- Department of Neurological Surgery, Weill Cornell Medicine, Bronx, New York, United States.
- Weill Cornell Medical College, Bronx, New York, United States.
- Department of Radiation Oncology, Albert Einstein College of Medicine, Bronx, New York, United States.
Correspondence Address:
Susan C. Pannullo
Department of Neurological Surgery, Weill Cornell Medicine, Bronx, New York, United States.
DOI:10.25259/SNI_539_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Swathi Chidambaram1, Sergio W. Guadix2, John Kwon2, Justin Tang3, Amanda Rivera3, Aviva Berkowitz3, Shalom Kalnicki3, Susan C. Pannullo1. Evidence-based practice of stereotactic radiosurgery: Outcomes from an educational course for neurosurgery and radiation oncology residents. 02-Mar-2021;12:77
How to cite this URL: Swathi Chidambaram1, Sergio W. Guadix2, John Kwon2, Justin Tang3, Amanda Rivera3, Aviva Berkowitz3, Shalom Kalnicki3, Susan C. Pannullo1. Evidence-based practice of stereotactic radiosurgery: Outcomes from an educational course for neurosurgery and radiation oncology residents. 02-Mar-2021;12:77. Available from: https://surgicalneurologyint.com/surgicalint-articles/10622/
Abstract
Background: As the field of brain and spine stereotactic radiosurgery (SRS) continues to grow, so will the need for a comprehensive evidence base. However, it is unclear to what degree trainees feel properly equipped to use SRS. We assess the perceptions and comfort level reported by neurosurgery and radiation oncology residents concerning the evidence-based practice of SRS.
Methods: A continuing medical education (CME) course provided peer-reviewed updates regarding treatment with intracranial and spinal SRS. Presentations were given by neurosurgery and radiation oncology residents with mentorship by senior faculty. To gauge perceptions regarding SRS, attendees were surveyed. Responses before and after the course were analyzed using the Fisher’s exact test in R statistical software.
Results: Participants reported the greatest knowledge improvements concerning data registries (P P = 0.026). About 82% of all (n = 17) radiation oncology and neurosurgery residents either agreed or strongly agreed that a brain and spine SRS rotation would be beneficial in their training. However, only 47% agreed or strongly agreed that one was currently part of their training. In addition, knowledge gains in SRS indications (P = 0.084) and ability to seek collaboration with colleagues (P = 0.084) showed notable trends.
Conclusion: There are clear knowledge gaps shared by potential future practitioners of SRS. Specifically, knowledge regarding SRS data registries, indications, and clinical trials offer potential areas for increased educational focus. Furthermore, the gap between enthusiasm for increased SRS training and the current availability of such training at medical institutions must be addressed.
Keywords: Conference, Education, Evidence based, Stereotactic radiosurgery
INTRODUCTION
Stereotactic radiosurgery (SRS) is a highly specialized and complex emerging treatment option for an increasing number of patients with a variety of medical conditions, including malignant and benign tumors, vascular malformations, pain, and psychiatric conditions. A recent survey found that nearly 97% of respondents in a group of radiation oncologists and neurosurgeons in US training programs planned to perform brain and spine SRS on graduation. However, over 50% reported below average understanding of intracranial radiosurgery and more than 80% reported below average understanding of spine radiosurgery; nearly 80% cited inadequacies in both the recognition and management of radiosurgery complications.[
Radiation oncologists and neurosurgeons during training report suboptimal levels of competence in SRS. Left unaddressed, this issue can lead to suboptimal performance in this highly technical specialty. To assess the perceptions and knowledge of SRS, we polled responses from medical students, attendings, and residents who attended a focused course on evidence-based practice of SRS.
