- Department of Biomedicine and Preventative Medicine, Faculty of Medicine and Surgery, University of Rome “Tor Vergata”, Rome, Italy
- Neurosurgery Unit, Dell’Angelo Hospital, Mestre (Ve), Italy
Correspondence Address:
Giovanni Monteleone
Neurosurgery Unit, Dell’Angelo Hospital, Mestre (Ve), Italy
DOI:10.4103/2152-7806.192633
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Monteleone G, Stevanato G. Entrapment of the sciatic nerve at the linea aspera: A case report and literature review. Surg Neurol Int 19-Oct-2016;7:89
How to cite this URL: Monteleone G, Stevanato G. Entrapment of the sciatic nerve at the linea aspera: A case report and literature review. Surg Neurol Int 19-Oct-2016;7:89. Available from: http://surgicalneurologyint.com/surgicalint_articles/entrapment-sciatic-nerve-linea-aspera-case-report-literature-review/
Abstract
Background:Nontraumatic, non-neoplastic sciatic nerve entrapment at the level of the thigh is extremely rare. In its course, in proximity of the linea aspera, the nerve is exposed to unexpected neuropathic syndromes associated with bone disorders.
Case Description:A 67-year-old woman presented with a painful, neuropathic syndrome of the sciatic nerve, not resulting from any trauma and persisting for approximately 2 years. Imaging studies of the thigh showed a delimited zone of hyperostosis in the proximal third of the femoral diaphysis. The symptoms dramatically resolved after the patient underwent neurolysis of the tract of the nerve adjoining to the linea aspera. At the clinical checkup 2 years later, the patient remained free of pain.
Conclusion:The diagnosis of sciatic nerve entrapment at the linea aspera may present considerable difficulties. The clinical history and physical examination sometimes motivate the exploration and neurolysis of the nerve at this site.
Keywords: Linea aspera, sciatic nerve compression, sciatic nerve entrapment, sciatic neuropathy
INTRODUCTION
Of all sciatic neuropathies described in literature, those not dependent on the nerve roots injury have been calculated to be less than 1%.[
In addition to the cases following trauma, expansive processes, and iatrogenic damage to the lower limb,[
The course of the sciatic nerve in the back of the thigh, in closeness to the femur, has been indicated as a critical site of susceptibility of the nervous trunk where uncommon entrapments syndromes may occur.[
CASE DESCRIPTION
A 67-year-old housewife had been treated for 2 years with cycles of strong doses of cortisones and nonsteroidal anti-inflammatory drugs (i.e., Dicloreum) to ease the pain in the back of her left inferior limb.
The medical history, negative for trauma, presented a diagnosis of fibroangiomatosis of the left leg, which had been treated with electrocoagulation and phlebectomy 50 years ago. At the physical examination, both limbs showed diffused varicosis. The Lasègue maneuver of the left limb was positive whereas the Wasserman maneuver was negative. The patellar reflexes, Achilles reflexes, and the plantar reflexes reacted normally and symmetrically. Digital pressure in the posterior region of the left thigh, at the limit between the proximal third and the middle third, provoked slight pain. At this site, the Tinel's sign was positive with paresthesia radiating to the popliteal space and to the calf. The ultrasound scan of the left thigh was negative for lesions of the superficial and deep soft tissues.
A color Doppler ultrasound exam of the lower limbs highlighted ectasic collateral veins of the posterior left thigh and leg and incompetence of the external saphenous vein in the same limb.
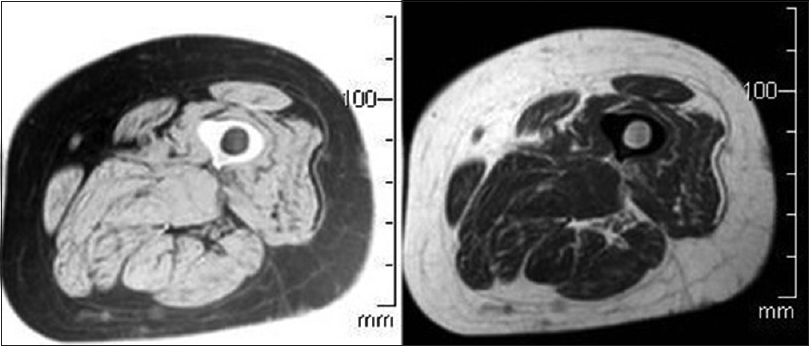
An X-ray exam of the femur showed a delimited zone of hyperostosis in the proximal third of the femoral diaphysis. A magnetic resonance imaging (MRI) scan of the thigh was negative for lesions of periskeletal soft tissue or changes of the bone signal [
Electromyography revealed chronic neurogenic damage without denervation in progress, with a bilateral L5-S1 radicular distribution and slight predominance on the left.
Other radiographic exams of the hips, knee and spine showed diffused moderate or severe arthrosis. The common hematochemical examinations (sedimentation rate, C-reactive protein, and the hemochromocytometric examinations) presented values within the normal range.
