- Department of Neurosurgery, Surgery Interest Group of Africa, Abijo, Lagos, Nigeria.
- Department of Research, Surgery Interest Group of Africa, Abijo, Lagos, Nigeria.
Correspondence Address:
Damilola Alexander Jesuyajolu Department of Neurosurgery, Surgery Interest Group of Africa, Abijo, Lagos, Nigeria.
DOI:10.25259/SNI_747_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Damilola Alexander Jesuyajolu1, Abdulahi Zubair1, Armstrong Kpachi Nicholas2, Terngu Moti1, Osamagie Ehi Osarobomwen1, Israel Anyahaebizi1, Charles Okeke1, Samuel Olawale Davis1. Endoscopic third ventriculostomy versus ventriculoperitoneal shunt insertion for the management of pediatric hydrocephalus in African centers – A systematic review and meta-analysis. 14-Oct-2022;13:467
How to cite this URL: Damilola Alexander Jesuyajolu1, Abdulahi Zubair1, Armstrong Kpachi Nicholas2, Terngu Moti1, Osamagie Ehi Osarobomwen1, Israel Anyahaebizi1, Charles Okeke1, Samuel Olawale Davis1. Endoscopic third ventriculostomy versus ventriculoperitoneal shunt insertion for the management of pediatric hydrocephalus in African centers – A systematic review and meta-analysis. 14-Oct-2022;13:467. Available from: https://surgicalneurologyint.com/surgicalint-articles/11932/
Abstract
