- Department of Surgery, College of Medicine, University of Baghdad, Baghdad, Iraq
- Department of Neurosurgery, Teaching Hospital, Baghdad, Iraq.
Correspondence Address:
Najah K. Mohammad, Department of Surgery, College of Medicine, University of Baghdad, Baghdad, Iraq.
DOI:10.25259/SNI_120_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Najah K. Mohammad1, Ibrahim Ali Rajab1, Mohammed T. Mutar1, Mustafa Ismail2. Enhancing neuro-ophthalmic surgical education: The role of neuroanatomy and 3D digital technologies – An overview. 29-Mar-2024;15:106
How to cite this URL: Najah K. Mohammad1, Ibrahim Ali Rajab1, Mohammed T. Mutar1, Mustafa Ismail2. Enhancing neuro-ophthalmic surgical education: The role of neuroanatomy and 3D digital technologies – An overview. 29-Mar-2024;15:106. Available from: https://surgicalneurologyint.com/surgicalint-articles/12833/
Abstract
Background: Neuro-ophthalmology, bridging neurology and ophthalmology, highlights the nervous system’s crucial role in vision, encompassing afferent and efferent pathways. The evolution of this field has emphasized the importance of neuroanatomy for precise surgical interventions, presenting educational challenges in blending complex anatomical knowledge with surgical skills. This review examines the interplay between neuroanatomy and surgical practices in neuro-ophthalmology, aiming to identify educational gaps and suggest improvements.
Methods: A literature search across databases such as PubMed, Scopus, and Web of Science was conducted, focusing on the implications of neuroanatomy in neuro-ophthalmic surgery education and practice. The review synthesizes insights from both recent and foundational studies to highlight current understandings and future research directions, particularly in educational approaches.
Results: Findings indicate that 3D digital modeling and virtual reality have significantly enhanced neuroophthalmic surgical education by providing immersive and engaging learning experiences. For instance, detailed 3D brain atlases offer comprehensive resources for understanding the central nervous system’s normal and pathological states. Although studies show that 3D and traditional 2D methods achieve similar post-test results, 3D methods notably improve engagement and motivation, suggesting a shift toward more interactive learning environments.
Conclusion: Integrating both traditional and innovative educational tools is crucial for the progression of neuro-ophthalmic surgical training. This balance helps overcome educational hurdles and better prepare future surgeons. Continuous research and collaboration are essential to refine educational strategies, ultimately aiming to enhance patient care in neuro-ophthalmology.
Keywords: 3D digital modeling, Neuroanatomy, Neuro-ophthalmology, Surgical education, Virtual reality
INTRODUCTION
Neuro-ophthalmology serves as the crossroads between neurology and ophthalmology. It deals with the nervous system’s role in vision, in particular, the afferent and efferent visual pathways that extend from the retina to the visual cortex.[
MATERIALS AND METHODS
The methodology for the narrative review involves a literature search in databases such as PubMed, Scopus, and Web of Science, focusing on keywords related to neuroanatomy, neuro-ophthalmology, and surgical education. The review prioritizes recent articles complemented by foundational studies for context. Inclusion criteria target studies on neuroanatomy’s educational and practical roles in neuroophthalmic surgery, with a qualitative analysis of selected articles to assess their contributions to the field. This approach aims to synthesize current insights and identify areas for future research in neuro-ophthalmic surgical education.
RESULTS
The results section of our narrative review highlights the transformative role of 3D digital modeling and virtual reality (VR) technologies in enhancing the educational landscape. The pioneering work by Nowinski and Thaung[
3D virtual resources of educational anatomy were also sought, but this time within the teaching environment. In fact, Stepan et al.[
DISCUSSION
Integration of advanced technologies in surgical education
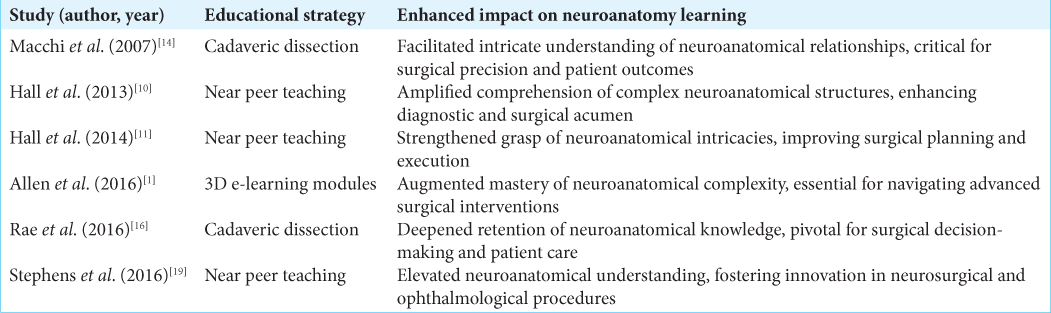
Multiple studies reported the effect of utilizing computer-based tools in neuroanatomy teaching.[
It introduces techniques that enrich training landscapes for neuro-ophthalmic and neurosurgeons, such as VR and 3D modeling. This technology enhances understanding of neuro-anatomical structures and neurosurgical methods through immersive and interactive learning experiences. Estevez et al.[
These tools have roles beyond undergraduate medical education, extending into specialized fields such as neurosurgery to enhance clinical practice readiness. VR technology holds promise for medical education and practice but requires further evaluation to understand its full capabilities and limitations.[
Cadaveric dissection’s enduring value
It has rightly been said and discussed quite clearly by Macchi et al.[
The role of peer teaching
Effective near-peer teaching strategies, illustrated in the study by Hall et al.[
Challenges and limitations
While the integration of VR, 3D modeling, and other innovative teaching methods hold promise, several challenges persist. The high cost of technology, the steep learning curve associated with new software, and the need for continual updates to reflect the latest surgical and anatomical knowledge are significant barriers. Furthermore, the tactile sensation and the nuanced feel of real tissue manipulation during surgery are not fully replicable in a virtual environment, indicating a gap that technology has yet to bridge fully.
