- Department of Neurosurgery, Imamura General Hospital, Kagoshima, Japan.
- Department of Neurosurgery, National Hospital Organization Kagoshima Medical Center, Kagoshima, Japan.
- Department of Neurosurgery, Sakaki Neurosurgical Clinic, Kagoshima, Japan.
- Department of Neurosurgery, Kagoshima University, Kagoshima, Japan.
Correspondence Address:
Kazunori Arita, Department of Neurosurgery, Kagoshima University, Kagoshima, Japan.
DOI:10.25259/SNI_219_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Natsuko Tanoue1, Ayumi Taniguchi1, Fumikatsu Kubo2, Nozomi Shibuya1, Seigo Sakaki3, Ryosuke Hanaya4, Kazunori Arita4. Endovascular treatment of unruptured aneurysm arising from duplicate origin of the middle cerebral artery – A case report and literature review. 07-Jun-2024;15:194
How to cite this URL: Natsuko Tanoue1, Ayumi Taniguchi1, Fumikatsu Kubo2, Nozomi Shibuya1, Seigo Sakaki3, Ryosuke Hanaya4, Kazunori Arita4. Endovascular treatment of unruptured aneurysm arising from duplicate origin of the middle cerebral artery – A case report and literature review. 07-Jun-2024;15:194. Available from: https://surgicalneurologyint.com/surgicalint-articles/12927/
Abstract
Background: Duplicate origin of the middle cerebral artery (MCA) is a rare variation of MCA, often mislabeled as the fenestration of the M1 segment of MCA.
Case Description: The authors treated an unruptured aneurysm, 8 mm in diameter, associated with a duplicate origin of MCA in a 42-year-old woman who underwent magnetic resonance imaging for transient vertigo. Clipping surgery was inapplicable due to the lack of space to insert clip blades between the neck and two origins of MCA. Under stent-assisted maneuver, the aneurysm sac was successfully obliterated using three coils, resulting in Raymond-Roy class 1 occlusion status. Digital subtraction angiography performed 3 months after the embolization showed complete obliteration of the aneurysm. So far, only 11 patients with aneurysms associated with duplicate origin of MCA have been reported. We performed a literature review of this very rare combination. The size of aneurysms ranged from 2 to 8 mm, with a mean of 5.2 mm. The neck of the aneurysm is mainly located at the corner between the inferior limb and the internal carotid artery. Ours is the youngest and has the largest aneurysm.
Conclusion: Aneurysm can arise from duplicate origin of MCA, for which stent-assisted coiling may be an appropriate treatment modality.
Keywords: Aneurysm, Coil embolization, Duplicate origin of middle cerebral artery, Endovascular treatment, Stent-assisted coiling
INTRODUCTION
Anatomical variations of proximal middle cerebral artery (MCA) include duplicate MCA, accessory MCA, early bifurcation of MCA, fenestrated MCA, and duplicate origin of MCA (DOMA).[
The authors hereby report a rare case of aneurysm arising from the proximal portion of DOMA, treated by endovascular coil embolization. A literature review of this rare combination is also performed.
CASE REPORT
An otherwise healthy 42-year-old woman suffering transient vertigo underwent magnetic resonance imaging (MRI), which did not show any causative condition for the symptom, whereas MRA found an aneurysm, 8 mm in the largest diameter, at the origin of the left MCA [
Figure 1:
Imaging studies before treatment. (a) Anteroposterior view of MRA, (b) anteroposterior view of 3DR-DSA, (c) left-right view of 3DR-DSA, and (d) posteroanterior view of 3DR-DSA. MRA suggested an aneurysm (square in a) at the origin of the left MCA. The aneurysm with irregular configuration protruded anteriorly and posteriorly through the ring composed of two limbs of DOMA on 3DRDSA images (b-d). Square: Supposed aneurysm on MRA: Magnetic resonance angiography, ICA: internal carotid artery, ATA: Anterior temporal artery, Ach: Anterior choroidal artery, LSA: lenticulostriate artery, SL: superior limb of DOMA, IL: inferior limb of DOMA, Pcom: posterior communicating artery, Arrowhead: fusing point of two limbs of DOMA, Yellow arrow: Anterior projection of aneurysm, Blue arrow: posterior projection of aneurysm, 3DR-DSA: Three-dimensional reconstruction image of digital subtraction angiography, MCA: Middle cerebral artery, DOMA: Duplicate origin of middle cerebral artery. A1 and A2: A1 and A2 portion of anterior cerebral artery, M1 and M2: M1 and M2 portion of middle cerebral artery.
Before the treatment, the patient was given 2 weeks-long dual antiplatelet treatment with prasugrel hydrochloride 3.75 mg/day and acetylsalicylic acid 100 mg/day.
