- Neurology and Electroneuromyography Clinic, Oneonta, New York, USA
Correspondence Address:
R. P. Lazaro
Neurology and Electroneuromyography Clinic, Oneonta, New York, USA
DOI:10.4103/2152-7806.163816
Copyright: © 2015 Lazaro RP. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Lazaro RP. Electromyography in musculoskeletal pain: A reappraisal and practical considerations. Surg Neurol Int 28-Aug-2015;6:143
How to cite this URL: Lazaro RP. Electromyography in musculoskeletal pain: A reappraisal and practical considerations. Surg Neurol Int 28-Aug-2015;6:143. Available from: http://surgicalneurologyint.com/surgicalint_articles/electromyography-in-musculoskeletal-pain-a-reappraisal-and/
Abstract
Background:Patients with musculoskeletal pain (MSP) and local tenderness in the back and extremities are frequently referred to electromyography (EMG) laboratory to assess the integrity of the spinal nerve roots, peripheral nerves, and skeletal muscles. When focal muscle weakness and anatomical sensory deficits are clinically evident, this procedure is almost always abnormal. In some situations, when the presenting symptoms consist of local pain and tenderness without neuromuscular deficits, its diagnostic utility becomes questionable as illustrated in the present study.
Methods:EMG findings of 75 patients referred for evaluation of local MSP and tenderness in the neck and lower back and in the upper and lower extremities were reviewed. These patients were selected from a group of 200 patients referred for evaluation of unilateral local pain and tenderness in various parts of the body. All EMG procedures and clinical neurologic examination were performed by the author and all underwent magnetic resonance imaging of the affected parts of the body prior to the procedure. None of the 75 patients studied had concurrent medical disorders or had previous spinal root injuries or surgeries to the spine.
Results:All 75 patients in this study showed normal EMG of the affected extremities and normal peripheral nerve conduction study. Those with herniated disc in the cervical or lumbar spine presenting with local pain and tenderness in the neck and lower back but without neurologic deficits or clear radicular symptoms, had normal study also. The remaining 125 patients excluded from the study, had various EMG and peripheral nerve abnormalities that can be attributed to concurrent medical disorders and previous injuries to the spinal roots.
Conclusions:Use of EMG in the diagnosis of local MSP, unless associated with clinical neurologic deficits, almost always yields negative results. The utility of this procedure is limited to pathology in the motor unit. It cannot assess the function of the sensory components of the spinal roots, small-diameter sensory nerves, and the sensory innervation of the spine via sinuvertebral nerve. Therefore, if the motor unit is anatomically and physiologically intact, the procedure is of little value in the diagnosis of MSP. Likewise, peripheral nerve conduction study is likely to be normal unless clear neurologic deficits are present. The present study illustrates that a good history and meticulous neurologic examination should be an integral part of an ideal electrodiagnostic procedure.
Keywords: Electromyography, musculoskeletal pain, neck and back pain
INTRODUCTION
Needle electromyography (EMG) is a well-established procedure used frequently to diagnose conditions presenting with pain and various sensory symptoms in the spine and extremities and to explain the etiology of focal or diffuse muscle weakness. It is usually performed in conjunction with peripheral nerve conduction studies to diagnose entrapment neuropathies or polyneuropathies. Musculoskeletal pain (MSP), defined as local pain and tenderness in the soft tissues, spine, and joints, is a common symptom that brings patients to EMG laboratory for evaluation. In general, depending on clinical symptomatology, emphasis is focused on EMG to diagnose radiculopathy, plexopathy and myopathy, or on a peripheral nerve conduction study to diagnose peripheral neuropathy. The usefulness of EMG in MSP with the normal clinical neuromuscular examination and without clearly defined sensory deficits is re-assessed in this communication. The impetus that led to this retrospective study stemmed from an inordinate number of normal EMG studies in uncomplicated MSP elicited by the author in the past several years.
