- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan.
- Department of Neurosurgery, Shiroishi Kyoritsu Hospital, Shiroishi, Japan.
- Department of Neurosurgery, Imari Arita Kyoritsu Hospital, Arita, Japan.
Correspondence Address:
Tatsuya Tanaka, Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan.
DOI:10.25259/SNI_268_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tatsuya Tanaka1, Xuan Liu2, Nobuaki Momozaki3, Eiichiro Honda2. Endoscopic-assisted removal of bilateral traumatic intracerebral hemorrhage: A case report. 11-Aug-2023;14:288
How to cite this URL: Tatsuya Tanaka1, Xuan Liu2, Nobuaki Momozaki3, Eiichiro Honda2. Endoscopic-assisted removal of bilateral traumatic intracerebral hemorrhage: A case report. 11-Aug-2023;14:288. Available from: https://surgicalneurologyint.com/surgicalint-articles/12492/
Abstract
Background: Decompressive craniectomy or craniotomy is an effective method for reducing intracranial pressure in patients with traumatic brain injury. However, contralateral intracranial hematoma is a rare but serious complication. Recently, the endoscopic technique has been described as a minimally invasive, safe, and effective treatment for intracranial hematoma evacuation. To the best of our knowledge, no technical report has described bilateral traumatic intracerebral hemorrhage (TICH) evacuation using a neuroendoscope.
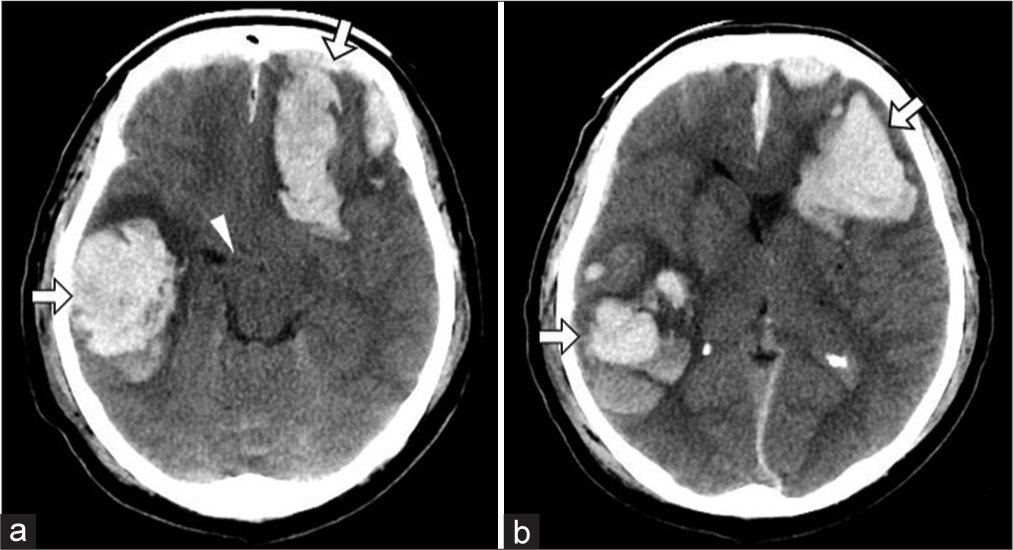
Case Description: A 62-year-old man was admitted to the hospital after a fall due to intoxication. His initial Glasgow Coma Scale (GCS) score was 14. Initial computed tomography (CT) revealed a right temporal skull fracture, bilateral frontal and right temporal tip contusions, and acute subdural hematoma. During admission, his condition deteriorated to a GCS score of 6 points, and follow-up CT showed hemorrhagic progression of left frontal and right temporal contusion with midline shift and brainstem compression. Emergency surgery was performed for TICH in the left frontal lobe and right temporal lobe. A burr hole was made in each of the left frontal and right temporal regions, and we used a neuroendoscope to assist in the evacuation of the hematoma. Postoperative CT showed adequate evacuation of the hematoma. The patient regained consciousness and was discharged after 2 months.
Conclusion: Bilateral TICH was rapidly and sequentially removed by burr-hole craniotomy and endoscopic hematoma evacuation without rapid decompression by craniotomy. The hematoma did not increase. This report demonstrates that the endoscopic-assisted technique allows the safe treatment of bilateral TICH.