Background: Ventriculoperitoneal shunt (VPS) insertion and endoscopic third ventriculostomy (ETV) are common surgical procedures used to treat pediatric hydrocephalus. There have been numerous studies comparing ETV and VPS, but none from an African perspective. In this study, we sought to compare outcomes from African neurosurgical centers and review the associated complications.
Methods: The Preferred Reporting Items for Systematic Reviews and Meta-Analyses were used in conducting this study. PubMed, Google Scholar, and African Journal Online were searched. Data on treatment successes and failures for ETV and VPS were pooled together and analyzed with a binary meta-analysis. A clinically successful outcome was defined as no significant event or complication occurring after surgery and during follow-up (e.g., infection, failure, CSF leak, malfunction, and mortality). Seven studies fully satisfied the eligibility criteria and were used in this review.
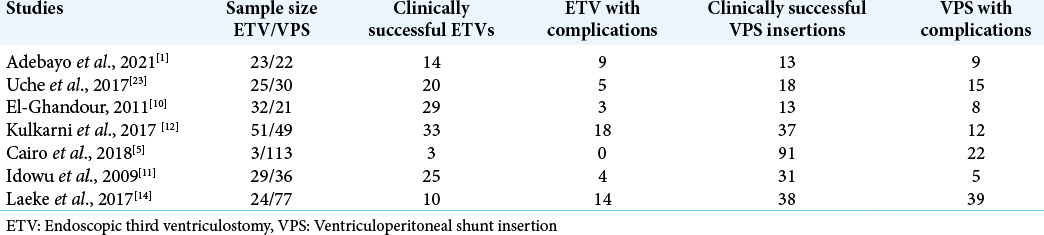
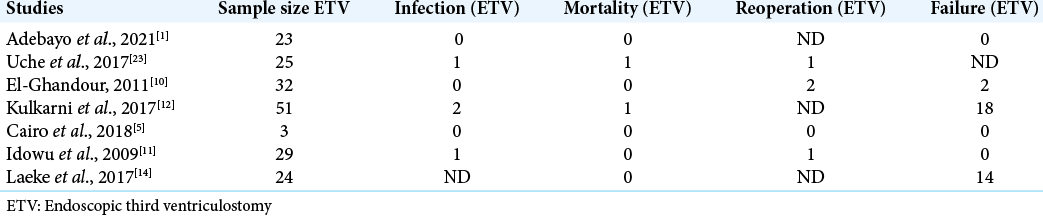
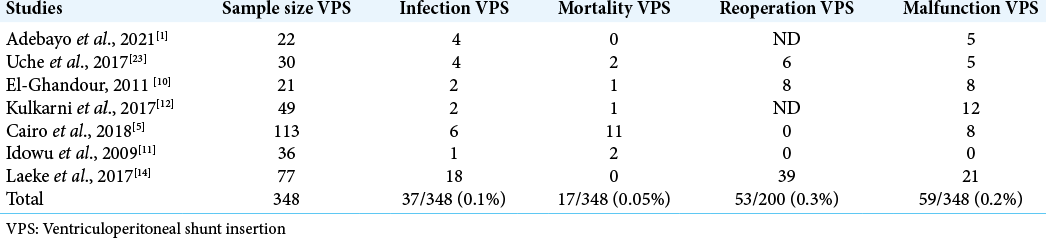
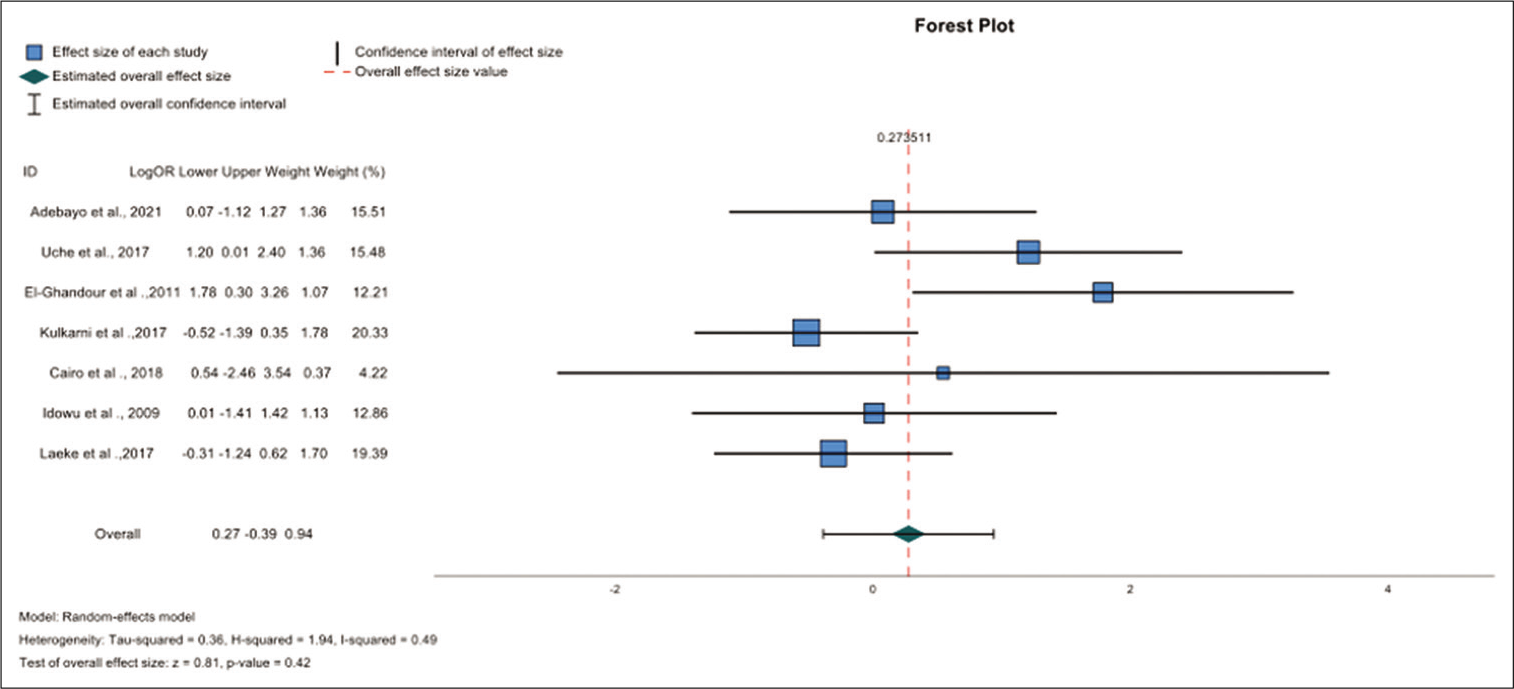
Results: There was no statistically significant difference between the outcomes of ETV and VPS (OR- 0.27; 95% CI −0.39–0.94, P = 0.42). After reviewing the rates of complications of ETV and VPS from the identified studies, four were recurrent. The infection rates of ETV versus VPS were 0.02% versus 0.1%. The mortality rates were 0.01% versus 0.05%. The reoperation rates were 0.05% versus 0.3%, while the rates of ETV failure and shunt malfunction were 0.2% versus 0.2%.
