- Department of Neurosurgery, University of Baghdad - College of Medicine, Baghdad, Iraq,
- Department of Neurosurgery, Alfaisal University - College of Medicine, Riyadh, Saudi Arabia,
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq,
- Department of Neurosurgery, University of King Abdulaziz - College of Medicine, Jeddah, Saudi Arabia,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
DOI:10.25259/SNI_1168_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammad SA1, Albulaihed SA2, Ismail M3, Alshuqayfi KM4, Farooq IA1, Al-Ageely TA1, Palmisciano P5, Andaluz N5, Hoz SS5. Endolymphatic sac: A surreptitious anatomy for neurosurgeons. Surg Neurol Int 03-Feb-2023;14:42
How to cite this URL: Mohammad SA1, Albulaihed SA2, Ismail M3, Alshuqayfi KM4, Farooq IA1, Al-Ageely TA1, Palmisciano P5, Andaluz N5, Hoz SS5. Endolymphatic sac: A surreptitious anatomy for neurosurgeons. Surg Neurol Int 03-Feb-2023;14:42. Available from: https://surgicalneurologyint.com/surgicalint-articles/12137/
Dear Editor,
INTRODUCTION
The endolymphatic sac (ES) is an essential structure in the field of otorhinolaryngology, while it can be seen as a hidden corner from neurosurgical perspectives. The ES is a small epithelial-lined channel, considered a non-sensory organ related to the inner ear. The available literature on neurosurgical pathologies and their relation to ES is scattered with a noticeable paucity. In this paper, we attempt to give an overview of the anatomical description, potential functions, and applications of the ES in neurosurgery.
Gudziol and Guntinas-Lichius tapped into the historical journey of the endolymphatic structures, starting from Huscke in 1824 to Hensen in 1880. Their exploration of the Labyrinth, besides its possible connection to the intracranial structures, paved the way to be followed later by WeberLiel (1823–1891) and their proof of their theory.[
PERTINENT ANATOMY OF ES
The ES represented a segment of the membranous labyrinth, a part of the inner ear composed of two other parts, including the osseous labyrinth and the otic capsule.[
ANATOMICAL VARIATIONS AND RELATIONS OF ES
Regarding the ES size, variation exists as the mean width of the sac was 12 mm, and the mean length of its superior and inferior borders was 12 mm and 11 mm, respectively.[
Highlighting the relation of ES to the sigmoid sinus has been mentioned in different studies, as a study by Lo WW et al. showed that in up to 40% of the cases, the distal part of the ES overlaps the sigmoid sinus.[
Regarding the vasculature of the ES, the arterial blood supply appears to be from the occipital artery.[