Keywords: Bilateral traumatic intracerebral hemorrhage, Burr hole, Endoscopic surgery, Minimally invasive, Traumatic brain injury
INTRODUCTION
Traumatic intracerebral hemorrhage (TICH) is estimated to occur in 25–45% of cases of severe traumatic brain injury (TBI) and in 3–12% of cases of moderate TBI.[
CASE DESCRIPTION
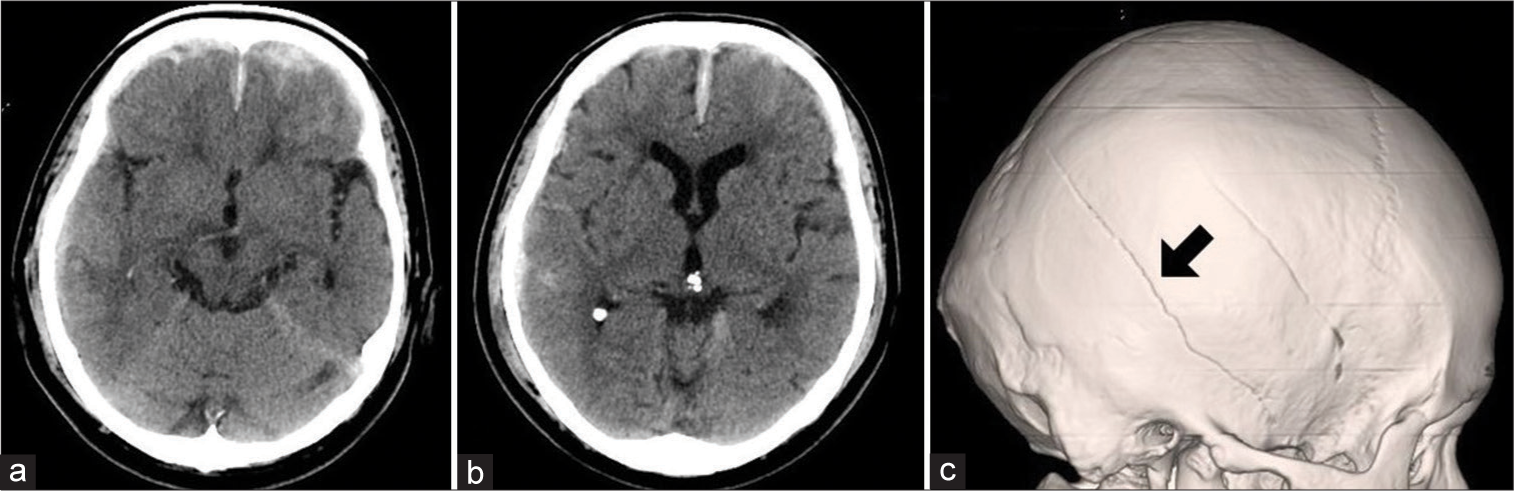
A 62-year-old man with well-controlled hypertension and diabetes was admitted to the hospital after a fall due to intoxication. He lost consciousness after the accident and regained consciousness shortly after arrival at the emergency department. His initial Glasgow Coma Scale (GCS) score was 14 (E4V4M6). Computed tomography (CT) revealed a right temporal skull fracture, bilateral frontal and right temporal tip contusions, and acute subdural hematoma [
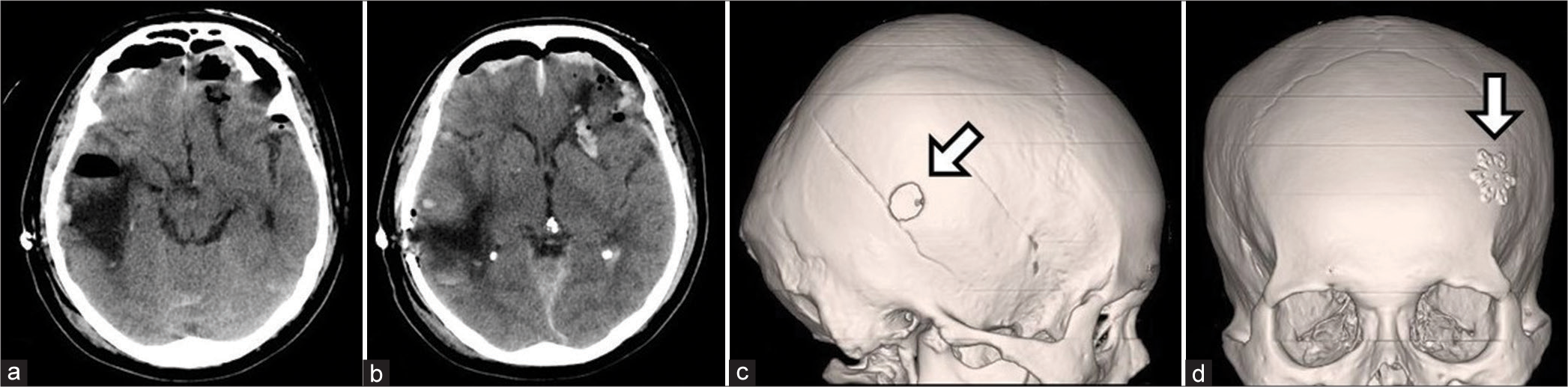
Postoperative CT showed more than 90% TICH removal with adequate decompression [
Figure 3:
Postoperative computed tomography (CT) showing adequate hematoma evacuation (a) and improved midline shift after surgery (b). Three-dimensional CT showing two burr holes made in the right temporal (c, arrow) and left frontal (d, arrow) regions for the endoscopic removal of bilateral traumatic intracerebral hemorrhage.