Conclusion: This study concludes that there is no significant difference between the outcomes of ETV and VPS insertion.
Keywords: Endoscopy, Infection, Malfunction, Ventriculostomy
INTRODUCTION
There are not many neurosurgeons in Africa; it has the second highest neurosurgical workforce deficit reported globally.[
Hydrocephalus is an enlargement of the ventricles resulting from the inadequate passage or absorption of cerebrospinal fluid (CSF).[
Ventriculoperitoneal shunt (VPS) insertion and endoscopic third ventriculostomy (ETV) are common surgical procedures used to treat pediatric hydrocephalus. In emergency cases, however, external ventricular drainage can be used as a lifesaving procedure while a definitive treatment plan is arranged.[
MATERIALS AND METHODS
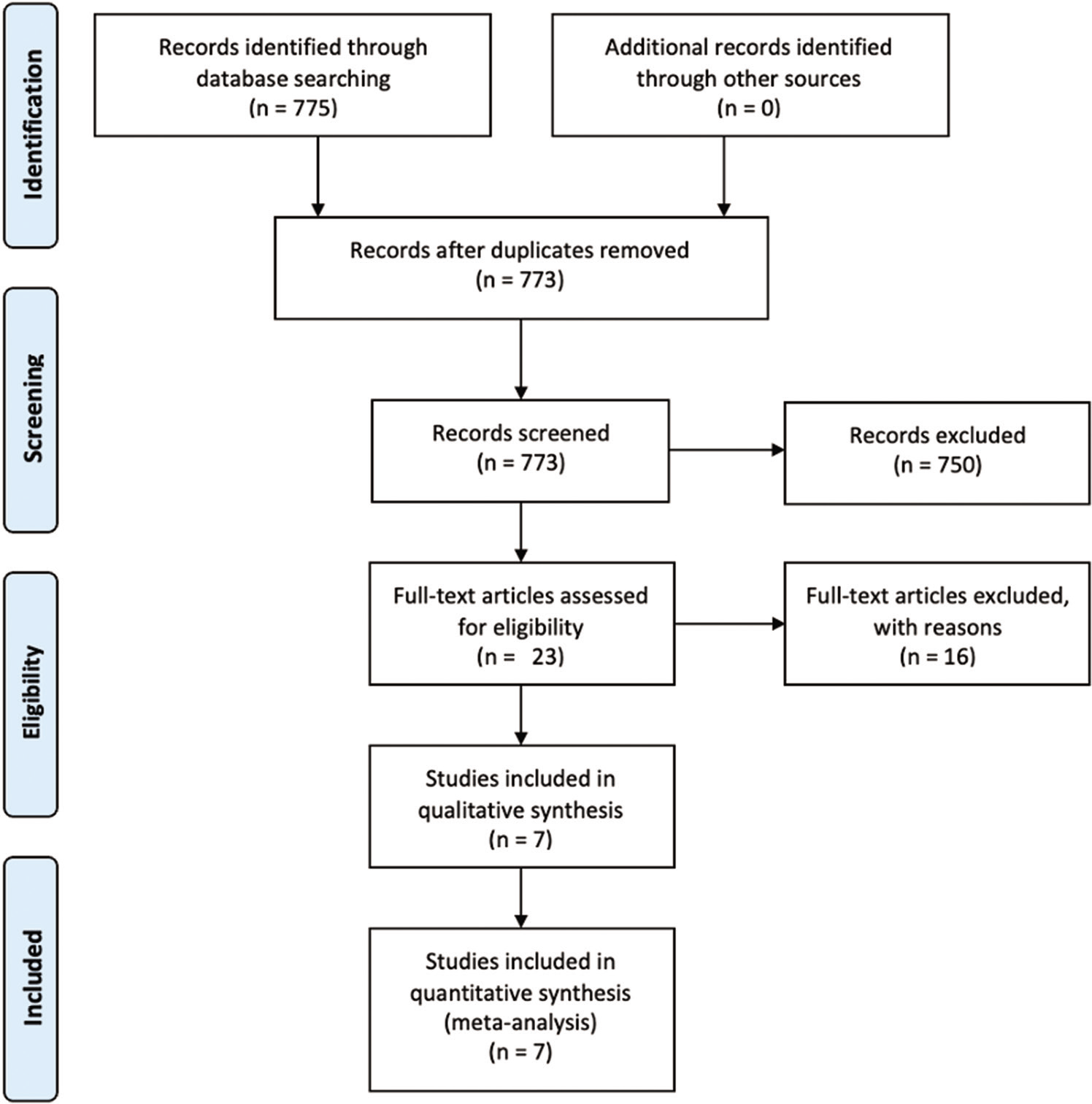
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA guidelines) were used in conducting this study. A guide that included the review question, search strategy, eligibility criteria, and risk of bias assessment was established before the commencement of this review. Papers that compared ETV with VPS in the management of pediatric hydrocephalus in African surgical centers were included in this study. Studies that were not in the English language, from non-African countries and studies that did not compare ETV with VPS systems were excluded from the study. Reviews, meta-analyses, abstracts, conference presentations, commentaries, case reports, and letters to the editors were excluded from the study. Studies that reported data on ETV or VPS alone were excluded from the study. Studies that failed to report disaggregated data on ETV and VPS were also excluded from the study. To identify all eligible articles, a search was conducted from inception to August 2022. PubMed, Google Scholar, and African Journal Online were searched. During the screening process, the references of similar review articles were manually searched for studies that may have been missed by our initial search. The search strategy was jointly devised by the authors and is summarized in
To ensure consistency, two authors screened each article twice. Where conflicts existed, they were resolved by the third author. The search was broad and it aimed to identify all papers with information on ETV and VPS. The titles and abstracts were screened first, followed by a full-text screening. We extracted the following data: the author, publication year, country, study design, study arms, age, gender, cause of the hydrocephalus, period of follow-up, CSF leak, infection, mortality, reoperation, shunt malfunction, failure of ETV, and successful outcomes. For this meta-analysis, a clinically successful outcome was defined as no significant event or complication occurring after surgery and during follow-up (e.g., infection, failure, CSF leak, malfunction, and mortality). Failure was defined as the occurrence of a postoperative significant event (e.g., infection, failure, CSF leak, malfunction, shunt erosion, and mortality). The primary outcome was defined as the success or failure of the procedure. Raw data on clinically successful outcomes for ETV and VPS were pooled together and analyzed with a binary meta-analysis. All studies were first analyzed together, and then, all observational studies (6/7) were analyzed together. Subgroup analysis based on the risk of bias was also carried out. Tests of heterogeneity were also carried out with the Egger’s test and a funnel plot. The meta-analysis feature of IBM SPSS versus 28.0.1 was used. The analysis was carried out with inverse variance, and a random effects meta-analysis was used to account for the heterogeneity of studies. The level of significance was set at 0.05 with a 95% confidence interval.
