- Department of Neurosurgery, Ibn Sina Hospital, Al-Sabah Medical Area, Kuwait.
Correspondence Address:
Waleed Azab, Department of Neurosurgery, Ibn Sina Hospital, Al-Sabah Medical Area, Kuwait.
DOI:10.25259/SNI_1249_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Waleed Azab, Mustafa Najibullah, Ghada Waheed. Endoscope-controlled extended supraorbital keyhole approach through a modified eyebrow incision for a large dural-based solitary fibrous tumor of the frontal convexity: A technical note. 15-Apr-2022;13:153
How to cite this URL: Waleed Azab, Mustafa Najibullah, Ghada Waheed. Endoscope-controlled extended supraorbital keyhole approach through a modified eyebrow incision for a large dural-based solitary fibrous tumor of the frontal convexity: A technical note. 15-Apr-2022;13:153. Available from: https://surgicalneurologyint.com/surgicalint-articles/11530/
Abstract
Background: The extended supraorbital approach through a modified eyebrow incision is a minimally invasive approach that has been recently described. It entails a lateral extension of the skin incision beyond the lateral end of the eyebrow and allows exposure of the proximal sylvian fissure with a superior degree of surgical freedom in the middle fossa and the parasellar region. In this technical note, we describe an endoscope-controlled extended supraorbital keyhole approach with modified eyebrow incision for excision of a large dural-based solitary fibrous tumor of the left frontal convexity.
Methods: An endoscope-controlled extended supraorbital keyhole approach with modified eyebrow incision was performed to excise a large extra-axial mass attached to the dura of the left frontal convexity and extends from the superior temporal line up to the midline in a 34-year-old male patient presented with 1-year history of headache, dizziness, and blurred vision.
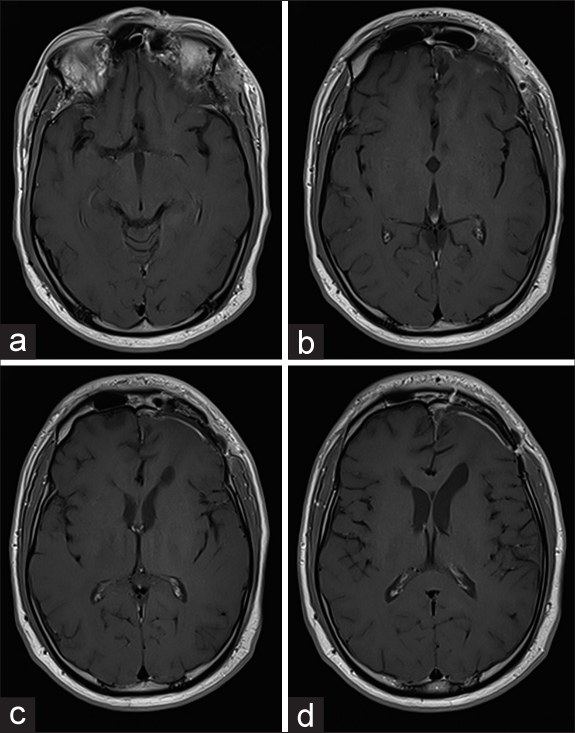
Results: The patient had an uneventful postoperative course with gross total excision of the lesion and satisfying cosmetic appearance. Histopathological examination revealed a Grade 1 solitary fibrous tumor.
Conclusion: We demonstrated the feasibility of the endoscope-controlled extended supraorbital keyhole approach through a modified eyebrow incision for excision of tumors that abut the inner table of the frontal calvarial bone, extend highly above the skull base level, or extend medially reaching the midline. The approach is very versatile and allows a great exposure for a category of lesions deemed not perfectly suitable for the classic supraorbital keyhole approach.
Keywords: Endoscopic, Eyebrow, Keyhole, Solitary fibrous tumor, Supraorbital
INTRODUCTION
The supraorbital eyebrow approach is a minimally invasive approach that allows an excellent access to many pathologies located in the anterior cranial fossa, suprasellar, and parasellar regions.[
In this technical note, we describe an endoscope-controlled extended supraorbital keyhole approach with modified eyebrow incision for excision of a large dural-based solitary fibrous tumor of the left frontal convexity and demonstrate that the combination of the extended exposure and the use of the angled rigid endoscopes add greatly to the versatility of the approach.