Under general anesthesia, a 9 Fr sheath was inserted into the right femoral artery. Through the sheath, the tip of an 8 Fr guiding catheter was put into the left cervical portion of the ICA, and then, a 6 Fr intermediate catheter was introduced into the cavernous portion of the ICA, through which microcatheters were advanced distally. Microcatheter-1 for stenting was advanced to M1-portion of the MCA through the superior limb. Through microcatheter-2, which was put into the aneurysmal sac, a Target 360 SOFT ® 5 mm × 15 cm coil (Stryker, USA) for framing was advanced into the sac. After the second loop of the framing coil was deployed, the tip of the coil was found inadvertently advanced into the inferior limb and then into the superior limb through the distal fusion point of the ring [
Figure 2:
DSA of the left internal carotid artery during coil embolization. (a) Anteroposterior view of road mapping image during embolization, (b) right-left view of road mapping image during embolization, (c) anteroposterior view of DSA after the embolization, and (d) right-left view of DSA after the embolization. The tip of the coil inadvertently migrated into the upper limb through the lower limb of DOMA at the initial stage of framing (a and b). Complete obliteration of the aneurysm was achieved (c and d). Asterisk: Aneurysmal sac. ICA: Internal carotid artery, SL: Superior limb of DOMA, IL: Inferior limb of DOMA, ATA: Anterior temporal artery, Yellow arrow: Anterior projection of aneurysm, Blue arrow: Posterior projection of aneurysm, DOMA: Duplicate origin of middle cerebral artery, DSA: Digital subtraction angiography. A2: A2 portion of anterior cerebral artery, M2: M2 portion of middle cerebral artery.
Diffusion-weighted MRI 1 day after the procedure revealed a scattering of asymptomatic small ischemic lesions in the cortical area irrigated by the left MCA. She was discharged 8 days after the procedure without sequela.
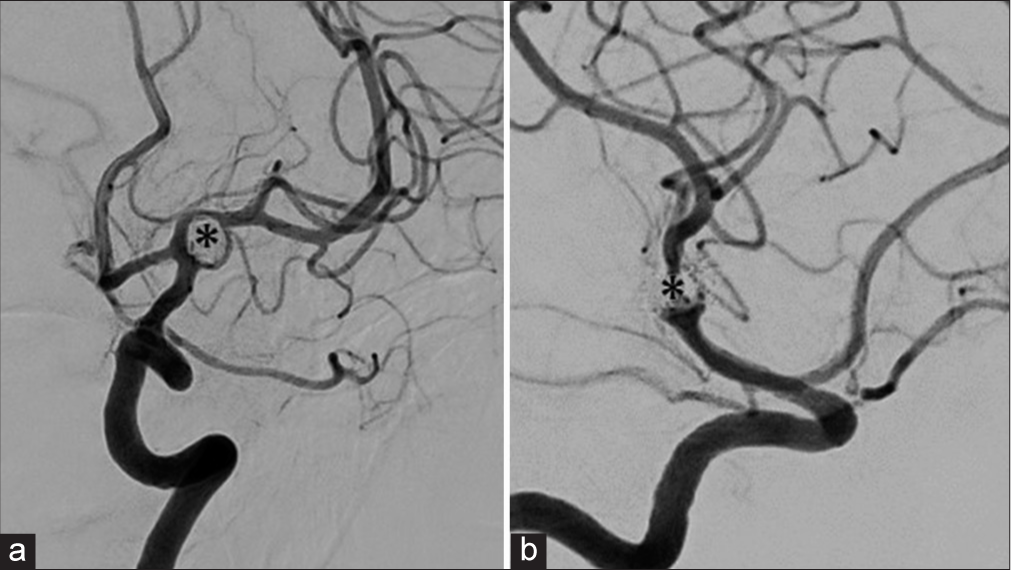
DSA performed 3 months after the embolization showed that the aneurysm remained completely occluded [
Figure 3:
DSA of the left internal carotid artery performed 3 months after the coil embolization. (a) Anteroposterior view, and (b) right-left view. The aneurysmal sac was completely obliterated, demonstrating Raymond-roy occlusion class I. Asterisk: Aneurysmal sac, DSA: Digital subtraction angiography.