MATERIALS AND METHODS
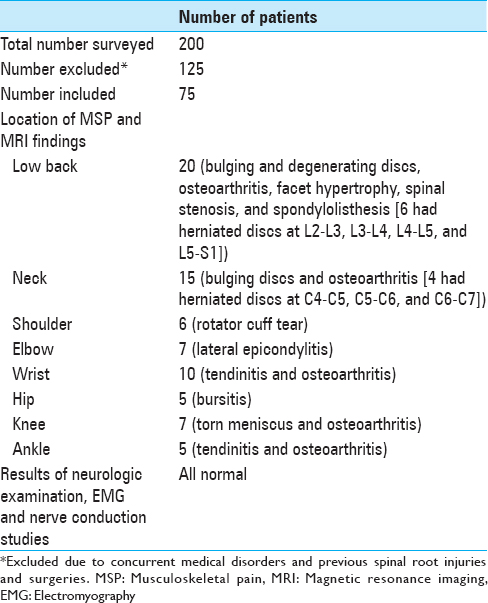
Records of 75 patients ages 30–60 (45 males and 30 females) who underwent EMG and peripheral nerve conduction study in the past 7 years, were reviewed. They were selected from a group of 200 patients who were referred by their primary care providers and surgical specialists for evaluation of MSP in the neck, lower back, and extremities [
Of the 75, presenting symptoms were low back and neck pain (20 and 15 patients, respectively) associated with no-anatomical or nondermatomal paresthesias without sensory loss or focal muscle weakness in the affected extremity; and unilateral local pain and tenderness in the joints and soft tissues in the shoulder (6), elbow (7), wrist (10), hip (5), knee (7), and ankle (5). All patients with low back and neck pain were either occupational or related to vehicular accidents. Those with regional MSP in either upper or lower extremity were of uncertain origin. All patients were examined clinically and electrophysiologically, at least 3 months after onset of the symptoms.
Monopolar needle electrodes were used in all patients. Abnormal EMG was defined as presence of signs of active denervation (sharp positive waves and fibrillation potentials) alongside excessive complex motor units. Presence of rare complex units, absence of active denervation, and full activation of motor units during maximal contraction in association with completely normal clinical neurologic examination, was not considered an abnormal study. Minimum of four muscles (deltoid, triceps, brachioradialis and first dorsal interosseous for the upper extremity and vastus medialis, biceps femoris, tibialis anterior, and medial gastrocnemius for the lower extremity) and maximum of six muscles, using five quadrant sampling as tolerated, were tested in the affected extremity. Paraspinal muscle sampling was also performed as tolerated or was avoided in patients with severe low back or neck pain and muscle spasm.
Peripheral nerve conduction studies were performed using the standard technique for percutaneous nerve stimulation and recording with surface electrodes. H-reflex study along with either tibial or peroneal motor nerve and sural nerve conduction studies were performed for patients presenting with low back pain and with nonanatomical or nondermatomal paresthesias or cool sensation in the affected extremity. In the upper extremity, the median and ulnar motor and sensory nerve conduction studies were performed. Measurement of late responses via F-wave latency determination was not routinely performed since this technique can only assess the motor components of the neural axis. Moreover, elicitation of F-wave requires several supramaximal stimulation that can be quite unpleasant to patients already suffering from MSP.
Magnetic resonance imaging (MRI) studies ordered by the referring health care providers prior to EMG study were reviewed. MRI findings included degenerating and bulging discs, facet hypertrophy, osteoarthritis, spinal stenosis, spondylolisthesis, rotator cuff tear, lateral epicondylitis, tendinitis, bursitis, and torn meniscus. Ten patients had herniated discs in various levels, four in the cervical (C4–C5, C5–C6, and C6–C7) and six in the lumbar (L3–L4, L4–L5, and L5–S1) spine.
RESULTS
None of the muscles sampled in all 75 patients, including 10 patients with cervical and lumbar herniated discs, showed EMG abnormalities. Clinically, those patients with herniated discs had normal muscle stretch reflexes and normal muscle tone and power. They had no sensory loss, fasciculations, or muscle atrophies. Low back pain that intensified with prolonged sitting or standing along with a limited range of motion correlated with the presence of either degenerating or bulging discs in the lumbar spine. None of the patients with various MRI findings in the cervical and lumbar spine and extremities had an abnormal neurologic examination. Local pain and tenderness in various parts of the affected extremities, some with swelling and limited range of motion of the affected joints, were not associated with neuromuscular deficits or signs of complex regional pain syndrome. Their EMG and peripheral nerve conduction study were normal.
DISCUSSION
Anatomically, a motor unit consists of anterior horn cell and its axon along with muscle fibers innervated by the terminal branches of this axon. Any lesion affecting any segment of the motor unit proximally and distally, will generate abnormal action potentials in EMG along with clinical motor deficits affecting specific myotomes or muscles innervated by a peripheral nerve.[
Of relevance in this discussion is the utility of EMG in MSP regardless of location. MSP may be accompanied by vague paresthesias without clear anatomical distribution in the affected limb and is frequently the presenting symptoms in musculoskeletal stress injuries in the workplace. Unless associated with focal muscle weakness or atrophy, EMG in these situations will likely yield negative results. The reason is obvious. MSP is the result of irritation of small-diameter A-delta and C-fiber sensory nerves.[
Presence of a herniated disc (or other abnormalities in the vertebra) does not necessarily lead to abnormal neurologic examination or EMG abnormalities, in fact, 10 of the patients studied showed otherwise. All these patients had no radicular symptoms, but had prominent MSP that were indicative of axial or mechanical injury rather than injury to the spinal nerve root as evidenced by normal clinical and EMG examination. Even in situations when a herniated disc is associated with sensory and motor deficits in the affected extremity, axial pain, and MSP remain the more prominent and disabling symptoms in most patients with back or neck injury thereby underscoring the pathophysiologic relevance of the sinuvertebral nerve in the generation of back pain. An abnormal EMG in those with motor deficits would only reflect the effect of spinal nerve root impingement by the herniated disc, but not the pain related to irritation of the sinuvertebral nerve, a pure sensory nerve.