The function of ES is based on its location. As part of the labyrinth, it serves the purposes of regulating the volume and pressure of the endolymph, modulating the immune response of the inner ear, and eliminating the endolymphatic waste products by phagocytosis. However, the precise function of the sac is a point of controversy.
PATHOLOGIES RELATED TO THE ES
Lesions related to the ES can vary; an example is the ES tumors which were categorized together with adenomatous tumors of the middle ear and the mastoid air sinus until 1984 when Hassard et al. first described an extradural papillary lesion that was adherent to the ES.[
There are many lesions affecting the ES reported in the literature. For example, if a tumor is found in the endolymphatic duct, it is considered an extremely rare tumor at the base of the skull. It does not have clear-cut clinical guidelines and can be encountered sporadically from the lymph-epithelium within the vestibular duct, which is characterized by locally aggressive papillary tumors of the petrous bone, which may be sporadic or associated with Von Hippel-Lindau (VHL) disease. However, they can rarely occur in individuals who do not have mutation or deletion of the VHL gene.[
Radiographic features of ES include the following; generally, ES tumors always arise within the VA [
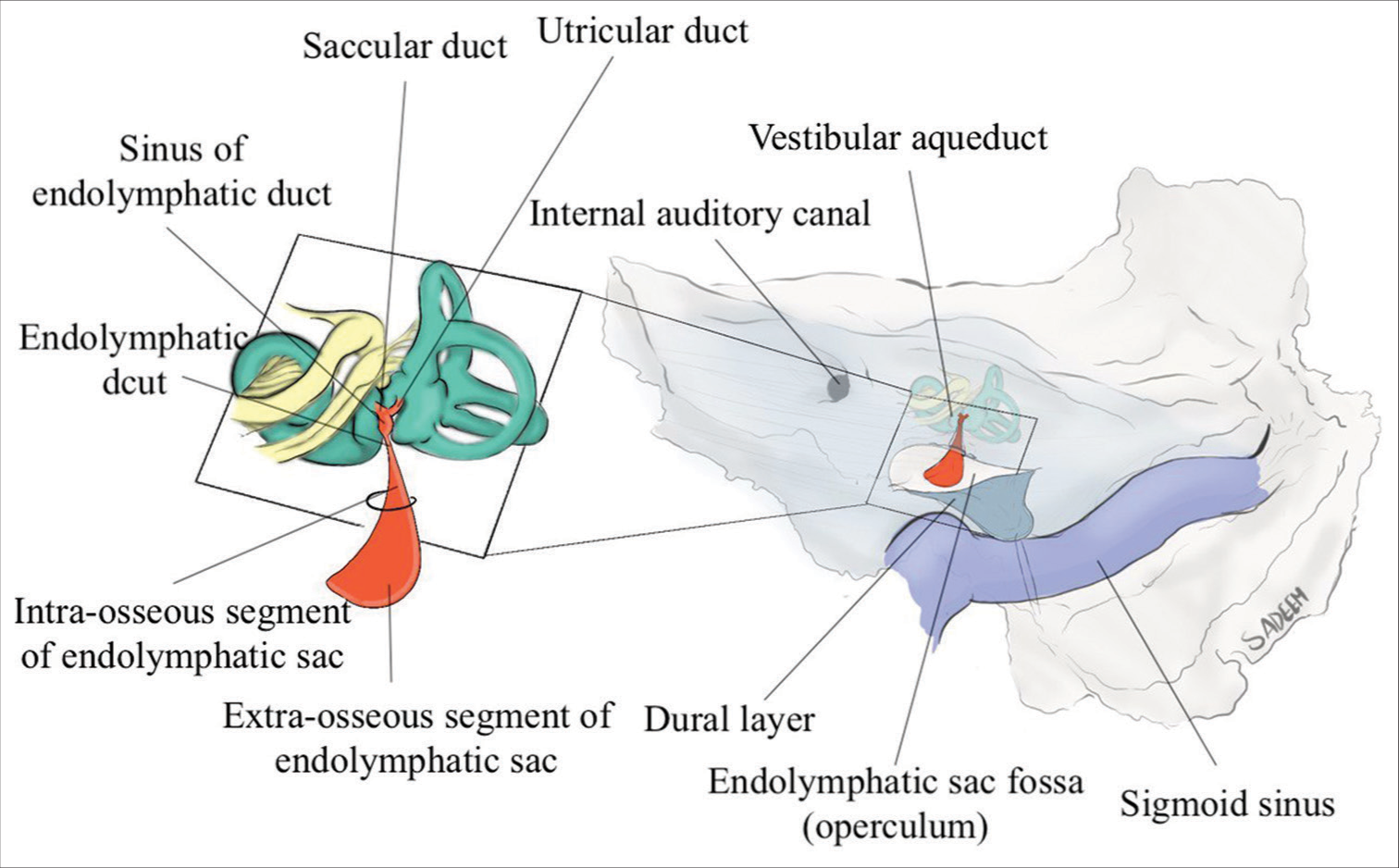
Figure 1:
A schematic illustration (the posterior view of the posterior surface of the right petrous temporal bone) detailing the anatomy of the endolymphatic system and its relationship to the surrounding petrous bone; The endolymphatic duct is connected to the membranous labyrinth of the inner ear by the saccular and utricular ducts. The saccular and utricular ducts form the sinus of the endolymphatic duct. The sinus of the endolymphatic duct tapers and becomes the isthmus of the endolymphatic duct as it enters the bony vestibular aqueduct. The isthmus of the endolymphatic duct connects it to the intra-osseous portion (within the vestibular aqueduct) of the endolymphatic duct. Endolymphatic sac tumors arise from the endolymphatic epithelium of the endolymphatic duct with the vestibular aqueduct (osseous portion, striped area); the vestibular aqueduct is considered the site of origin of endolymphatic sac tumors. Distally, the extra-osseous portion of the endolymphatic sac begins as the sac exits the aperture of the vestibular aqueduct. The extra-osseous portion of the sac resides between the leaves of the posterior fossa dura mater on the posterior wall of the petrous ridge.