MATERIALS AND METHODS
A continuing medical education (CME) course hosted by the Radiosurgery Society was held in January 2019 entitled “Evidence-based Practice of Stereotactic Radiosurgery” to update residents and attendings on the most recent data and guidelines concerning intracranial and spinal SRS. This course was designed to provide data from peer-reviewed medical literature regarding indications and treatment of patients with SRS relevant to a range of practitioners including residents, attending physicians, advanced practice providers, and medical physicists. Other emphasized topics of this course included importance of data collection and use in clinical practice, opportunities for interdisciplinary collaborations to improve clinical and translational research, and patient care. The aims of this course were to provide current and prospective practitioners of SRS with the information needed to select appropriate patients for treatment with SRS, perform treatment with maximal safety and efficacy, and work collaboratively in multidisciplinary teams. The course also focused on increasing resident and SRS practitioner awareness of various SRS data registries and the current landscape of clinical trials.
Presentations were given by neurosurgery and radiation oncology residents and fellows from institutions around the country, with a high representation of residency programs from New York. A panel of attending faculty in neurosurgery and radiation oncology led a discussion after each presentation to critically appraise the research presented and supplement information provided in the presentations with first-hand knowledge and expertise. The faculty residing on the panels was selected for their expertise and engagement in the development and training of neurosurgery and radiation oncology residents at their respective institutions.