CLINICAL PRESENTATION
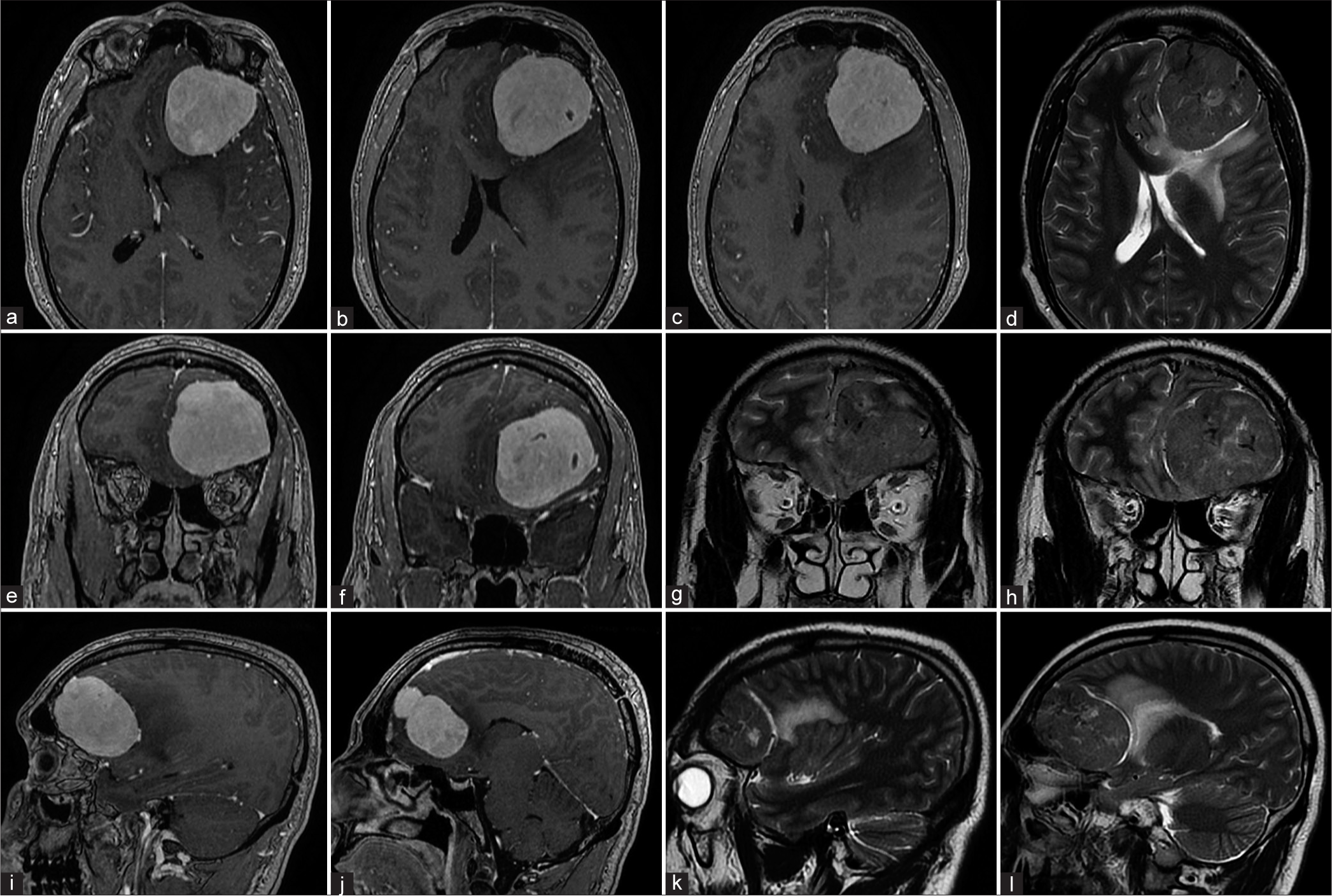
A previously healthy 34-year-old male patient presented with 1-year history of headache, dizziness, and blurred vision. He had no history of trauma, seizures, or loss of consciousness. Neurological examination was normal except for Grade 4 papilledema. Magnetic resonance imaging of the brain [
Figure 1:
Preoperative magnetic resonance imaging. Serial images in axial (a-d), coronal (e-h), and sagittal planes (i-l) reveal a left frontal extra-axial mass based on the convexity dura. The mass avidly enhanced after contrast medium injection (a-c, e, f, i and j). At the level of the frontal skull base, the lesion extended from the superior temporal line laterally to reach the midline medially. Note the extent of the frontal air sinus in relation to the tumor base (a-c). In T2-wighted images (d, g-f, and k-l), a well-defined arachnoid plane is present between the tumor and the surrounding brain. Significant perifocal vasogenic edema is seen to involve the rostrum and genu of the corpus callosum as well as the frontal white matter.