LITERATURE REVIEW
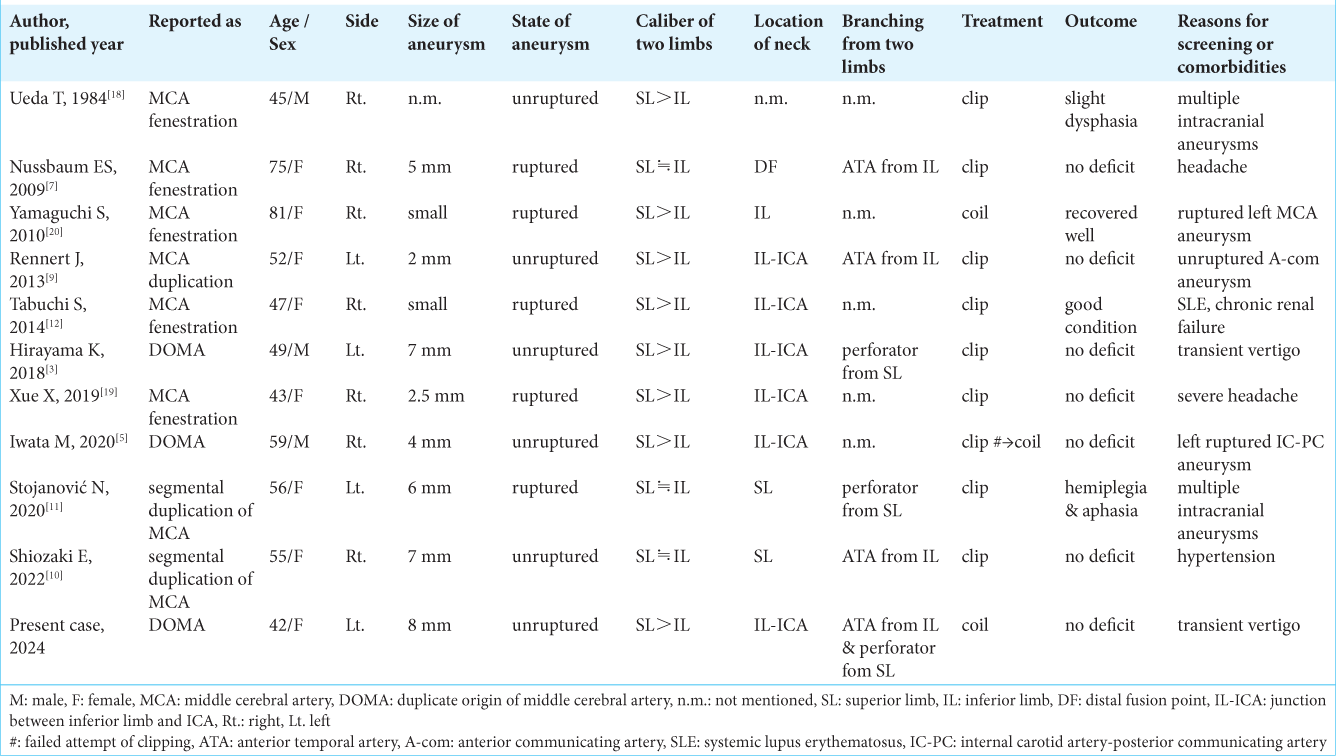
So far as we know, there are 11 reported patients, including ours, eight women and three men, with an aneurysm arising from DOMA [
For the treatment, clipping was performed in eight, coiling was performed in two, and clipping was initially attempted, but eventually, coiling was performed in another patient. Except for two patients with complications after clipping, one with slight dysphasia and another with hemiplegia and aphasia, outcomes of the treatment were generally favorable.
DISCUSSION
In general, anatomical variations of the MCA are caused by a failure in the formation of a single MCA trunk through the coalescing primitive plexiform arterial network, which typically appears during the 34–36 days of the embryonic stage.[
In 2020, Hou et al. found 67 patients with aneurysms reported to be associated with one of the four types of MCA anomalies, including 20 aneurysms associated with accessory MCA, 34 with duplicated MCA, and 12 with MCA fenestration.[
Thus, this is a rare case of an aneurysm arising from DOMA. The aneurysm was the largest, 8 mm, among ever-reported patients with such a combination. The size, patient’s age, and irregular shape of the two domes urged us to treat this unruptured aneurysm. The authors chose the endovascular coiling technique due to the lack of space between the aneurysm neck and two limbs. With the aid of a protective stent of the parent arteries, complete obliteration of the aneurysm was accomplished. During the attempt of initial framing, the tip of the coil was found to be in the superior limb. The happening meant the tip inadvertently migrated into the inferior limb and went into the superior limb through the distal fusion point of two limbs, verifying the existence of the distal communication of the two limbs.
Our extensive review found 11 reported cases of DOMA-associated aneurysms, including ours.[
CONCLUSION
The authors presented a rare case of an aneurysm associated with DOMA, successfully treated with coil embolization. This report will raise awareness of DOMA, preventing it from being mislabeled as other types of anatomical MCA variations. In the future, larger case series will enhance our understanding of the true nature of this combination and inform appropriate management strategies.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
The authors would like to thank Haibunsha Kagoshima for performing a critical review of this manuscript and English language editing.
