- Student Research Committee, Department of Oral and Maxillofacial Disease, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran.
- Oral and Dental Disease Research Center, Department of Oral and Maxillofacial Disease, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran.
Correspondence Address:
Fatemeh Lavaee, Oral and Dental Disease Research Center, Department of Oral and Maxillofacial Disease, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran.
DOI:10.25259/SNI_394_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Saman Baghaei1, Fatemeh Lavaee2, Azadeh Roosta1, Delara Amiri1. Evaluation of anxiety disorder in patients with trigeminal neuralgia. 28-Jul-2023;14:266
How to cite this URL: Saman Baghaei1, Fatemeh Lavaee2, Azadeh Roosta1, Delara Amiri1. Evaluation of anxiety disorder in patients with trigeminal neuralgia. 28-Jul-2023;14:266. Available from: https://surgicalneurologyint.com/surgicalint-articles/12464/
Abstract
Background: The aim of this cross-sectional study was to evaluate the relationship between anxiety levels and severity of trigeminal neuralgia (TN) disorder’s chronic orofacial pain during 2019–2020 in Shiraz Dental Faculty.
Methods: In this study, patients with TN disorder who were referred to the Oral Medicine Department of Shiraz Dental Faculty were evaluated. Individuals were selected based on convenience sampling. Finally, 47 patients with TN were recruited in this study. Satisfaction with treatment was recorded based on controlling the patient’s pain, age, sex, and frequency of recurrence, and data were analyzed using SPSS18. The Chi-square test was used to compare the final results. A reliability of more than 95% was considered significant (P
Results: According to the results, the mean ages of participants with TN and control groups were 56.89 ± 10.93 and 37.12 ± 9.55, respectively. The mean value of participants’ age was significantly different between the two evaluated groups (P P P > 0.05). The mean level of anxiety of men and women in TN group was significantly higher than the healthy control women (P = 0.001). The mean levels of anxiety between different age ranges in patients with TN and healthy controls were not different in both evaluated groups (P > 0.05). Patients with TN in different age ranges had higher level of anxiety than healthy controls (P
Conclusion: Patients with TN had significantly higher level of anxiety than healthy participants.
Keywords: Anxiety, Stress, Trigeminal neuralgia
INTRODUCTION
Trigeminal neuralgia (TN) is a common neuralgia with paroxysmal, shock-like pain. The pain is located in distributions of different branches of the fifth cranial nerve. Short-period attacks are followed by painless periods between pain attacks.[
Daroff et al. introduced stress as a defensive response against stimulations and if these stimulations excess the body’s adaptive mechanism, disabling diseases and even death may occur. Anxiety and stress can activate the central mechanism, the adrenal cortex hypothalamus axis. The autonomic nervous system controls chronic, severe, and uncontrolled anxiety which can lead to some diseases.[
The relationship between neuroendocrine (hypothalamic pituitary adrenal axis) and inflammatory immune system has been revealed.[
The patients with temporomandibular disease and pain had higher cortisol serum level.[
The prevalence of migraine in patients with panic disorders was more significant. In addition, anxiety disorders were more prevalent in patients with migraine.[
Due to the inevitable role of stress and anxiety in our lives and their known effects on inflammatory diseases such as rheumatoid arthritis and lupus erythematous,[
MATERIALS AND METHODS
This cross-sectional study has been performed on 47 patients with TN during 2019–2020. The patients had been referred to the Oral and Maxillofacial Department of Shiraz Dental Faculty.
After confirmation of their problem by a specialist, and signing the written consent form, the anxiety level has been assessed by the Hamilton questionnaire.
Patients with psychiatric disorders such as depression, and bipolar disorders, and patients under treatment for such diseases and anxiety disorders have been excluded from the study. Participants who had consumed any medication with a potency of affecting anxiety were excluded too.
Participants of TN group were selected by convenience sampling. Finally, 47 patients with TN were recruited in this study. On the other hand, 40 healthy persons with no emotional criteria were enrolled as central group. Considering TN patients, the status of their pain and demographic data has been registered from their files.
The Hamilton Anxiety Rating Scale is a popular questionnaire for measuring anxiety symptoms and Kar severity.[
This questionnaire has been used widely. It is a clinician-based self-secured survey. This questionnaire has 14 items including both psychological and somatic symptoms following: anxious mood, tension, fear, insomnia, intestinal, depressed mood, somatic (muscular), somatic (sensory), cardiovascular symptoms, respiratory, gastrointestinal, genitourinary and autonomic symptoms, and behavior at interview.
The final score is calculated from 56. A total score of <14 is indicative of mild anxiety, 18–24 is considered as mild to moderate, and 25–30 shows moderate to severe anxiety.