Surgical technique
Under general anesthesia with the patient in supine position, the head was secured in a MAYFIELD skull clamp® and rotated 30° to the right. The head was then extended 15° with a slight contralateral lateral flexion to help providing easier instrument maneuverability during the procedure.
Skin incision
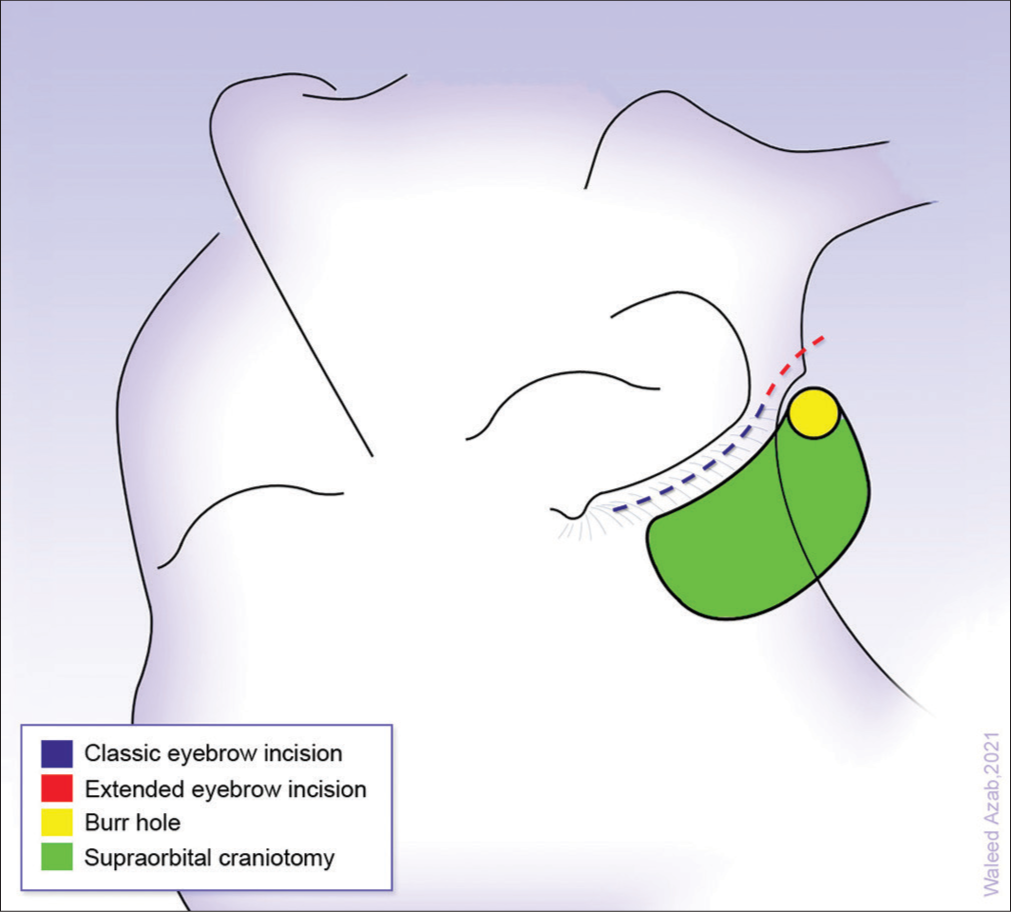
The skin incision was made within the eyebrow and started just lateral to the supraorbital notch and continued for further 15 mm within a skin crease after the lateral end of the eyebrow. At the superior temporal line, the temporalis fascia was incised for about 2 cm then the frontalis fascia is cut from the temporal line in a semicircular fashion over the frontal bone with its base at the orbital rim. The temporalis muscle is subsequently dissected off the bone and retracted posteriorly for 2 cm [
Craniotomy
A single burr hole was made using a sharp pit attached to the high-speed drill in the temporal fossa lateral to the superior temporal line at a point that is slightly higher than the classic MacCarty’s burr hole. A craniotome is then used to perform a 4 × 3 cm bone flap. The frontal air sinus was deliberately open. Although this should usually be avoided, it was necessary in our case because of the large lateral extension of the sinus and the tumor medial extent toward the midline.