An anonymous online survey was administered to attendees both before and after the course with the goal of evaluating baseline competencies and outcomes from the course as well as demographic details from the attendees. Questions included in the survey were aimed at assessing prior experience with SRS techniques as well as levels of anticipated future use of SRS. Survey questions did not mention the use of techniques specific to any device or technology to avoid introducing conflicts of interest. The survey also evaluated current availability of formal SRS training programs for the U.S. residents at their home institutions. Finally, faculty evaluations of resident preparedness for implementation of SRS within their future practice were included in the survey. Responses remained anonymous, except for the identification of the respondent’s field of practice or training.
Statistical analysis
Deidentified data were collected from participants of the SRS course. For matched questions that were asked before and after the conference, comparisons were evaluated across three distinct participant groups using a Fisher’s exact test. Statistical analysis was performed using statistical packages in R programming, with a significance threshold of P < 0.05.
RESULTS
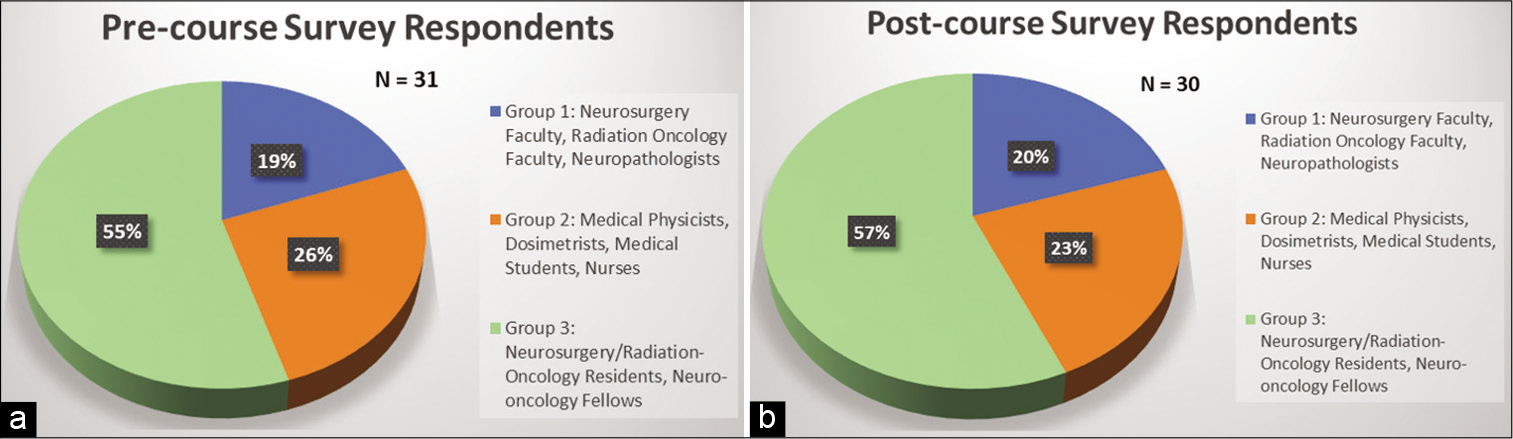
A total of n = 31 participants completed the precourse survey with a response rate of 50% [
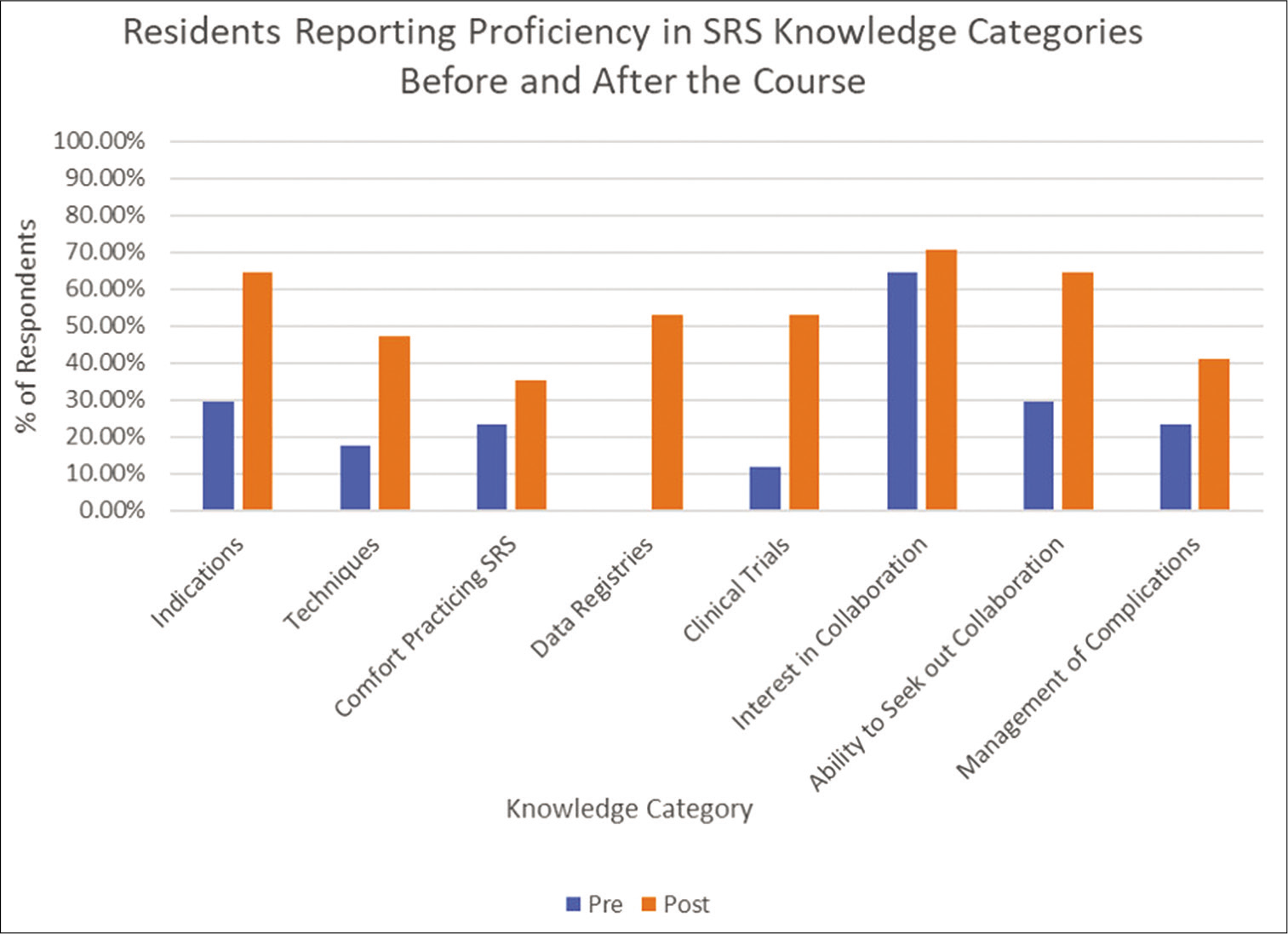
To evaluate the outcomes of the SRS course on current radiosurgery trainees, residents were assessed for their knowledge on eight defined categories of SRS before and after their participation in the course [
Figure 2:
Percentages of neurosurgery and radiation oncology residents and fellows reporting above average (4) or high (5) proficiency in relevant stereotactic radiosurgery knowledge categories before and after the course. A significantly higher percentage of residents and fellows report above average or high proficiency in data registries (P < 0.001) and clinical trials (P = 0.026) after the course compared to reports before the course.
