almost 3½ years earlier than children from LI and had no visible subcutaneous mass [
In addition, the spiritual believe was not checked by any of the participants (concern #13), regardless of parental level of income and the visibility of a subcutaneous mass. Perhaps this is related to not urgent appearance of SBO as perceived by the parents. What is prevalent in the literature are the papers on the believes of parents when their opinion is required about discontinuation of life support.[
CONCLUSION
We acknowledge that it is not possible to know how many parents opted for not seeking specialized care. We also acknowledge that the results of our study in one hospital in one country and with one pathology should not be generalized to every other country. Nonetheless, the relevance of parental socioeconomic history and perception of the sickness can be considered universal. The SES of patients links to the gradients of health and the physician is aware of such disparity.[
Perhaps, the most consistent interpretation of our findings is that it expands the personality of the parents from what can be called the “Lockean imperative.” The role of the parents of a sick child is often considered as a unidirectional interaction between them and the physician. The parents are bound to do what is the best interest for their children. The ideal parents were described by Locke centuries ago in the “Two Treatises of Government;” “The power, then, that parents have over their children arises from that duty, which is incumbent on them, to take care of their offspring, during the imperfect state of childhood. To inform the mind, and govern the actions of their yet ignorant nonage, till reason shall take its place and ease them of that trouble, is what the children want, and the parents are bound to.”[
There is a social dimension to the problem of spina bifida. The pathology is less frequent in upper income countries (UICs), where the average is about 0.7/1000 live births than in LMIC, where it can be as prevalent at 6/1000 live births. The medical cannon maintains that the most potent factor that affects the incidence of spina bifida of any form is a folic acid deficiency. Epidemiologists and obstetricians recommend that before pregnancy, women start a regime of 400–800 μg of folic acid/day. Interestingly, the concentration of folic acid in the cereal box sold in UIC is below the recommended for effective prevention. Indeed, a yearlong supply of folic acid is in nobody’s wedding list. Thus, we cannot say that the majority of the population fills the dietary requirement.
Nonetheless, the data showing a decrease of NTD in UIC are compelling. Thus, many LMIC adopted the model, but not with similar success. This fact begs the question about the existence of other factors prevalent in LMIC, such as chronic malnutrition linked to a high incidence of poverty. Maybe we should not log onto folic acid alone the role of a catalyst for the closure of the neural tube. The identification of the other factors prevalent in LMIC relevant for NTD is a task that is the responsibility of native neurosurgeons and epidemiologists. Such a multifactorial job is not for somebody who practices in a UIC. Many parents in our study complained about the attitude toward the patients by primary care doctors. One of us has developed an information booklet about spina bifida to distribute among patients and primary care physicians. Our Chinese colleagues received the text of the brochure and modified it into its final version and will continue adapting it according to the response from pediatricians and other health care workers. As stated at the beginning of this paragraph, there is a social dimension to the problem of spina bifida. Our work addressed just a tiny portion of the vast landscape.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
David Geffen School of Medicine at UCLA provided travel stipend.
Conflicts of interest
There are no conflicts of interest.
References
1. Allen KA. Parental decision-making for medically complex infants and children: An integrated literature review. Int J Nurs Stud. 2014. 51: 1289-304
2. Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: A systematic review. J Am Board Fam Pract. 2002. 15: 25-38
3. Campion A, Lee C, Bao N, Lazareff J. A parental perspective concerning barriers to care for neural tube defects in China. Surg Neurol Int. 2017. 8: 195
4. Field KS, Briggs DJ. Socio-economic and locational determinants of accessibility and utilization of primary health-care. Health Soc Care Community. 2001. 9: 294-308
5. Fildes L.editors. The Doctor. London: Tate Gallery; 1891. p.
6. Gabe J, Olumide G, Bury M. “It takes three to tango”: A framework for understanding patient partnership in paediatric clinics. Soc Sci Med. 2004. 59: 1071-9
7. Grimes CE, Bowman KG, Dodgion CM, Lavy CB. Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg. 2011. 35: 941-50
8. Jackson C, Cheater FM, Reid I. A systematic review of decision support needs of parents making child health decisions. Health Expect. 2008. 11: 232-51
9. Just AC. Parent participation in care: Bridging the gap in the pediatric ICU. Newborn Infant Nurs Rev. 2005. 5: 179-87
10. La Marca F, Grant JA, Tomita T, Mclone DG. Spinal lipomas in children: Outcome of 270 procedures. Pediatr Neurosurg. 1997. 26: 8-16
11. Locke J.editors. Two Treatises of Government. London: Peacock Books; 1993. p.
12. Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008. 358: 2468-81
13. Mckenna K, Collier J, Hewitt M, Blake H. Parental involvement in paediatric cancer treatment decisions. Eur J Cancer Care. 2010. 19: 621-30
14. Michelson KN, Koogler T, Sullivan C, Ortega MD, Hall E, Frader J. Parental views on withdrawing life-sustaining therapies in critically ill children. Arch Pediatr Adolesc Med. 2009. 163: 986-92
15. Parker RM, Gazmararian JA. Health literacy: Essential for health communication. J Health Commun. 2003. 8: 116-8
16. Pierre-Kahn A, Zerah M, Renier D, Cinalli G, Sainte-Rose C, Lellouch-Tubiana A. Congenital lumbosacral lipomas. Childs Nerv Syst. 1997. 13: 298-334
17. Verlinde E, Laender ND, Maesschalck SD, Deveugele M, Willems S. The social gradient in doctor-patient communication. Int J Equity Health. 2012. 11: 12
18. Zhu L, Ling H. National neural tube defects prevention program in China. Food Nutr Bull. 2008. 29: S196-204