Dural opening and tumor resection
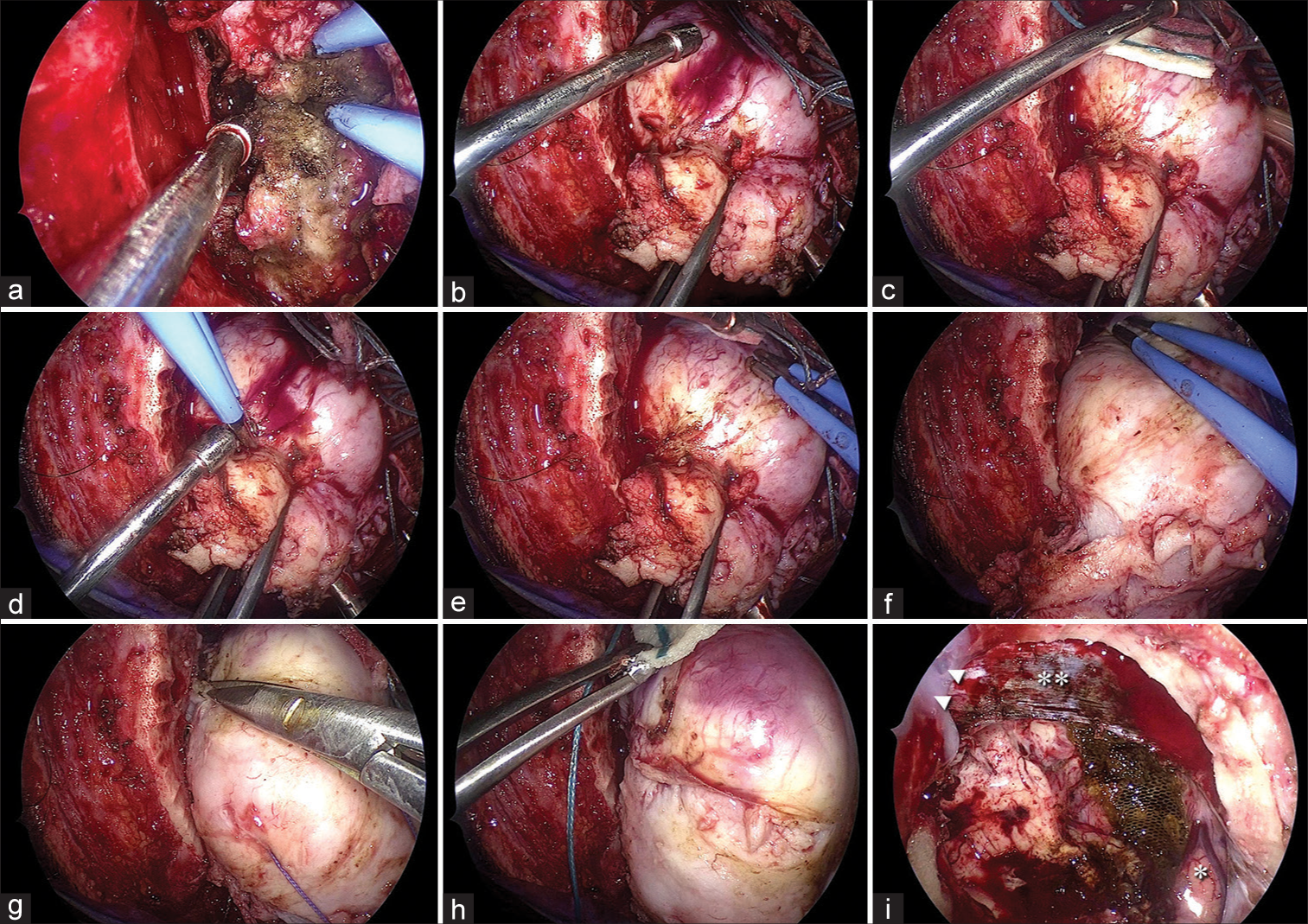
In
Figure 4:
Intraoperative views during tumor excision under endoscopic control. (a) The tumor has been centrally debulked. Bipolar coagulation within the tumor is undertaken to control bleeding. (b and c) Tumor is grasped reflected toward the debulked center and cottonoid patties are inserted into the plane between tumor and brain. (d and e) Further tumor capsule is exposed and vessels on the surface are coagulated. Coagulation (f) and cutting (g) of the inferior attachment of the tumor capsule are then undertaken and a cottonoid patty is inserted before the tumor is removed (h). (i) Final hemostasis of the tumor bed has been undertaken and the normal brain at the upper extent of the tumor cavity (asterisk), falx cerebri (double asterisks), and Tisseel used for closure of the frontal air sinus (arrowheads) is viewed.
The tumor was encountered immediately on dural removal. Central debulking was undertaken and the tumor outer capsule was grasped and gently pulled toward the centrally debulked area to help developing a dissection plane between the tumor and brain. Cottonoid