Future directions
Looking forward, the incorporation of artificial intelligence and machine learning into educational tools could personalize learning experiences, adapt to individual student needs, and simulate a wider range of surgical scenarios. The development of more sophisticated haptic feedback systems could also enhance the realism of VR simulations, making them more valuable for surgical training.
Over time, neuro-ophthalmology has redefined surgical education, hence an evolution with innovation coupled with tradition. As described very convincingly by Estevez et al.[
CONCLUSION
The evolution of neuro-ophthalmic surgical education intertwines traditional practices with modern innovations, balancing the enduring value of hands-on techniques with the potential of new technologies. This synergy is essential for advancing surgical training, overcoming current challenges, and preparing future neuro-ophthalmic surgeons. Continuous research, technological improvements, and collaborative efforts are crucial for enhancing educational strategies and ultimately bettering patient care in the specialty.
Ethical approval
The Institutional Review Board approval is not required
Declaration of patient consent
Patient’s consent are not required as there are no patients in this study
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Allen LK, Eagleson R, de Ribaupierre S. Evaluation of an online three-dimensional interactive resource for undergraduate neuroanatomy education. Anat Sci Educ. 2016. 9: 431-9
2. Arantes M, Arantes J, Ferreira MA. Tools and resources for neuroanatomy education: A systematic review. BMC Med Educ. 2018. 18: 94
3. Azer SA. 3D anatomy models and impact on learning: A review of the quality of the literature. Health Prof Educ. 2016. 2: 80-98
4. Brewer DN, Wilson TD, Eagleson R, de Ribaupierre S. Evaluation of neuroanatomical training using a 3D visual reality model. Stud Health Technol Inform. 2012. 173: 85-91
5. Chan S, Conti F, Salisbury K, Blevins NH. Virtual reality simulation in neurosurgery: Technologies and evolution. Neurosurgery. 2013. 72: 154-64
6. Desai A, Stelzer J, Desai S, Berman S. Emerging subspecialties in neurology: Neuro-ophthalmology. Neurology. 2016. 86: e222-4
7. Ekstrand C, Jamal A, Nguyen R, Kudryk A, Mann J, Mendez I. Immersive and interactive virtual reality to improve learning and retention of neuroanatomy in medical students: A randomized controlled study. CMAJ Open. 2018. 6: E103-9
8. Estevez ME, Lindgren KA, Bergethon PR. A novel three-dimensional tool for teaching human neuroanatomy. Anat Sci Educ. 2010. 3: 309-17
9. Gould DJ, Terrell MA, Fleming J. A usability study of users’ perceptions toward a multimedia computer-assisted learning tool for neuroanatomy. Anat Sci Educ. 2008. 1: 175-83
10. Hall S, Lewis M, Border S, Powell M. Near-peer teaching in clinical neuroanatomy. Clin Teach. 2013. 10: 230-5
11. Hall S, Stephens J, Andrade T, Davids J, Powell M, Border S. Perceptions of junior doctors and undergraduate medical students as anatomy teachers: Investigating distance along the near-peer teaching spectrum. Anat Sci Educ. 2014. 7: 242-7
12. Kockro RA, Amaxopoulou C, Killeen T, Wagner W, Reisch R, Schwandt E. Stereoscopic neuroanatomy lectures using a three-dimensional virtual reality environment. Ann Anat. 2015. 201: 91-8
13. Law KM, Geng S, Li TM. Student enrollment, motivation and learning performance in a blended learning environment: The mediating effects of social, teaching, and cognitive presence. Comput Educ. 2019. 136: 1-12
14. Macchi V, Porzionato A, Stecco C, Parenti A, De Caro R. Clinical neuroanatomy module 5 years’ experience at the School of Medicine of Padova. Surg Radiol Anat. 2007. 29: 261-7
15. Nowinski WL, Thaung TS. A 3D stereotactic atlas of the adult human skull base. Brain Inform. 2018. 5: 1
16. Rae G, Cork RJ, Karpinski AC, Swartz WJ. The integration of brain dissection within the medical neuroscience laboratory enhances learning. Anat Sci Educ. 2016. 9: 565-74
17. Shell K, Holt E, Kington A, Mohammed K, Black A, Troup C. Motivation to learn neuroanatomy by cadaveric dissection is correlated with academic performance. Clin Anat. 2020. 33: 128-35
18. Sonagara VJ, Santhirakumaran S, Kalkat HS. The value of near-peer teaching in the medical curriculum. Adv Med Educ Pract. 2018. 9: 63
19. Stephens JR, Hall S, Andrade MG, Border S. Investigating the effect of distance between the teacher and learner on the student perception of a neuroanatomical near-peer teaching program. Surg Radiol Anat. 2016. 38: 1217-23
20. Svirko E, Mellanby J. Attitudes to e-learning, learning style and achievement in learning neuroanatomy by medical students. Med Teach. 2008. 30: e219-27
21. Taylor CF, Kurn OR, Glautier SP, Anbu D, Dean O, Nagy E. The efficacy of interdisciplinary near-peer teaching within neuroanatomical education-preliminary observations. Med Sci Educ. 2021. 31: 387-93