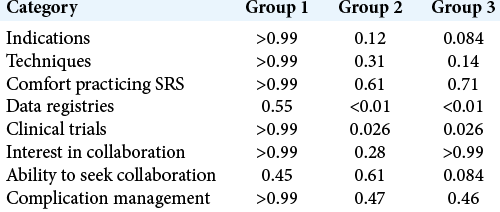
We evaluated whether course participation improved understanding of SRS in three participant groups, as defined above. For each knowledge category, we assessed differences between respondents reporting low proficiency (survey response score = 1, 2, 3) and high proficiency (survey response score = 4, 5) in each group. Group comparisons were analyzed using a Fisher’s exact test, with P-values reported [
Table 1:
P-values obtained from Fisher’s exact test comparing proportions of participants reporting low proficiency (1, 2, and 3) with those reporting high proficiency (4 and 5) before and after the course for different participant groups defined previously. Of note, knowledge of clinical trials and data registries shows significant differences before and after completion of the course for Groups 2 and 3, as defined by P<0.05.
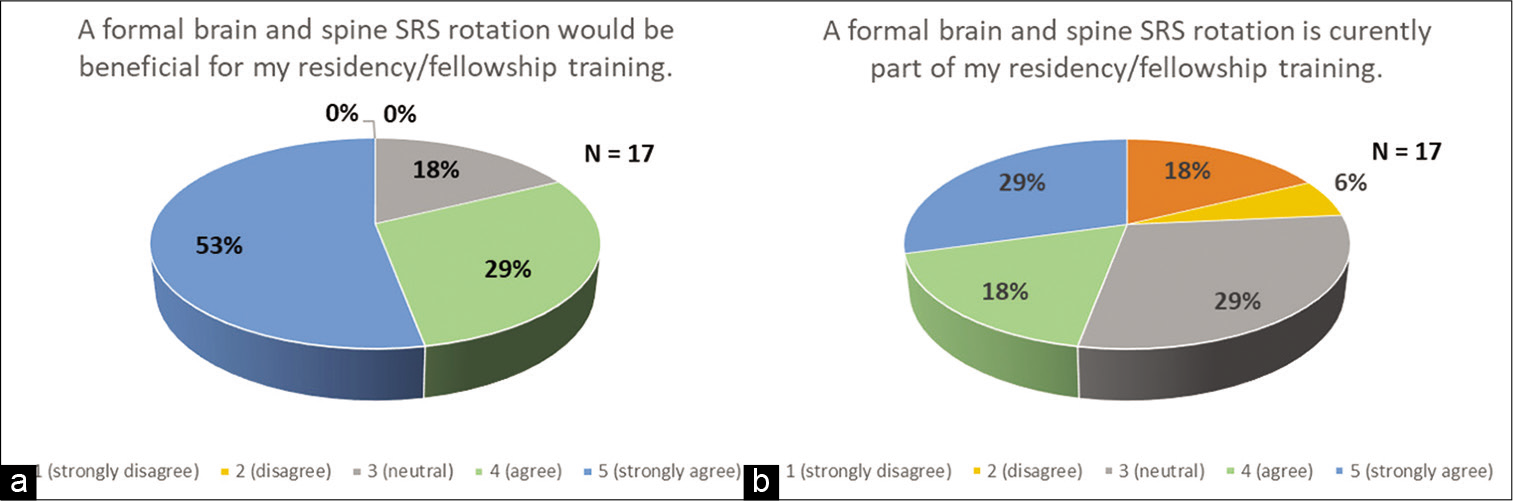
As part of the postcourse survey, residents and fellows were asked to grade on a Likert scale questionnaire whether they believed that a formal brain and spine SRS rotation would prove beneficial as a part of their training at their home institution [
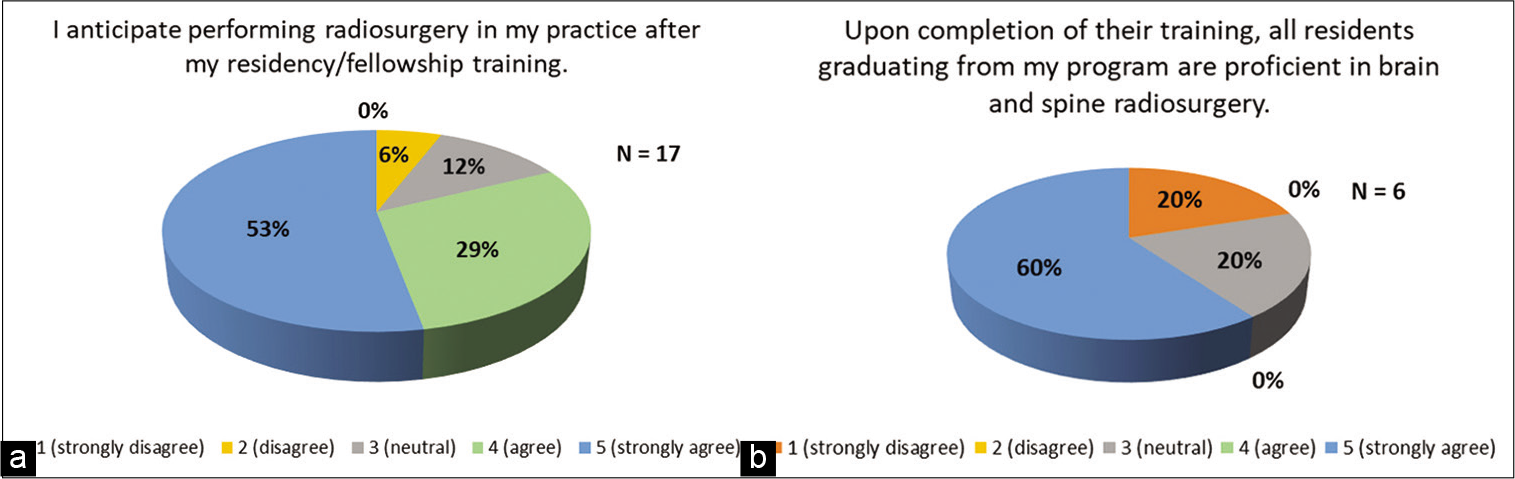
Figure 3:
(a) Perception of the benefits of an stereotactic radiosurgery (SRS) rotation in residency. Percentages correspond to residents and fellows responding to the survey item regarding whether a formal brain and spine SRS rotation be beneficial as part of their training. (b) Reported prevalence of SRS rotation in residency. Percentages correspond to residents and fellows responding to the survey item regarding whether a formal brain and spine SRS rotation is currently part of their training.
The postcourse survey also asked residents whether they anticipated performing radiosurgery in their practice after residency and fellowship training [
DISCUSSION
Results of this survey of neurosurgery and radiation oncology residents indicate a marked discrepancy between the high level of enthusiasm for the compelling, efficient, and effective treatment modality of SRS and the low level of comfort that practitioners express in managing patients and training residents for independent practice. The results further suggest that significant SRS knowledge gaps can be addressed by providing physicians with the data needed to select appropriate patients for treatment with SRS, to perform treatment with maximal safety and efficacy, and to work collaboratively in multidisciplinary teams.
