- Department of Neurosurgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India,
- Department of Orthopedic Surgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India,
- College of Nursing, All India Institute of Medical Sciences, Deoghar, Jharkhand, India,
- Department of Neuroanesthesia, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India,
- Department of Neurointervention, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
Correspondence Address:
Jitender Chaturvedi, Department of Neurosurgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
DOI:10.25259/SNI_261_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jitender Chaturvedi1, P. Venkata Sudhakar2, Mohit Gupta1, Nishant Goyal1, Shiv Kumar Mudgal3, Priyanka Gupta4, Sandeep Burathoki5. Endovascular management of iatrogenic vertebro-vertebral fistula: Black Swan event in C2 pedicle screw. 06-May-2022;13:189
How to cite this URL: Jitender Chaturvedi1, P. Venkata Sudhakar2, Mohit Gupta1, Nishant Goyal1, Shiv Kumar Mudgal3, Priyanka Gupta4, Sandeep Burathoki5. Endovascular management of iatrogenic vertebro-vertebral fistula: Black Swan event in C2 pedicle screw. 06-May-2022;13:189. Available from: https://surgicalneurologyint.com/surgicalint-articles/11583/
Abstract
Background: Vertebro-vertebral fistulas (VVF) are rare. Anatomically, they consist of an arteriovenous fistula, a direct pathological communication between vertebral veins (including the epidural vertebral venous plexus) and extradural vertebral artery. The various etiologies include trauma, iatrogenic, or spontaneous (e.g., NF-1 or Ehlers Danlos Syndrome). The clinical presentation may include acute/delayed onset of radiculopathy and/or myelopathy. They may further be characterized by the delayed onset hearing loss to tinnitus and/or the sensation of water in the ear.
Case Description: We report successful endovascular management for iatrogenic VVF in a 37-year-old female who was diagnosed with an odontoid fracture (Anderson type IIC). She underwent a posterior C1 lateral masses to C2 pedicle/laminar screw fixation. An intraoperative vertebro-vertebral fistulas (VVF) was recognized during the procedure and it was managed successfully with percutaneous transarterial endovascular coiling.
Conclusion: Iatrogenic VVF should immediately be suspected when the implant trajectory goes slightly off track during a C1-2 fixation. Immediate postoperative DSA and MRI are advisable, irrespective of whether the patient is symptomatic. These lesions are best managed with endovascular coiling with or without detachable balloons.
Keywords: Endovascular coiling, Iatrogenic, Odontoid fracture, Vertebro-vertebral fistula, Black Swan
INTRODUCTION
Vertebro-vertebral arteriovenous fistulas are rare. They consist of a high flow shunt between the extracranial vertebral artery, its muscular or radicular branches, and the adjacent vertebral venous plexuses. The etiology of these vascular lesions can be traumatic, iatrogenic, or spontaneous.[
CASE REPORT
Clinical presentation with quadriparesis
A 37-year-old female presented with a progressive quadriparesis and hypoxia following a road traffic accident. Following emergent intubation, she was found to have 0/5 motor function on the right and 2/5 function on the left in the C5-T1 distributions and 2/5 function in the right lower extremity, i.e., L2-S1 myotomes.