Early detection of these tumors is critical for surgical intervention and may prevent further hearing loss. ES tumors do not metastasize but are highly locally aggressive.[
SUMMARY
The ES can be considered an overlooked structure and not fully understood location and function for the general community in neurological surgery. Its location at the junction of the petrous bone and mastoid process renders the ES a potential route for tumors to invade the inner ear canal or spread to the middle and posterior cranial fossa.[
CONCLUSION
ES is a structure related to the inner ear and can be an asset to the auditory function. It might be an overlooked structure, particularly regarding the value of its pertinent anatomy, variation, pathologies, and operative nuances. The sigmoid sinus renders the ES a critical structure in the operative cavity of the related approaches.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bagger-Sjöbäck D, Jansson B, Friberg U, Rask-Andersen H. Three-dimensional anatomy of the human endolymphatic sac. Arch Otolaryngol Head Neck Surg. 1990. 116: 345-9
2. Bambakidis NC, Rodrigue T, Megerian CA, Ratcheson RA. Endolymphatic sac tumor metastatic to the spine. J Neurosurg. 2005. 3: 68-70
3. Bausch B, Wellner U, Peyre M, Boedeker CC, Hes FJ, Anglani M. Characterization of endolymphatic sac tumors and von Hippel-Lindau disease in the international endolymphatic sac tumor registry. Head Neck. 2016. 38: E673-9
4. Becker W, Naumann HH, Pfaltz CR, editors. Hals-Nasen-OhrenHeilkunde: Kurzgefasstes Lehrbuch mit Atlasteil, differential Diagnostische Tabellen, 250 Prüfungsfragen. Stuttgart, New York: Thieme; 1986. p.
5. Carlson ML, Thom JJ, Driscoll CL, Haynes DS, Neff BA, Link MJ. Management of primary and recurrent endolymphatic sac tumors. Otol Neurotol. 2013. 34: 939-43
6. Donaldson JA. Normal anatomy of the inner ear. Otolaryngol Clin North Am. 1975. 8: 267-9
7. Friberg U, Jansson B, Rask-Andersen H, Bagger-Sjöbäck D. Variations in surgical anatomy of the endolymphatic sac. Arch Otolaryngol Neck Surg. 1988. 114: 389-94
8. Gadre AK, Fayad JN, O’leary MJ, Zakhary R, Linthicum FH. Arterial supply of the human endolymphatic duct and sac. Otolaryngol Neck Surg. 1993. 108: 141-8
9. Gudziol H, Guntinas-Lichius O. Contributions of the Anatomist Emil Huschke to Otorhinolaryngology. ISIS. 1831. p. 950-1
10. Gussen R. Endolymphatic hydrops with absence of vein in Para vestibular canaliculus. Ann Otol Rhinol Laryngol. 1980. 89: 157-61
11. Hassard AD, Boudreau SF, Cronn CC. Adenoma of the endolymphatic sac. J Otolaryngol. 1984. 13: 213-6
12. Heffner DK. Low-Grade adenocarcinoma of probable endolymphatic sac origin. A clinicopathologic study of 20 cases. Cancer. 1989. 64: 2292-302
13. Lo WW, Daniels DL, Chakeres DW, Linthicum FH, Ulmer JL, Mark LP. The endolymphatic duct and sac. Am J Neuroradiol. 1997. 18: 881-7
14. Locke RR, Shaw-Dunn J, O’Reilly BF. Endolymphatic sac surgical anatomy and transmastoid decompression of the sac for the management of Ménière’s disease. J Laryngol Otol. 2014. 128: 488-93
15. Manski TJ, Heffner DK, Glenn GM, Patronas NJ, Pikus AT, Katz D. Endolymphatic sac tumors: A source of morbid hearing loss in von Hippel-Lindau disease. JAMA. 1997. 277: 1461-6
16. Marlan R. Hansen, William M. Luxford surgical outcomes in patients with endolymphatic sac tumor Laryngoscope. 2004. 114: 1470-4
17. Patel NP, Wiggins RH, Shelton C. The radiologic diagnosis of endolymphatic sac tumors. Laryngoscope. 2006. 116: 40-6
18. Pollak A, Bohmer A, Spycher M, Fisch U. Are papillary adenomas endolymphatic sac tumors?. Ann Otol Rhinol Laryngol. 1995. 104: 613-9
19. Shambaugh GE. Surgery of the endolymphatic sac. Arch Otolaryngol. 1966. 83: 305-15