patties were used to maintain the circumferentially developed plane around the tumor. Bipolar coagulation was used to coagulate the vessels on the gradually exposed tumor surface. Attachment to skull base dura was freed and the tumor was removed en bloc.
Closure
The opened frontal sinus mucosa was coagulated and an autologous fat graft was used to obliterate its cavity. Surgicel® was used to support the fat graft and Tisseel® glue was used to seal the frontal sinus. Artificial dura was then used to close the dural defect and the bone flap was returned and secured with titanium plates and screws. Wound closure is then undertaken in the usual manner.
DISCUSSION
The extended supraorbital approach through a modified eyebrow incision is a minimally invasive approach that has been recently described and is essentially a modification of the classic supraorbital eyebrow keyhole approach. It entails a lateral extension of the skin incision beyond the end of the eyebrow and allows exposure of the proximal sylvian fissure with a superior degree of surgical freedom in the middle fossa and the parasellar region without large compromise of the cosmetic outcome.[
The extent of exposure
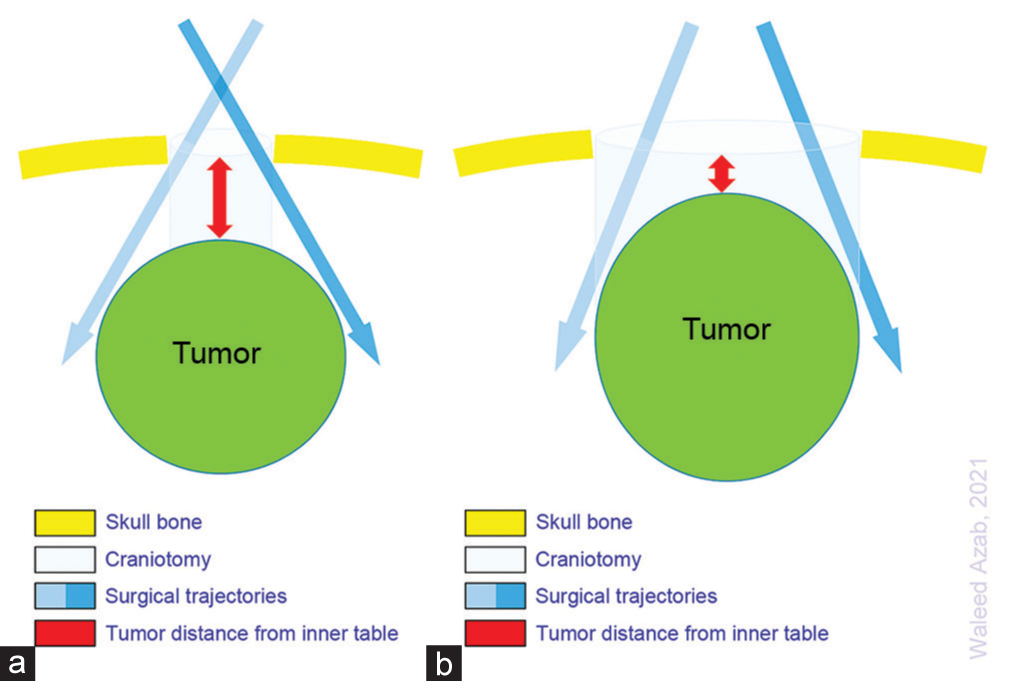
According to the keyhole principle, lesions located near the surface of the brain typically require a bony opening as large as the lesion, while deeper lesions can often be removed through a much smaller craniotomy [
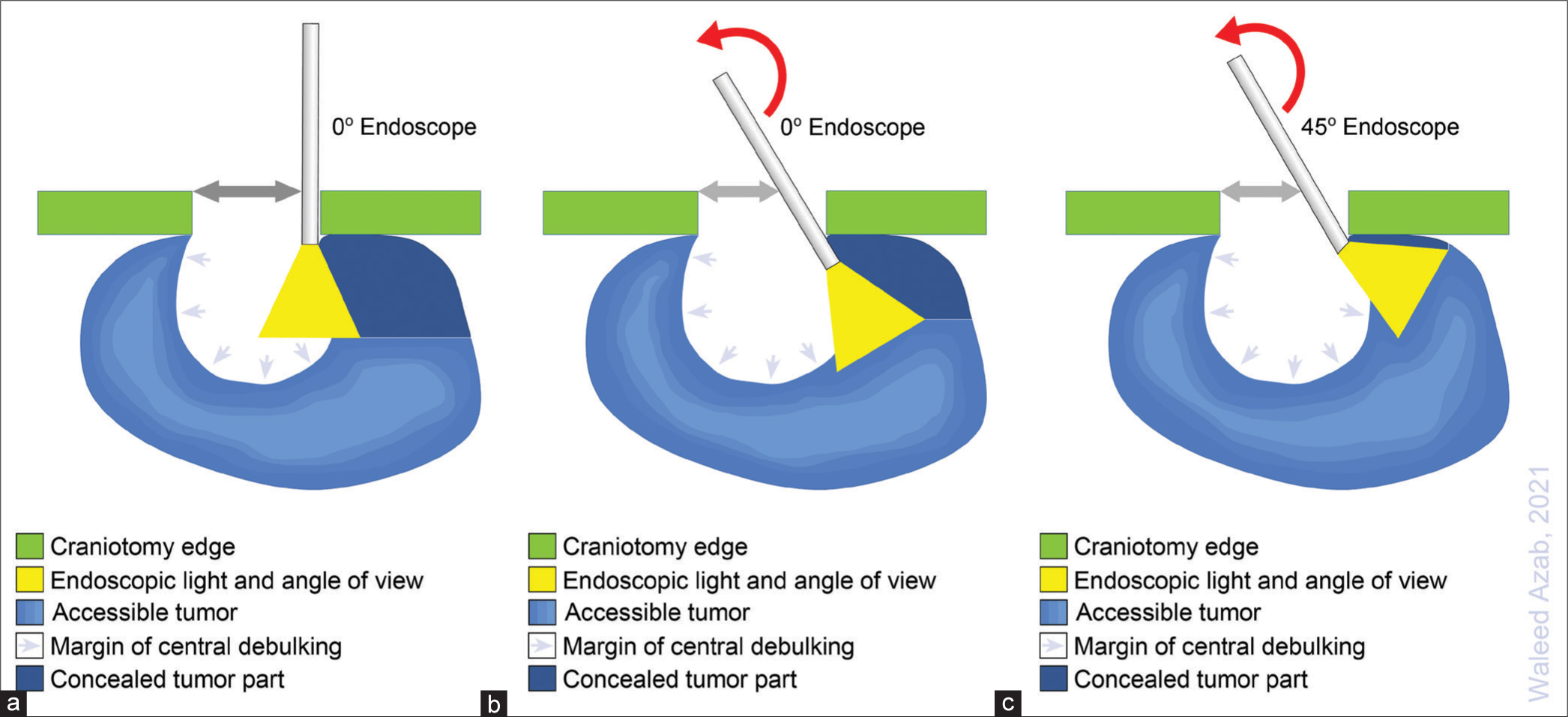
Figure 6:
The significance of combining the relatively larger craniotomy offered by the extended supraorbital keyhole approach with endoscopic control. After initial central debulking, the 0° endoscope allows further tumor visualization and removal within the scope’s field of view. Remaining tumor parts under the surface are, however, not visible (a). Angulating the shaft of the 0° endoscope enables further visualization and removal of these tumor parts while the working space is still uncompromised (b). Replacing the 0° with angled (30° and 45°) scopes further discloses the final remaining tumor tissue under the bone while the working space is still maintained (c). Red curved arrows indicate angulating the endoscope shaft. Grey arrows indicate the craniotomy width utilized for angulating the endoscope shaft.