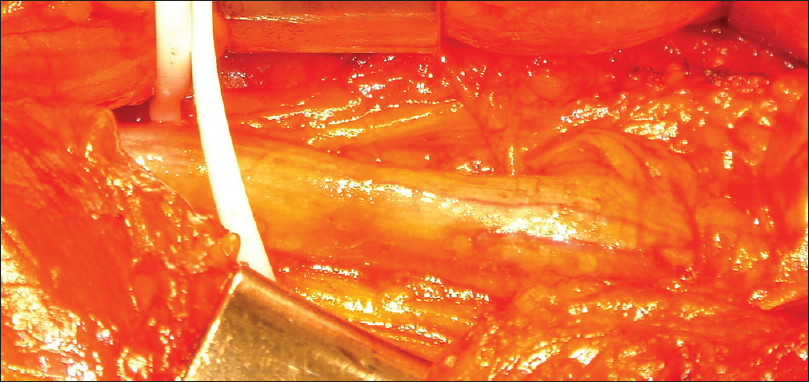
Because of the persisting pain and the findings of the physical examination, we decided to perform a surgical exploration of the sciatic nerve, in the region where the Tinel's sign was positive. Around the nervous trunk, we observed a fibrous tissue which blended in with the tissue of the surrounding muscular fascia. When this was removed, we could note a nerve deformity, with a partial interruption of the vasa nervorum [
On the first postoperative day, the painful symptoms had disappeared and this condition remained unchanged at the last clinical checkup 2 years after surgery.
DISCUSSION
Sciatic nerve entrapment syndromes at the thigh can arise late following penetrating wounds,[
Myofascial bands remaining from hematomas reabsorption,[
We discovered a compression laying in the part of the nervous trunk straddling between the proximal third and the middle third of the thigh. In this tract, the sciatic nerve descends vertically and is separated from the linea aspera by the insertions of the adductor magnus muscle, vastus lateralis muscle, and the short head of the biceps femoris muscle.[
Lignière et al.[
In this case, the femur showed a limited thickening of the cortical bone in proximity to the tract of the entrapped nervous trunk. The thickening developed on the medial side of the femur without contacting the nerve. A reactive process spreading from the femoral cortical bone could have changed the structure and consistency of the soft tissue near to the sciatic nerve, with retraction, and therefore, constricted nervous trunk.
The case presented notable diagnostic difficulties, that are, the unusual site of nerve entrapment, the previous surgery in the same limb, and the high degree of spondylarthrosis, and has precluded a connection between the nerve compression and electromyographic findings.
In addition, according to Petchprapa et al.[
A positive Tinel's sign, especially without an electromyography, is suggestive of entrapment neuropathy, and still represents an indispensable warning for the suspicion of a sciatic nerve compression in this region and to focalize on the diagnostic and therapeutic measures to be taken.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Artico M, Stevanato G, Ionta B, Cesaroni A, Bianchi E, Morselli C. Venous compressions of the nerves in the lower limbs. Br J Neurosurg. 2012. 26: 386-91
2. Banerjee T, Hall CD. Sciatic entrapment neuropathy. Case report. J Neurosurg. 1976. 45: 216-7
3. Barral JP, Croibier A.editorsManual Therapy for the Peripheral Nerves. Munchen, Paris: Elsevier Churching Liviston; 2007. p.
4. Bosma JW, Wijntjes J, Hilgevoord TA, Veenstra J. Severe isolated sciatic neuropathy due to a modified lotus position. World J Clin Cases. 2014. 2: 39-41
5. Carmody C, Prietto C. Entrapment of the sciatic nerve as a late sequela of injury to the hamstring muscles. A case report. J Bone Joint Surg Am. 1995. 77: 1100-2
6. Cattaneo L.editorsAnatomia del sistema nervoso centrale e periferico dell’uomo. Bologna: Monduzzi Editore; 1989. p.
7. Craig A. Entrapment neuropathies of the lower extremity. PM and R. 2013. 5: S31-40
8. Dong Q, Jacobson JA, Jamadar DA, Gandikota G, Brandon C, Morag . Entrapment neuropathies in the upper and lower limbs: Anatomy and MRI features. Radiol Res Pract. 2012. 2012: 230679-
9. Jawish RM, Assoum HA, Khamis CF. Anatomical, clinical and electrical observations in piriformis syndrome. J Orthop Surg Res. 2010. 5: 3-
10. Jones BV, Ward MW. Myositis ossificans in the biceps femoris muscles causing sciatic nerve palsy. A case report. J Bone Joint Surg Br. 1980. 62-B: 506-7
11. Kim DH, Murovic JA, Tiel R, Kline DG. Management and outcomes in 353 surgically treated sciatic nerve lesions. J Neurosurg. 2004. 101: 8-17
12. Lignière GC, Favalli E, Grosso P, Santalena G.editorsSindromi canalicolari degli arti. Milano, Paris, Barcelona: Masson; 1995. p.
13. Miller TA, White KP, Ross DC. The diagnosis and management of Piriformis Syndrome: Myths and facts. Cancer J Neurol Sci. 2012. 39: 577-83
14. Oldershaw JB, Salem A, Storrs BB, Milner B, Omer GE. Sciatic nerve entrapment in the upper thigh caused by an injury sustained during World War II at the battle of Anzio. Case report. J Neurosurg. 2004. 100: 295-7
15. Petchprapa CN, Rosenberg ZS, Sconfienza LM, Cavalcanti CF, Vieira RL, Zember JS. MR imaging of entrapment neuropathies of the lower extremity. Part 1. The pelvis and hip. Radiographics. 2010. 30: 983-1000
16. Saikku K, Vasenius J, Saar P. Entrapment of the proximal sciatic nerve by the hamstring tendons. Acta Orthop Belg. 2010. 76: 321-4
17. Søgaard I. Sciatic nerve entrapment. Case report. J Neurosurg. 1983. 58: 275-6