RESULTS
Seven hundred and fifty papers were excluded after the titles and abstracts were screened, and 16 more studies were excluded after reading and assessing the full texts. Nine studies were excluded because they did not report the outcome of interest, two studies were excluded because they did not report disaggregated data on ETV and VPS, one study was excluded because the study was conducted in a non-African country, while four studies were excluded because the focus of their paper was on ETV alone. Seven articles fully satisfied the eligibility criteria and were used in this review and meta-analysis.[
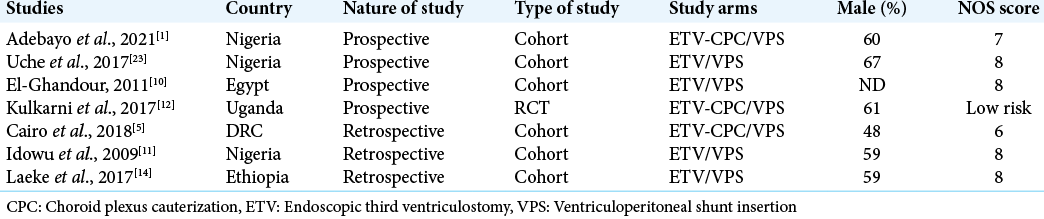
The observational studies used in this review were evaluated with the Newcastle Ottawa Scale evaluation to determine the risk of bias. The studies are shown in
Five studies were of high quality while one study had a high risk. There was one RCT among the selected studies. For that study, we used the Cochrane tool. There was no statistically significant difference between the outcomes of ETV and VPS (OR- 0.27; 95% CI −0.39–0.94) P = 0.42) after analysis of the seven studies. As there were six observational studies and one RCT, we decided to exclude the RCT from the second analysis and see if there would be any substantial difference. After analysis, there was still no statistically significant difference (OR- 0.47; 95% CI −0.25–1.19) P = 0.20); the forest plot can be seen in the appendix as
We went further to do a subgroup analysis by including only high-quality observational studies (scores of 7–9 on the NOS scale – low risk of bias studies), and still, there was still no significant difference (OR−0.47; 95% CI −0.29 −1.24, P = 0.23). The forest plot can be seen in the appendix as
DISCUSSION
Our study included 580 African children who had procedures done in African centers. In this study, we sought to compare the successful outcomes between ETV and VPS insertion in the management of pediatric hydrocephalus. Although this subject has been widely published in the literature, we intended to compare these two from an African perspective while paying attention to the findings and experiences from neurosurgical centers across the continent. Interestingly, we found no statistically significant difference in the outcomes. Studies conducted in some African centers also found no significant difference in outcomes between ETV–CPC and ventriculoperitoneal shunting.[
In our study, the failure rates were consistently lower with ETV than they were with VPS. This finding is consistent with other studies in the published literature.[