The use of the endoscope
The use of angled scopes was also critical because it allowed looking under the surface of the craniotomy so that the hidden parts of the tumor and neighboring brain tissue were seen and manipulated [
Despite the fact that surgical microscopes with coaxial slit illumination provide the high magnification and good stereoscopy, using the surgical microscope during a keyhole procedure forces the surgeon to work along the microscope’s line of view.[
Endoscopic control versus endoscopic assistance
Due to the benefits of endoscopic view, endoscopic assistance in supraorbital keyhole approach has by far been the most frequently reported since the early beginnings of using the procedure[
One of the main reasons for relying mainly on the surgical microscope for surgical control during the procedure and using the endoscope as a complimentary visualization tool is that the use of a non-stereoscopic (two-dimensional) endoscope result in loss of depth perception. This issue is easily overcome by moving the scope within the field of view and is usually not very troublesome for surgeons with familiarity with endoscopic use. It is our opinion that the full endoscopic control actually negates the problem of suboptimal visualization associated with a small exposure during the whole procedure. Based on the definite superiority of endoscopic view, it is our belief that the use of rigid endoscopes as the sole viewing tools is worth being more adopted and expanded.
Potential complications and choice of the approach
Avoidance of injury to the temporal branches of the facial nerve was achieved by bringing the incision posteriorly rather than inferiorly after its eyebrow component ends. Furthermore, the subperiosteal dissection of the temporalis muscle off the bone (subperiosteal dissection) is critical in avoiding frontalis branch injury. Although not performed in our case, the use of a neurostimulator to seek out the frontal facial branch once the temporalis muscle fascia is exposed has been described and allows safe dissection from the lateral canthal line back over the temporalis fascia.[
It is of note that other conventional approaches such as frontal, pterional, and mini-pterional approaches can also be utilized in this case. However, in our opinion, the endoscope-controlled extended supraorbital approach through a modified eyebrow incision is the least invasive and the shortest route to the tumor in our patient. Opening the frontal air sinus should of course be avoided; however, meticulous closure using a combination of autologous fat supported by Surgicel® and Tisseel® glue is very effective in preventing CSF leaks. Based on our experience in using this technique for frontal sinus closure, we opted to perform the approach described herein in lieu of the other alternative approaches.
CONCLUSION
We demonstrated the feasibility of endoscope-controlled (purely endoscopic) extended supraorbital keyhole approach through a modified eyebrow incision for excision of tumors that abut the inner table of the frontal calvarial bone, extend highly above the skull base level, and extend medially reaching the midline. The approach is very versatile and allows a great exposure for a category of lesions deemed not perfectly suitable for the classic supraorbital keyhole approach.
Authors’ contributions
All authors contributed equally to the manuscript.