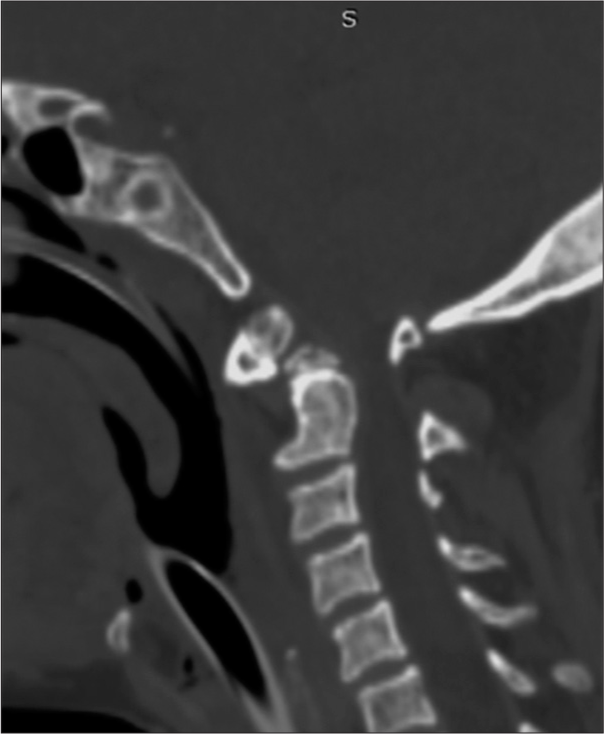
Computed tomography (CT)/MR presentation of odontoid Type II fracture
The CT studies showed an anteriorly displaced odontoid fracture through the base of dens (Anderson D’Alonzo type IIC) on CT scan [
Surgery
She underwent excision of the C1 posterior arch with the placement of bilateral C1 lateral mass screws and placement of bilateral C2 pedicle screws. However, after satisfactorily placing the right-sided C2 pedicle screw into position, the left-sided pedicle resulted in unexpected brisk nonpulsatile and dark venous bleeding from the entry point; notably, it stopped immediately after the application of wax. As a rescue procedure, the final construct included bilateral C1 lateral mass screws, a right C2 pedicle screw supplemented with a right C2 laminar screws, followed by rod fixation.
Postoperative course
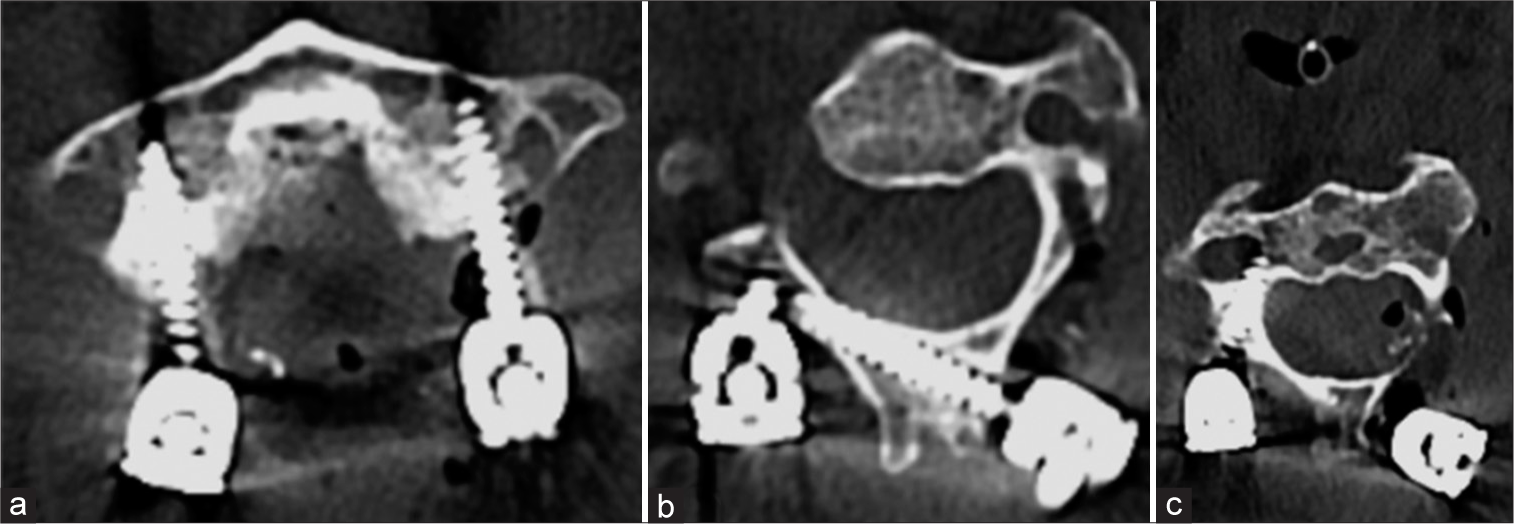
Immediate postoperatively, the CT CV junction [
Figure 2:
(a) Postoperative CT scan axial cut at the level of C1 showing bilateral lateral mass screws and (b) axial CT cuts at the level of C2 showing right laminar screw. Tract made for pedicle screw insertion on the left side is also appreciated (responsible for fistula formation). (c) Right pedicle screw at C2.