The amount of existing research on this subject is exhaustive and many systematic reviews and meta-analyses have provided evidence on this topic. This study, however, is the first to look exclusively at the African literature, to generate evidence that may guide local practices. Regardless, more studies may need to be done on a geographic basis to generate locally relevant guidelines and practices that will improve patient care. Despite the comprehensive nature of this study, we had some limitations. The small sample size and the few African studies covered in this review make generalization difficult. Because we included articles only in the English language and searched three databases, we may have missed potentially relevant papers from nonanglophone countries. The heterogeneity of the studies in terms of how the complications were defined makes it hard to generalize the complications across the board.
CONCLUSION
This study concludes that there is no significant difference between the outcomes of ETV and VP shunt insertion. Considering the findings of this study, it would depend on other factors such as cost, accessibility, the skill, experience, and preference of the operating neurosurgeon when determining a surgical modality for the management of pediatric hydrocephalus. This paper contributes immensely to the African pediatric neurosurgical front and adds more evidence to local practices when managing pediatric hydrocephalus.
Data availability
Data are available on reasonable request.
Ethical approval
Ethical approval was not needed for this paper.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Care for All Foundation Research Grant (CFA 3262-22).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge the Care for All foundation for which D.J won a research grant award (CFA 3262-22).
References
1. Adebayo BO, Kanu OO, Bankole OB, Ojo OA, Adetunmbi B, Morgan E. Early outcome of endoscopic third ventriculostomy with choroid plexus cauterization versus ventriculoperitoneal shunt as primary treatment of hydrocephalus in children with myelomeningocele: A prospective cohort study. Oper Neurosurg (Hagerstown). 2021. 21: 461-6
2. Albright AL. Reflections on developing pediatric neurosurgery in Sub-Saharan Africa. J Neurosurg Pediatr. 2016. 18: 127-38
3. Appelgren T, Zetterstrand S, Elfversson J, Nilsson D. Long-term outcome after treatment of hydrocephalus in children. Pediatr Neurosurg. 2010. 46: 221-6
4. Bryant MJ, McEniery J, Walker DG, Campbell R, Lister B, Sargent P. Preliminary study of shunt related death in paediatric patients. J Clin Neurosci. 2004. 11: 614-5
5. Cairo SB, Agyei J, Nyavandu K, Rothstein DH, Kalisya LM. Neurosurgical management of hydrocephalus by a general surgeon in an extremely low resource setting: Initial experience in North Kivu province of eastern democratic republic of Congo. Pediatr Surg Int. 2018. 34: 467-73
6. Dandy WE, Blackfan KD. An experimental and clinical study of internal hydrocephalus. JAMA. 1913. 61: 2216-7
7. Dewan MC, Naftel RP. The global rise of endoscopic third ventriculostomy with choroid plexus cauterization in pediatric hydrocephalus. Pediatr Neurosurg. 2017. 52: 401-8
8. Dewan MC, Rattani A, Fieggen G, Arraez MA, Servadei F, Boop FA. Global neurosurgery: The current capacity and deficit in the provision of essential neurosurgical care. Executive summary of the global neurosurgery initiative at the program in global surgery and social change. J Neurosurg. 2018. 130: 1-10
9. El Khamlichi A. African neurosurgery: Current situation, priorities, and needs. Neurosurgery. 2001. 48: 1344-7