Ethical approval
This is technical note. The Research Ethics Committee in Ibn Sina Hospital has confirmed that no ethical approval is required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ansari SF, Eisenberg A, Rodriguez A, Barkhoudarian G, Kelly DF. The supraorbital eyebrow craniotomy for intra and extra-axial brain tumors: A single-center series and technique modification. Oper Neurosurg (Hagerstown). 2020. 19: 667-77
2. Azab WA, Elmaghraby MA, Zaidan SN, Mostafa KH. Endoscope-assisted transcranial surgery for anterior skull base meningiomas. Mini Invasive Surg. 2020. 4: 88
3. Berhouma M, Jacquesson T, Jouanneau E. The fully endoscopic supraorbital trans-eyebrow keyhole approach to the anterior and middle skull base. Acta Neurochir (Wien). 2011. 153: 1949-54
4. Chen YH, Lin SZ, Chiang YH, Ju DT, Liu MY, Chen GJ. Supraorbital keyhole surgery for optic nerve decompression and dura repair. J Neurotrauma. 2004. 21: 976-81
5. da Costa MD, Hardesty DA, Priddy B, Noiphithak R, Barbero JM, Prevedello DM. Extended supraorbital approach with modified eyebrow incision: Technical note. World Neurosurg. 2019. 128: 354-9
6. Dlouhy BJ, Chae MP, Teo C. The supraorbital eyebrow approach in children: Clinical outcomes, cosmetic results, and complications. J Neurosurg Pediatr. 2015. 15: 12-9
7. Filho LF, McLaughlin N, Bresson D, Solari D, Kassam AB, Kelly DF. Supraorbital eyebrow craniotomy for removal of intraaxial frontal brain tumors: A technical note. World Neurosurg. 2014. 81: 348-56
8. Gazzeri R, Nishiyama Y, Teo C. Endoscopic supraorbital eyebrow approach for the surgical treatment of extraaxialand intraaxial tumors. Neurosurg Focus. 2014. 37: E20
9. Igressa A, Pechlivanis I, Weber F, Mahvash M, Ayyad A, Boutarbouch M. Endoscope-assisted keyhole surgery via an eyebrow incision for removal of large meningiomas of the anterior and middle cranial fossa. Clin Neurol Neurosurg. 2015. 129: 27-33
10. Ivan ME, Lawton MT. Minisupraorbital approach to inferior frontal lobe cavernous malformations: Case series. J Neurol Surg A Cent Eur Neurosurg. 2013. 74: 187-91
11. Kabil MS, Shahinian HK. Application of the supraorbital endoscopic approach to tumors of the anterior cranial base. J Craniofac Surg. 2005. 16: 1070-5
12. Martinez-Perez R, Albonette-Felicio T, Hardesty DA, Carrau RL, Prevedello DM. Same viewing angle, minimal craniotomy enlargement, extreme exposure increase: The extended supraorbital eyebrow approach. Neurosurg Rev. 2021. 44: 1141-50
13. Perneczky A, Reisch R.editors. Keyhole Approaches in Neurosurgery. Vol. I Concept and Surgical Technique. Vienna: Springer; 2008. p.
14. Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005. 57: 242-55
15. Sughrue ME, Teo C, Sughrue ME, Teo C.editors. Cognitive principles of planning keyhole approaches. Principles and Practice of Keyhole Brain Surgery. Stuttgart: Georg Thieme Verlag; 2015. p. 6-9
16. Szabo KA, Cheshier SH, Kalani MY, Kim JW, Guzman R. Supraorbital approach for repair of open anterior skull base fracture. J Neurosurg Pediatr. 2008. 2: 420-3
17. van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: Concept and technique. Surg Neurol. 1998. 49: 481-90
18. Wilson DA, Duong H, Teo C, Kelly DF. The supraorbital endoscopic approach for tumors. World Neurosurg. 2014. 82: e243-56
19. Youngerman BE, Shtayer L, Gerges MM, Larsen AG, Tomasiewicz HC, Schwartz TH. Eyebrow supraorbital keyhole craniotomy for olfactory groove meningiomas with endoscope assistance: Case series and systematic review of extent of resection, quantification of postoperative frontal lobe injury, anosmia, and recurrence. Acta Neurochir (Wien). 2021. 163: 101-12
20. Zumofen DW, Rychen J, Roethlisberger M, Taub E, Kalbermatten D, Nossek E. A review of the literature on the transciliary supraorbital keyhole approach. World Neurosurg. 2017. 98: 614-24