EMG, in general, can be a painful and uncomfortable procedure. Some purists will go as far as sampling the paraspinal muscles despite the presence of severe back pain and spasm in pursuit of EMG diagnosis. Multiple muscles, and, therefore, multiple needle punctures, are frequently sampled in an effort to elicit an abnormality. Others will rely on clinical examination and limit muscle sampling to a minimum. When the clinical history and clinical examination are diagnostic of a radiculopathy or focal neuropathy and corroborated by an imaging study, some practitioners find EMG unnecessary.
The presence of EMG “abnormalities” in cases of uncomplicated MSP with normal neurologic examination can lead to diagnostic and therapeutic obfuscation. They may also lead to inappropriate medicolegal claims following trauma to the musculoskeletal system. Thus, any EMG report must be interpreted in conjunction with the clinical history and examination and awareness of the limitations of this procedure.
Cost of an EMG procedure is worthy of consideration. Expense for a comprehensive procedure with peripheral nerve conduction study may range from $400 to $800. Thus, misuse of this procedure is a threat to health care cost. However, there are obvious situations when the cost is justified by a comprehensive procedure. This can occur when local MSP is complicated by concurrent medical or neuromuscular disorder, symptoms of which, some patients may not be aware of. A good neurological history and examination, however, can easily detect such occurrence. On the other hand, an unwary electromyographer can only make the situation confusing to the referring health care provider when reporting an abnormal EMG study.
There are important and intriguing questions that are worthy of serious considerations. Does a clinician-electromyographer have an obligation to proceed and perform the procedure knowing that the diagnosis is already obvious clinically and radiologically, and that the results are likely to be normal? Is it necessary to sample multiple muscles in the affected extremity or perform peripheral nerve conduction study if the presenting symptom is a localized MSP without sensory and motor deficits? If the diagnosis or radiculopathy is already obvious, is it necessary to sample the very tender and tense paraspinal muscles simply to localize the lesion electrophysiologically at the expense of patient's comfort? Multiple factors such as differences in medical judgment and referring physician's approach to health care, medicolegal issues, and clinician-electromyographer's training and diagnostic orientation, can only generate more questions whose answers are complex and controversial.
The results of this study should behoove any clinicians and surgeons to realize that needle EMG cannot assess sensory symptoms – particularly pain – directly; and that this procedure can only assess the components of the peripheral motor system. On the other hand, a negative study can still be diagnostically helpful and reassuring, thus, providing the referring health care providers valuable guide to the treatment of MSP. It is also equally helpful to know that an abnormal EMG and/or abnormal peripheral nerve conduction study can co-exist with MSP thereby providing incontrovertible evidence of peripheral neural process, symptoms of which can be masked by severe musculoskeletal symptoms, particularly MSP.
References
1. Brenn D, Richter F, Schaible HG. Sensitization of unmyelinated sensory fibers of the joint nerve to mechanical stimuli by interleukin-6 in the rat: An inflammatory mechanism of joint pain. Arthritis Rheum. 2007. 56: 351-9
2. Cavanaugh JM, Ozaktay AC, Yamashita T, Avramov A, Getchell TV, King AI. Mechanisms of low back pain: A neurophysiologic and neuroanatomic study. Clin Orthop Relat Res. 1997. 335: 166-80
3. Chen C, Lu Y, Kallakuri S, Patwardhan A, Cavanaugh JM. Distribution of A-delta and C-fiber receptors in the cervical facet joint capsule and their response to stretch. J Bone Joint Surg Am. 2006. 88: 1807-16
4. Daube JR, Rubin DI. Needle electromyography. Muscle Nerve. 2009. 39: 244-70
5. Edgar MA. The nerve supply of the lumbar intervertebral disc. J Bone Joint Surg Br. 2007. 89: 1135-9
6. Nakamura SI, Takahashi K, Takahashi Y, Yamagata M, Moriya H. The afferent pathways of discogenic low-back pain. Evaluation of L2 spinal nerve infiltration. J Bone Joint Surg Br. 1996. 78: 606-12
7. Takebayashi T, Cavanaugh JM, Kallakuri S, Chen C, Yamashita T. Sympathetic afferent units from lumbar intervertebral discs. J Bone Joint Surg Br. 2006. 88: 554-7