References
1. Fujimoto K, Hashimoto H, Uchiyama Y, Maekawa H, Shida Y, Nakagawa I. Duplicated middle cerebral artery aneurysms treated by coil embolization; a report of two cases and literature review. J Stroke Cerebrovasc Dis. 2021. 30: 105773
2. Gailloud P, Albayram S, Fasel JH, Beauchamp NJ, Murphy KJ. Angiographic and embryologic considerations in five cases of middle cerebral artery fenestration. AJNR Am J Neuroradiol. 2002. 23: 585-7
3. Hirayama K, Nakamura H, Yoshimura S, Ozono K, Fukuda Y, Hiu T. Unruptured aneurysm arising from the proximal end of the duplicate origin of the middle cerebral artery. No Shinkei Geka. 2018. 46: 901-9
4. Hou K, Xu K, Liu H, Li G, Yu J. The clinical characteristics and treatment considerations for intracranial aneurysms associated with middle cerebral artery anomalies: A systematic review. Front Neurol. 2020. 11: 564797
5. Iwata M, Kawaguchi S, Manaka H. A case of unruptured cerebral aneurysm arising from duplicate origin of the middle cerebral artery. No Shinkei Geka. 2020. 48: 515-20
6. Komiyama M, Nakajima H, Nishikawa M, Yasui T. Middle cerebral artery variations: Duplicated and accessory arteries. AJNR Am J Neuroradiol. 1998. 19: 45-9
7. Nussbaum ES, Defillo A, Janjua TM, Nussbaum LA. Fenestration of the middle cerebral artery with an associated ruptured aneurysm. J Clin Neurosci. 2009. 16: 845-7
8. Padget DH. The development of the cranial arteries in the human embryo. Contr Embryol Carneg Instn. 1948. 32: 205-61
9. Rennert J, Ullrich WO, Schuierer G. A rare case of supraclinoid internal carotid artery (ICA) fenestration in combination with duplication of the middle cerebral artery (MCA) originating from the ICA fenestration and an associated aneurysm. Clin Neuroradiol. 2013. 23: 133-6
10. Shiozaki E, Kawahara I, Uchida D, Morofuji Y, Ono T, Haraguchi W. Unruptured cerebral aneurysms with the segmental duplicated middle cerebral artery formed a fenestrated structure at origin. Surg Neurol Int. 2022. 13: 33
11. Stojanović NN, Kostić A, Mitić R, Berilažić L. Correlation between multiple cerebral aneurysms and a rare type of segmental duplication of the middle cerebral artery. BMC Neurol. 2020. 20: 3
12. Tabuchi S, Yoshioka H. Ruptured aneurysm at the fenestration of the middle cerebral artery detected by magnetic resonance angiography in a patient with systemic lupus erythematosus and renal failure: A case report. J Med Case Rep. 2014. 8: 30
13. Teal JS, Rumbaugh CL, Bergeron RT, Segall HD. Anomalies of the middle cerebral artery: Accessory artery, duplication, and early bifurcation. Am J Roentgenol. 1973. 118: 567-75
14. Uchino A, editors. Variation of proximal middle cerebral artery (MCA). Atlas of the supraaortic craniocervical arterial variations: MR and CT angiography. Singapore: Springer-Verlag; 2022. p. 99-107
15. Uchino A, Saito N, Okada Y, Nakajima R. Duplicate origin and fenestration of the middle cerebral artery on MR angiography. Surg Radiol Anat. 2012. 34: 401-4
16. Uchino A, Takase Y, Nomiyama K, Egashira R, Kudo S. Fenestration of the middle cerebral artery detected by MR angiography. Magn Reson Med Sci. 2006. 5: 51-5
17. Uchiyama N. Anomalies of the middle cerebral artery. Neurol Med Chir (Tokyo). 2017. 57: 261-6
18. Ueda T, Goya T, Kinoshita K, Wakuta Y, Mihara K. Multiple anomalies of cerebral vessels. A case of multiple aneurysms associated with fenestration of the middle cerebral artery and persistent primitive trigeminal artery. No Shinkei Geka. 1984. 12: 531-6
19. Xue X, Li Y, Yin Y, Yuan X, Xiao H, Wei L. Aneurysms arising from the fenestrated middle cerebral artery. J Craniofac Surg. 2019. 30: e485-7
20. Yamaguchi S, Ito O, Suzuki S. Coil embolization of a ruptured aneurysm arising from a middle cerebral artery fenestration--case report. Neurol Med Chir (Tokyo). 2010. 50: 213-6