Didactic presentations, such as this course, are a proven format for delivering information regarding medical evidence to a medical audience. The question and answer period and related discussions allow for appropriate clarification of information presented.[
In the survey, 47% of residents and fellows indicated formal SRS training at their home institutions. It is unclear what limitations to SRS training accessibility have been encountered by the remaining 53%. For example, it may be the case that cranial and spinal SRS functions as an independent entity at these institutions or that patients are referred elsewhere if they require SRS. Regardless, this lack of access to SRS training may limit the overall educational opportunities for trainees in neurosurgery and radiation oncology. In addressing the knowledge and practice gaps in radiosurgery highlighted by the results in this study, we must consider incorporating changes in residency training. Nevertheless, the continuing concern of balancing duty hours with optimizing resident training poses a challenge for how to incorporate access to additional skills training related to SRS into an already overburdened curriculum.[
Another method of increasing exposure to SRS during training is by way of postgraduate “boot camps,” simulation-based learning and e-learning resources; all have shown promise in improving performance and in training residents in a time-sensitive manner.[
Several challenges arise when attempting to reform residency training with the above or other methods. Hesitance to include trainees in the treatment planning and delivery of SRS may hinge on fears of introducing new complications to patients from the involvement of nonindependent practitioners. However, a multicenter study demonstrated that resident involvement in the neurosurgical operating room was not a significant factor for postoperative complications in neurosurgery service and that much of the observed difference in postoperative complication rates was attributable to other confounding factors.[
Several limitations of our study merit discussion. First, because New York residency training programs were highly represented in our study, this may limit the generalizability of our findings to reflect more regional training practices. Second, our pre- and postcourse response rates of 50% and 48%, respectively, indicate the potential for response bias. It may be the case that respondents were composed of those most enthusiastic about SRS and thus were more likely to advocate for increased SRS training. However, this is not corroborated by the finding that 53% of respondents were not receiving formal SRS training. Rather, this indicated that the CME course captured a population of residents who lacked formal training in SRS which could benefit from educational sessions taught within this CME framework. Further, response rates of 50% are quite reasonable in most survey studies. Finally, this survey likely could not adequately capture those populations who are not interested in SRS or those who are pursuing SRS with adequate training outside of this CME course. This would require larger sample sizes to capture nationwide trends in SRS training. However, based on these initial findings from neurosurgery and radiation oncology residents, there is some indication that a discrepancy remains between enthusiasm for SRS and access to formal training. Future work with larger participant pools across multiple institutions is warranted to validate these findings within a greater scope. Results of these nationwide investigations may help advocate for increased SRS training and guide modifications to existing residency training.
CONCLUSION
SRS is an increasingly utilized technology in the management of a wide variety of clinical conditions. The results of this study indicate that while residents and practitioners express great enthusiasm for this emerging specialty, they also self-report deficiencies in their ability to recognize indications, perform treatment, and manage complications utilizing SRS techniques within an evidence-based framework. This discrepancy poses a hurdle in the ability to utilize SRS with improved safety and efficacy and suggests a need for residency training reform to incorporate increased, focused exposure to brain and spine SRS for neurosurgery and radiation oncology residents.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to acknowledge the support of this program by Kristine Gagliardi and the Radiosurgery Society.