RESULTS
In this cross-sectional study, 87 participants have been enrolled, including 47 patients in TN group and 40 healthy persons in control group.
The data were analyzed by SPSS version 18. Moreover, parametric independent t-test and ANOVA test were used for data analysis (P < 0.05 was considered meaningful). The normality of data distribution was assessed by KS test, which was normal.
Participants’ mean age with TN and control groups were 56.89 ± 10.93 and 37.12 ±9.55, respectively. Furthermore, the mean value of participants’ age was significantly different between the two evaluated groups (P < 0.0001).
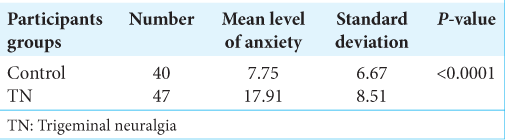
The anxiety level of participants of both evaluated groups is presented in
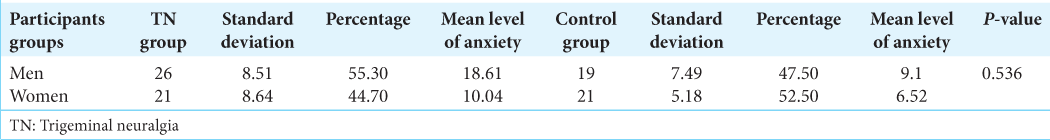
The mean level of anxiety in patients with TN and also in healthy controls did not show a significant difference between men and women (P > 0.05), [
The mean level of anxiety of men and women in TN group was significantly higher than healthy control women (P: 0.001).
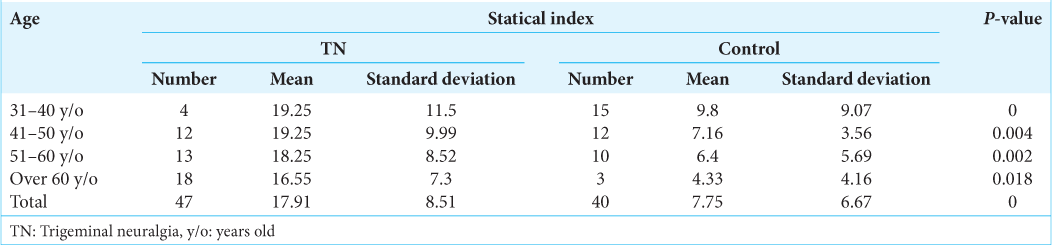
The mean levels of anxiety between different age ranges in patients with TN and healthy controls are presented in
The patients with TN in different ranges of ages had higher level of anxiety than healthy controls (P < 0.05) [
DISCUSSION
In this study, patients with TN had more prominent levels of anxiety than healthy controls. Furthermore, the mean level of anxiety was higher in both men and women with TN than in healthy men and women. In addition, patients with the age range of 31 up to 60 years old had significantly higher levels of anxiety than healthy controls. On the other hand, in each group, the same level of anxiety was reported for men in comparison to women and also for different age ranges.
Some studies regarding the variation of different types of orofacial pain and headaches are discussed below. In a study, Kambalimath et al. reported a positive correlation between myofascial pain dysfunction syndrome (MPDS) and anxiety through higher level of serum cortisol in patients with MPDS than healthy controls.[
In a study, the association between migraine and psychiatric disorders has been reported in both clinical and epidemiological aspects. Hence, the prevalence of psychiatric disorders has been found to be increased among individuals with migraine. Furthermore, the severity of anxiety disorder symptoms was significantly higher in patients with migraine compared to patients without migraine. This study suggests that there is an increased prevalence of migraine headaches among anxiety disorder patients in comparison with the general population.[
Higher level of anxiety has been reported in patients with more severe pain due to TMDs.[
Differences in the prevalence of anxiety disorders in women and men are controversial.[
Anxiety can affect pain perception; therefore, anxiety disorders cause more pain attention in affected patients. These focuses on pain can aggravate pain intensity.[
An emotional physical or psychological response to environmental stimulators is described as anxiety. If this normal reaction becomes chronic, anxiety disorders will arise. Furthermore, anxiety disorders impair daily function and quality of life.[
TN is a disabling painful disorder, which can affect the quality of life greatly. The frequency of painful attacks in addition to its severity is directly related to lower quality of life. The frequency and chronicity of headaches and TN attacks can affect the severity of sleep disturbance.[
Anxiety can affect pain perception; therefore, anxiety disorders cause more pain attention in affected patients. These focuses on pain can aggravate pain intensity.[
Some studies reported that treatment of TN patients could alleviate pain and anxiety disorders caused by TN.[
The environmental situations for sleep, anxiety, and psychological disorders in addition to their prescribed medication can affect the prevalence of sleep disorders. Excluding these confounding factors can homogenize the evaluated population. The socioeconomic and cultural evaluation may be important and can affect sleep quality.[
Cross-sectional studies cannot assess the sleep disturbance precisely. Furthermore, long-term evaluations with follow-ups are also helpful. In addition, differences in culture and socioeconomic variables may affect anxiety level and even pain perception. Furthermore, considering a heterogeneous population can eliminate the confounding factors. Furthermore, larger sample size, using other various sleep disorders indexes and more previous anxiety evaluations are suggested for the next studies.