10. El-Ghandour NM. Endoscopic third ventriculostomy versus ventriculoperitoneal shunt in the treatment of obstructive hydrocephalus due to posterior fossa tumors in children. Childs Nerv Syst. 2011. 27: 117-26
11. Idowu OE, Falope LO, Idowu AT. Outcome of endoscopic third ventriculostomy and chhabra shunt system in noncommunicating non-tumor childhood hydrocephalus. J Pediatr Neurosci. 2009. 4: 66-9
12. Kulkarni AV, Schiff SJ, Mbabazi-Kabachelor E, Mugamba J, Ssenyonga P, Donnelly R. Endoscopic treatment versus shunting for infant hydrocephalus in Uganda. N Engl J Med. 2017. 377: 2456-64
13. Kulkarni AV, Warf BC, Drake JM, Mallucci CL, Sgouros S, Constantini S. Surgery for hydrocephalus in Sub-Saharan Africa versus developed nations: A risk-adjusted comparison of outcome. Childs Nerv Syst. 2010. 26: 1711-7
14. Laeke T, Tirsit A, Biluts H, Murali D, Wester K. Pediatric hydrocephalus in Ethiopia: Treatment failures and infections: A hospital-based, retrospective study. World Neurosurg. 2017. 100: 30-7
15. Lima BO, Pratesi R. Endoscopic third ventriculostomy has no higher costs than ventriculoperitoneal shunt. Arq Neuropsiquiatr. 2014. 72: 524-7
16. Morgan E, Nwatuzor C. Starting a neurosurgical service in a Southern Nigeria rural community. Prospect, challenges, and future-the Irrua experience. Egypt J Neurosurg. 2020. 35: 6
17. Rekate HL. The definition and classification of hydrocephalus: A personal recommendation to stimulate debate. Cerebrospinal Fluid Res. 2008. 5: 2
18. Robertson FC, Gnanakumar S, Karekezi C, Vaughan K, Garcia RM, Bourquin BA. The world federation of neurosurgical societies young neurosurgeons survey (Part II): Barriers to professional development and service delivery in neurosurgery. World Neurosurg X. 2020. 8: 100084
19. Schrander-Stumpel C, Fryns JP. Congenital hydrocephalus: Nosology and guidelines for clinical approach and genetic counselling. Eur J Pediatr. 1998. 157: 355-62
20. Tuli S, Alshail E, Drake J. Third ventriculostomy versus cerebrospinal fluid shunt as a first procedure in pediatric hydrocephalus. Pediatr Neurosurg. 1999. 30: 11-5
21. Tuli S, Tuli J, Drake J, Spears J. Predictors of death in pediatric patients requiring cerebrospinal fluid shunts. J Neurosurg. 2004. 100: 442-6
22. Tully HM, Dobyns WB. Infantile hydrocephalus: A review of epidemiology, classification and causes. Eur J Med Genet. 2014. 57: 359-68
23. Uche EO, Okorie C, Iloabachie I, Amuta DS, Uche NJ. Endoscopic third ventriculostomy (ETV) and ventriculoperitoneal shunt (VPS) in non-communicating hydrocephalus (NCH): Comparison of outcome profiles in Nigerian children. Childs Nerv Syst. 2018. 34: 1683-9
24. Upadhyayula PS, Yue JK, Yang J, Birk HS, Ciacci JD. The current state of rural neurosurgical practice: An international perspective. J Neurosci Rural Pract. 2018. 9: 123-31
25. Warf BC. Comparison of endoscopic third ventriculostomy alone and combined with choroid plexus cauterization in infants younger than 1 year of age: A prospective study in 550 African children. J Neurosurg. 2005. 103: 475-81
26. Warf BC. The impact of combined endoscopic third ventriculostomy and choroid plexus cauterization on the management of pediatric hydrocephalus in developing countries. World Neurosurg. 2013. 79: S23.e13-5
27. Wright Z, Larrew TW, Eskandari R. Pediatric hydrocephalus: Current state of diagnosis and treatment. Pediatr Rev. 2016. 37: 478-90