References
1. Armson H, Lockyer JM, Zetkulic M, Konings KD, Sargeant J. Identifying coaching skills to improve feedback use in postgraduate medical education. Med Educ. 2019. 53: 477-93
2. Fernandez GL, Page DW, Coe NP, Lee PC, Patterson LA, Skylizard L. Boot cAMP: Educational outcomes after 4 successive years of preparatory simulation-based training at onset of internship. J Surg Educ. 2012. 69: 242-8
3. Ganju A, Aoun SG, Daou MR, El Ahmadieh TY, Chang A, Wang L. The role of simulation in neurosurgical education: A survey of 99 United States neurosurgery program directors. World Neurosur. 2013. 80: e1-8
4. Ghobrial GM, Balsara K, Maulucci CM, Resnick DK, Selden NR, Sharan AD. Simulation training curricula for neurosurgical residents: Cervical foraminotomy and durotomy repair modules. World Neurosurg. 2015. 84: 751-5.e1-7
5. Gondi V, Bernard JR, Jabbari S, Keam J, de Amorim Bernstein KL. Results of the 2005-2008 association of residents in radiation oncology survey of chief residents in the united states: Clinical training and resident working conditions. Int J Radiat Oncol Biol Phys. 2011. 81: 1120-7
6. Grady MS, Batjer HH, Dacey RG. Resident duty hour regulation and patient safety: Establishing a balance between concerns about resident fatigue and adequate training in neurosurgery. J Neurosurg. 2009. 110: 828-36
7. Haji FA, Clarke DB, Matte MC, Brandman DM, Brien S, de Ribaupierre S. Teaching for the transition: The Canadian PGY-1 neurosurgery Rookie Camp. Can J Neurol Sci. 2015. 42: 25-33
8. Harrison G, Grandhi R, Monaco EA, Niranjan A, Lunsford LD. The evolution of training in brain stereotactic radiosurgery: A growing part of intracranial neurosurgery. World Neurosurg. 2014. 82: 292-7
9. Heilbrun MP, Adler JR. The 2009 devaluation of radiosurgery and its impact on the neurosurgery-radiation oncology partnership. J Neurosurg. 2010. 113: 10-5
10. Jensen R, O’Rourke D, Warnick R, Sawaya R. Resident training in neurosurgical oncology: Results of the survey of North American training programs by the AANS/CNS section on tumors. J Neurooncol. 2006. 77: 241-6
11. Lehane E, Leahy-Warren P, O’Riordan C, Savage E, Drennan J, O’Tuathaigh C. Evidence-based practice education for healthcare professions: An expert view. BMJ Evid Based Med. 2019. 24: 103-8
12. Lim S, Parsa AT, Kim BD, Rosenow JM, Kim JY. Impact of resident involvement in neurosurgery: An analysis of 8748 patients from the 2011 American college of surgeons national surgical quality improvement program database. J Neurosurg. 2015. 122: 962-70
13. Lunsford LD, Chiang V, Adler JR, Sheehan J, Friedman W, Kondziolka D. A recommendation for training in stereotactic radiosurgery for US neurosurgery residents. J Neurosurg. 2012. 117: 2-4
14. Mansouri A, Witiw CD, Badhiwala JH, Nassiri F, McDonald PJ, Kulkarni AV. National perspectives on the training of neurosurgery residents in stereotactic radiosurgery. Can J Neurol Sci. 2017. 44: 51-8
15. Samuel N, Philteos J, Alotaibi NM, Ahuja C, Mansouri A, Kulkarni AV. Canadian neurosurgery educators’ views on stereotactic radiosurgery in residency training. World Neurosurg. 2018. 112: e208-15
16. Sheehan J, Suh JH, Kavanagh B, Xu Z, Ren L, Sheehan K. Training neurosurgery and radiation oncology residents in stereotactic radiosurgery: Assessment gathered from participants in AANS and ASTRO training course. World Neurosurg. 2018. 109: e669-75
17. Sheehan JP. Resident perceptions of radiosurgical training and the effect of a focused resident training seminar. J Neurosurg. 2010. 113: 59-63
18. Stienen MN, Schaller K, Cock H, Lisnic V, Regli L, Thomson S. eLearning resources to supplement postgraduate neurosurgery training. Acta Neurochir (Wien). 2017. 159: 325-37
19. Yang I, Udawatta M, Prashant GN, Preet K, Mekonnen M, Duong C. Commentary: Stereotactic radiosurgery training for neurosurgery residents: Results of a survey of residents, attendings, and program directors by the American association of neurological surgeons/congress of neurological surgeons section on tumors. Neurosurgery. 2019. 84: E86-91