CONCLUSION
Patients with TN had significantly higher level of anxiety than healthy participants.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
The authors thank the Vice-Chancellor of Shiraz University of Medical Sciences for supporting this research (Grant#20958).
References
1. Arcand M, Juster RP, Lupien SJ, Marin MF. Gender roles in relation to symptoms of anxiety and depression among students and workers. Anxiety Stress Coping. 2020. 33: 661-74
2. Bendtsen L, Zakrzewska JM, Abbott JA, Braschinsky M, Di Stefano G, Donnet A. European Academy of Neurology guideline on trigeminal neuralgia. Eur J Neurol. 2019. 26: 831-49
3. Boardman HF, Thomas E, Millson DS, Croft PR. Psychological, sleep, lifestyle, and comorbid associations with headache. Headache. 2005. 45: 657-69
4. Bonjardim LR, Lopes-Filho RJ, Amado G, Albuquerque RL, Goncalves SR. Association between symptoms of temporomandibular disorders and gender, morphological occlusion, and psychological factors in a group of university students. Indian J Dent Res. 2009. 20: 190-4
5. Chang B, Zhu W, Li S. Effects of depression and anxiety on microvascular decompression outcome for trigeminal neuralgia patients. World Neurosurg. 2019. 128: e556-61
6. Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: A review of the epidemiology, risk and treatment evidence. Med J Aust. 2009. 190: S54-60
7. Cui WQ, Zhang WW, Chen T, Li Q, Xu F, Mao-Ying QL. Tacr3 in the lateral habenula differentially regulates orofacial allodynia and anxiety-like behaviors in a mouse model of trigeminal neuralgia. Acta Neuropathol Commun. 2020. 8: 44
8. Daroff RB, Fenichel GM, Jankovic J, Mazziotta JC, editors. Neurology in Clinical Practice. Netherlands: Elsevier Health Sciences; 2012. p.
9. Devor M, Wood I, Sharav Y, Zakrzewska JM. Trigeminal neuralgia during sleep. Pain Pract. 2008. 8: 263-8
10. Faryabi J, Joolhar M. Treatments’ outcomes of patients suffered from trigeminal neuralgia in Kerman, Iran. J Dent (Shiraz). 2014. 15: 140-6
11. Gambeta E, Chichorro JG, Zamponi GW. Trigeminal neuralgia: An overview from pathophysiology to pharmacological treatments. Mol Pain. 2020. 16: 1-18
12. Ge X, Wang L, Pan L, Ye H, Zhu X, Fan S. Alteration of the cortical morphology in classical trigeminal neuralgia: Voxel-, deformation-, and surface-based analysis. J Headache Pain. 2023. 24: 17
13. Genco RJ, Ho AW, Kopman J, Grossi SG, Dunford RG, Tedesco LA. Models to evaluate the role of stress in periodontal disease. Ann Periodontol. 1998. 3: 288-302
14. Greenberg MS, editors. Ulcerative, vesicular, and bullous lesions. Burket‘s Oral Medicine Diagnosis and Treatment. United States: Lippincott Williams and Wilkins; 2003. p.