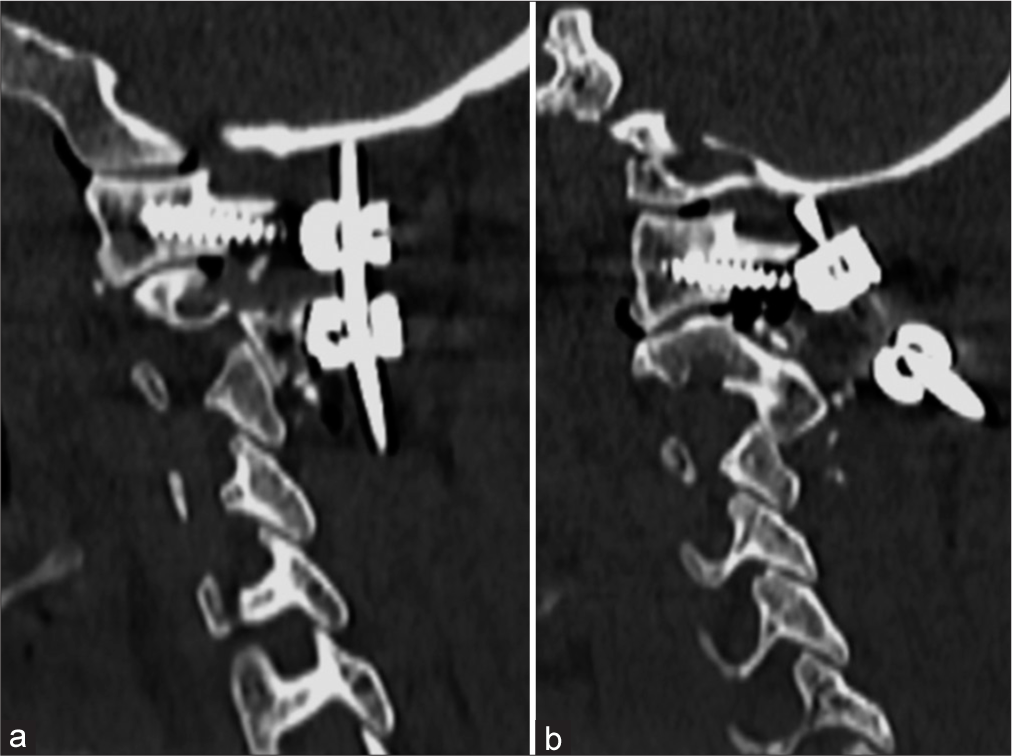
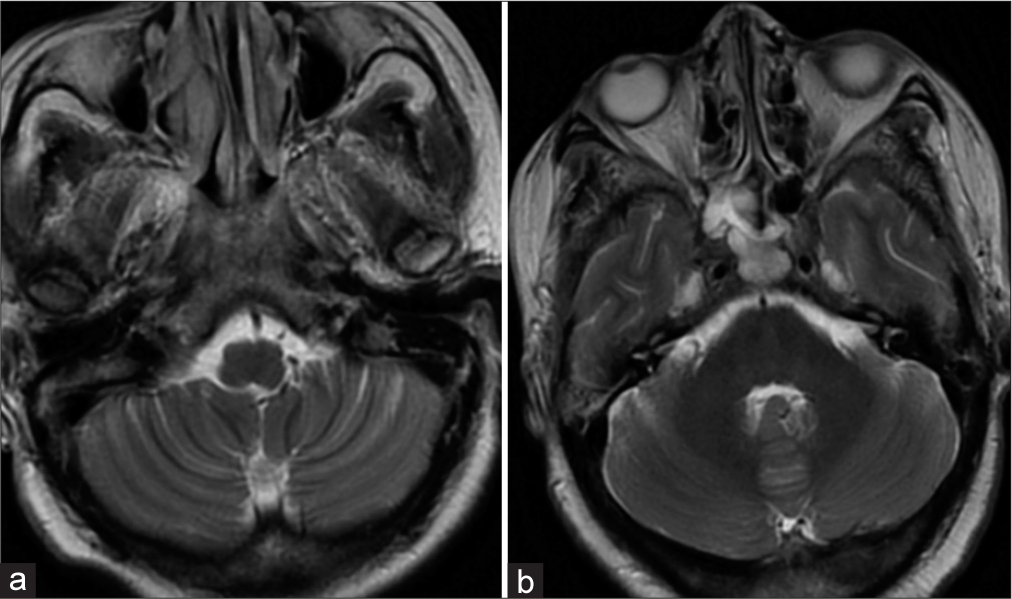
Figure 5:
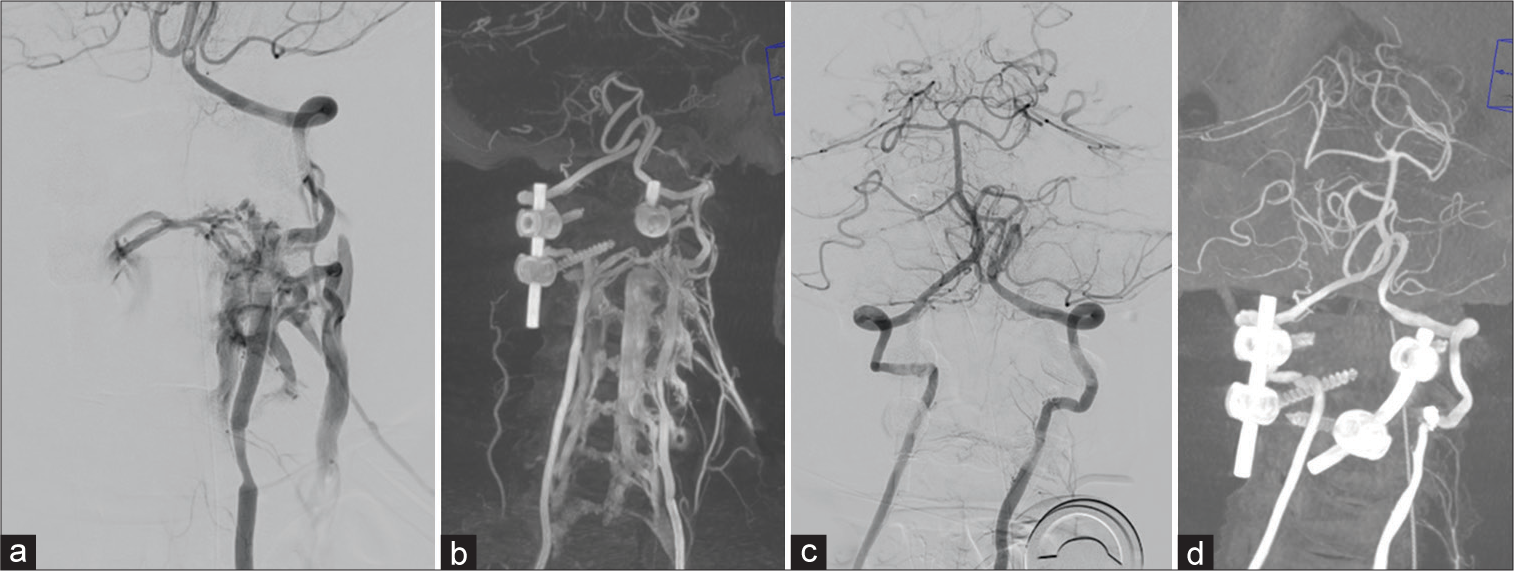
Left vertebral artery injection (a) and coronal reformatted image (b) showed vertebra-vertebral fistula at V2 segment with a filling of vertebral venous plexus (arrow) and intervertebral venous plexus (arrowhead). Endovascular treatment was performed using standard tri-coaxial technique, 6 F guide catheter (Envoy, Codman, US) was placed at proximal left vertebral artery. Then, microcatheter (Headway 17, Microvention, US) over microwire (Traxcess 14, Microvention, US) was selectively placed at fistulous junction. Three electro-detachable coils (Cosmos 4 mm × 12 cm, helical 3 mm ×6 cm, helical 2.5 mm × 6 cm, Microvention, US) were deployed at fistulous junction under balloon (Scepter C 4 mm × 15 mm, Microvention, US) protection of the left vertebral artery. Final angiogram showed complete occlusion of vertebravertebral fistula. Post coiling left vertebral artery injection (c) and reformatted image (d) showed complete closure of the fistula.