DISCUSSION
The clinical course and complications associated with TICH and ICH are similar. Following the primary injury, re-bleeding and cerebral edema are the most common significant adverse events.[
We perform endoscopic hematoma removal in the management of TICH, similar to how we routinely manage ICH. In cases of intracranial pressure >20 mmHg after removal of TICH by endoscopic hematoma evacuation, we consider decompressive craniectomy. As the present case had no significant cerebral edema, postoperative neurological recovery was faster.
Extra-axial hematomas (EAH) progress in 22% of patients with TBI at the original frontotemporal site after contralateral decompression surgery (CDS).[
CONCLUSION
Bilateral TICH was rapidly and sequentially removed by burr-hole craniotomy and endoscopic hematoma evacuation without rapid decompression by craniotomy without an increase in the hematoma. Our report demonstrates that bilateral TICH can be safely treated with endoscopic-assisted techniques.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bullock R, Golek J, Blake G. Traumatic intracerebral hematoma-which patients should undergo surgical evacuation? CT scan features and ICP monitoring as a basis for decision making. Surg Neurol. 1989. 32: 181-7
2. Chen P, Deng YB, Hu X, Zhou W, Zhang QT, Zhang LY. Risk factors associated with the progression of extra-axial hematoma in the original frontotemporoparietal site after contralateral decompressive surgery in traumatic brain injury patients. Chin J Traumatol. 2020. 23: 45-50
3. Masuno A, Katayama H, Wada H, Morikawa K, Tanaka K, Tanaka H. Significance of consecutive bilateral surgeries for patients with acute subdural hematoma who develop contralateral acute epi-or subdural hematoma. Surg Neurol. 2003. 60: 23-30 discussion 30
4. Mohindra S, Mukherjee KK, Gupta R, Chhabra R, Gupta SK, Khosla VK. Decompressive surgery for acute subdural haematoma leading to contralateral extradural haematoma: A report of two cases and review of literature. Br J Neurosurg. 2005. 19: 490-4
5. Oh MJ, Jeong JH, Shin DS, Hwang SC, Im SB, Kim BT. Postoperative contralateral hematoma in patient with acute traumatic brain injury. KoreanJ Neurotrauma. 2017. 13: 24-8
6. Patel NY, Hoyt DB, Nakaji P, Marshall L, Holbrook T, Coimbra R. Traumatic brain injury: Patterns of failure of nonoperative management. J Trauma. 2000. 48: 367-75 discussion 374-5
7. Scaggiante J, Zhang X, Mocco J, Kellner CP. Minimally invasive surgery for intracerebral hemorrhage. Stroke. 2018. 49: 2612-20
8. Shih FY, Chang HH, Wang HC, Lee TH, Lin YJ, Lin WC. Risk factors for delayed neuro-surgical intervention in patients with acute mild traumatic brain injury and intracranial haemorrhage. World J Emerg Surg. 2016. 11: 13
9. Shen J, Pan JW, Fan ZX, Zhou YQ, Chen Z, Zhan RY. Surgery for contralateral acute epidural hematoma following acute subdural hematoma evacuation: Five new cases and a short literature review. Acta Neurochir (Wien). 2013. 155: 335-41
10. Su TM, Lan CM, Lee TH, Hsu SW, Lu CH. Risk factors for the development of contralateral epidural hematoma following decompressive craniectomy in patients with calvarial skull fracture contralateral to the craniectomy site. WorldNeurosurg. 2016. 89: 223-9
11. Sweeney TE, Salles A, Harris OA, Spain DA, Staudenmayer KL. Prediction of neurosurgical intervention after mild traumatic brain injury using the national trauma data bank. World J Emerg Surg. 2015. 10: 23
12. Tanaka T, Goto H, Momozaki N, Honda E. Endoscopic hematoma evacuation for acute subdural hematoma with improvement of the visibility of the subdural space and postoperative management using an intracranial pressure sensor. Surg Neurol Int. 2023. 14: 1
13. Tseng WL, Kuo LT, Chen CM, Yang SH, Tang CT, Lai DM. Surgical application of endoscopic-assisted minimally-invasive neurosurgery to traumatic brain injury: Case series and review of literature. J Formos Med Assoc. 2022. 121: 1223-30
14. Wu R, Shi J, Cao J, Mao Y, Dong B. Two occurrences of delayed epidural hematoma in different areas following decompressive craniectomy for acute subdural hematoma in a single patient: A case report. BMC Surg. 2017. 17: 123






HIROTA Shin
Posted August 16, 2023, 3:42 pm
Thank you for your valuable case presentation. I am troubled by the irregular shape of the traumatic intracerebral hematoma and the difficulty in determining to what extent to remove the contused brain with mixed brain and hematoma. You used a 4mm endoscope instead of 2.6mm. Would the brightness and field of view be useful regarding those above?