15. Goyal S, Jajoo S, Nagappa G, Rao G. Estimation of relationship between psychosocial stress and periodontal status using serum cortisol level: A clinico-biochemical study. Indian J Dent Res. 2011. 22: 6-9
16. Hals EK, Stubhaug A. Mental and somatic co-morbidities in chronic orofacial pain conditions: Pain patients in need of multiprofessional team approach. Scand J Pain. 2011. 2: 153-4
17. Hamilton M. Hamilton anxiety scale. Group. 1959. 1: 10.1037
18. Jia YZ, Li HT, Zhang GM, Wu HY, Zhang SS, Zhi HW. Electroacupuncture alleviates orofacial allodynia and anxiety-like behaviors by regulating synaptic plasticity of the CA1 hippocampal region in a mouse model of trigeminal neuralgia. Front Mol Neurosci. 2022. 15: 979483
19. Katusic S, Beard CM, Bergstralth E, Kurland LT. Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945–1984. Ann Neurol. 1990. 27: 89-95
20. Kambalimath HV, Dixit UB, Thyagi PS. Salivary cortisol response to psychological stress in children with early childhood caries. Indian J Dent Res. 2010. 21: 231-7
21. Khoo A, Dent MT, Oei TP. Group cognitive behaviour therapy for military service-related post-traumatic stress disorder: Effectiveness, sustainability and repeatability. Aust N Z J Psychiatry. 2011. 45: 663-72
22. Luo LY, Lee J, Li KY, Leung YY, Li DT. Psychological outcomes on anxiety and depression after interventions for temporomandibular disorders: A systematic review and meta-analysis. Diagnostics (Basel). 2023. 13: 653
23. Marbach JJ, Lund P. Depression, anhedonia and anxiety in temporomandibular joint and other facial pain syndromes. Pain. 1981. 11: 73-84
24. Melek LN, Devine M, Renton T. The psychosocial impact of orofacial pain in trigeminal neuralgia patients: A systematic review. Int J Oral Maxillofac Surg. 2018. 47: 869-78
25. Melek LN, Smith JG, Karamat A, Renton T. Comparison of the neuropathic pain symptoms and psychosocial impacts of trigeminal neuralgia and painful posttraumatic trigeminal neuropathy. J Oral Facial Pain Headache. 2019. 33: 77-88
26. Obermann M. Pain lateralization in trigeminal neuralgia. Anesth Pain Med. 2012. 2: 46-7
27. Park IH, editors. Pain Related Fear of Movement in Korean Temporomandibular Disorder Patients. South Korea: Seoul National University Graduate School; 2018. p.
28. Pompili M, Serafini G, Di Cosimo D, Dominici G, Innamorati M, Lester D. Psychiatric comorbidity and suicide risk in patients with chronic migraine. Neuropsychiatr Dis Treat. 2010. 6: 81-91
29. Reisner SL, Katz-Wise SL, Gordon AR, Corliss HL, Austin SB. Social epidemiology of depression and anxiety by gender identity. J Adolesc Health. 2016. 59: 203-8
30. Restrepo CC, Vásquez LM, Alvarez M, Valencia I. Personality traits and temporomandibular disorders in a group of children with bruxing behaviour. J Oral Rehabil. 2008. 35: 585-93
31. Sarnvivad P, Bumpenboon A, Chumnanvej S. Retrospective long term outcome following microvascular decompression surgery in Thai patients with trigeminal neuralgia. J Med Assoc Thai. 2013. 96: 801-6
32. Senaratne R, Van Ameringen M, Mancini C, Patterson B, Bennett M. The prevalence of migraine headaches in an anxiety disorders clinic sample. CNS Neurosci Ther. 2010. 16: 76-82
33. Seidel S, Hartl T, Weber M, Matterey S, Paul A, Riederer F. Quality of sleep, fatigue and daytime sleepiness in migraine--a controlled study. Cephalalgia. 2009. 29: 662-9
34. Shiau YY, Chang C. An epidemiological study of temporomandibular disorders in university students of Taiwan. Community Dent Oral Epidemiol. 1992. 20: 43-7
35. Tan CY, Shahrizaila N, Goh KJ. Clinical characteristics, pain, and quality of life experiences of trigeminal neuralgia in a Multi-Ethnic Asian Cohort. J Oral Facial Pain Headache. 2017. 31: e15-20
36. von Eckardstein KL, Keil M, Rohde V. Unnecessary dental procedures as a consequence of trigeminal neuralgia. Neurosurg Rev. 2015. 38: 355-60
37. Wu TH, Hu LY, Lu T, Chen PM, Chen HJ, Shen CC. Risk of psychiatric disorders following trigeminal neuralgia: A nationwide population-based retrospective cohort study. J Headache Pain. 2015. 16: 64
38. Yoshihara T, Shigeta K, Hasegawa H, Ishitani N, Masumoto Y, Yamasaki Y. Neuroendocrine responses to psychological stress in patients with myofascial pain. J Orofac Pain. 2005. 19: 202-8
39. Zakrzewska JM. Multi-dimensionality of chronic pain of the oral cavity and face. J Headache Pain. 2013. 14: 37
40. Zakrzewska JM. Diagnosis and differential diagnosis of trigeminal neuralgia. Clin J Pain. 2002. 18: 14-21
41. Zhuang ZF, Wu HY, Song YY, Li L, Cui X, Yang J. N-Methyl D-aspartate receptor subtype 2B/Ca2+/calmodulin-dependent protein kinase II signaling in the lateral habenula regulates orofacial allodynia and anxiety-like behaviors in a mouse model of trigeminal neuralgia. Front Cell Neurosci. 2022. 16: 981190
42. Zwanzger P. Pharmakotherapie bei Angsterkrankungen. PSYCH up2date. 2016. 10: 135-45






Carlos Francisco Uriarte Nuñez
Posted August 6, 2023, 5:10 am
Mil gracias por su ayuda para entender mejor éstas patologías