DISCUSSION
Vertebro-vertebral fistula (VVF) is a pathological communication between vertebral artery or its muscular/ radicular branches and venous plexus.[
CONCLUSION
An iatrogenic VVF should be immediately suspected if screw placement goes off track during a C1-2 fixation. In these cases, an immediate postoperative CT, MRI, and DSA should be performed to rule out the presence of a VVF that may then be emergently coiled by a neurointerventionist.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aljobeh A, Sorenson TJ, Bortolotti C, Cloft H, Lanzino G. Vertebral arteriovenous fistula: A review article. World Neurosurg. 2019. 122: e1388-97
2. Briganti F, Tedeschi E, Leone G, Marseglia M, Cicala D, Giamundo M. Endovascular treatment of vertebrovertebral arteriovenous fistula. A report of three cases and literature review. Neuroradiol J. 2013. 26: 339-46
3. Duncan IC, Fourie PA. Percutaneous management of concomitant post-traumatic high vertebrovertebral and caroticojugular fistulas using balloons, coils, and a covered stent. J Endovasc Ther. 2003. 10: 882-6
4. Geng J, Hu P, Ma Y, Zhang P, Zhang H. Endovascular treatment of V3 segment vertebro-vertebral arteriovenous fistula with Willis covered stent: Case report and literature review. Interv Neuroradiol. 2019. 25: 97-101
5. He H, Li Q, Du M, Chen K, Li X, Li J. Endovascular and surgical approaches of iatrogenic vertebrovertebral arteriovenous fistula. J Vasc Surg Cases Innov Tech. 2021. 7: 206-10
6. Honarmand AR, Ansari SA, Alden TD, Soltanolkotabi M, Schoeneman SE, Hurley MC. Endovascular management of pediatric high-flow vertebro-vertebral fistula with reversed basilar artery flow. A case report and review of the literature. Interv Neuroradiol. 2013. 19: 215-21
7. Li F, Song X, Liu C, Liu B, Zheng Y. Endovascular stent-graft treatment for a traumatic vertebrovertebral arteriovenous fistula with pseudoaneurysm. Ann Vasc Surg. 2014. 28: 489.e11-4
8. Madoz A, Desal H, Auffray-Calvier E, Isnard J, Liberge R, Taverneau C. Diagnostic et traitement des fistules vertébrovertébrales. Revue de la littérature: À propos de 8 observations [Vertebrovertebral arteriovenous fistula diagnosis and treatment: Report of 8 cases and review of the literature]. J Neuroradiol. 2006. 33: 319-27
9. Ono I, Satow T, Ito Y, Hamano E, Matsubara H, Kataoka H. Case of iatrogenic vertebro-vertebral arteriovenous fistula treated by combination of double-catheter and balloon anchoring techniques. World Neurosurg. 2019. 128: 98-101
10. Robinson PN, Jewkes DA, Kendall B. Vertebrovertebral arteriovenous fistula. A complication of internal jugular catheterisation. Anaesthesia. 1984. 39: 46-7