- Department of Neurosurgery, University of Chicago Medicine, Chicago IL USA.
DOI:10.25259/SNI_268_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Javad Hekmatpanah. Evidence-based treatment of cavernous sinus meningioma. 22-Nov-2019;10:228
How to cite this URL: Javad Hekmatpanah. Evidence-based treatment of cavernous sinus meningioma. 22-Nov-2019;10:228. Available from: http://surgicalneurologyint.com/surgicalint-articles/9772/
Abstract
Background: Cavernous sinus meningioma (CSM) causes gradual ophthalmoplegia and may eventually cause compression of the chiasma. The tumor is often histologically benign, slow growing, and seldom life threatening. Besides visual limitation, ophthalmoplegia causes emotional stress and disability. The tumor is commonly treated by operation, radiation, or both. While effective in varied degrees, the treatments, especially radical operation, are associated with unacceptable mortality and morbidity. The question remains as to what treatment approach is most conducive to longest survival with minimum disability.
Methods: In five patients, operation, radiotherapy, or both were based on presenting symptoms or delayed based on a doctor–patient decision, seeking the most desirable and suitable option that potentially offers longer life with less disability.
Results: Five patients were followed from over 2 to almost 5 decades: two patients are still alive, 25 and 28 years after craniotomy and radiation. One was treated conservatively for 15 years before requiring craniotomy and radiation. One was followed for 45 years without needing craniotomy or radiation, despite enlargement of the tumor. One was followed for 36 years after craniotomy. Patient did not have radiation. Craniotomy consisted of removing enough tumor to diminish symptoms without causing complications. There were no mortalities or complications.
Conclusion: The patient number is not large enough to make a broad conclusion. However, the individualized treatments and long follow-ups, together with detailed literature review, suggest that CSM requires individualized staged treatments based on each patient’s condition. A period of “wait and see” before starting with either surgery or radiation treatment can benefit the patient.
Keywords: Cavernous sinus meningioma, Conservative treatment, Evidence-based treatment
INTRODUCTION
The cavernous sinus is a crowded anatomic region. In addition to cranial nerves III, IV, VI, and the frontal branch of the Vth nerve, it contains the carotid artery and receives venous drainage from the orbit and basilar plexus. Cavernous sinus meningioma (CSM) gradually compresses the above nerves and artery causing varied degrees of unilateral ophthalmoplegia. It may also cause compression of the chiasma over a long period of time. Histologically, the tumor is often benign and slow growing. The tumor is commonly treated by operation or radiation; while effective, both treatments have limited and partial therapeutic effects. Operation can be associated with death and disability; radiation can be associated with long-term complications.
Meanwhile, without treatment, the tumor’s spontaneous growth seldom threatens life and the ophthalmoplegia may take a long time to occur or become disturbing enough to limit the patient’s daily activity. The question then remains as to what approach is most appropriate for each patient to potentially give a longer survival with less disability. This paper represents 2 to almost 5 decades of follow-up of five patients in whom operation, radiotherapy, and/ or conservative management were done based on the evidence of presenting symptoms and a doctor–patient decision as to the best option to offer a longer life with less disability. Despite the small patient number, the results together with a review of pertinent available information from the literature may be of help in planning treatment measures.
MATERIALS AND METHODS
In each patient, the potential treatment risks were assessed and presented to the patient, and a treatment plan was made for what was thought to likely offer the lowest chances for morbidity and mortality. Treatment was started based on presenting symptoms and their degree of impact on the patient’s life, goals, and outlook. No specific routine or guideline was used, for at the time there was none. The patients were followed, so far for over 2 to almost 5 decades. A summary of each patient is presented, and the results are compared with those available in the literature.
Presentations
Patient 1
A 55-year-old man presented in 1970 with mild diplopia caused by partial left VIth nerve palsy. Cerebral angiography showed no specific related abnormality. Due to no definite diagnosis, a plan was made for conservative management. The diplopia was corrected with glasses. Over a period of several years, he developed partial IIIrd nerve palsy with mild drooping of the eyelid, but retained normal vision.
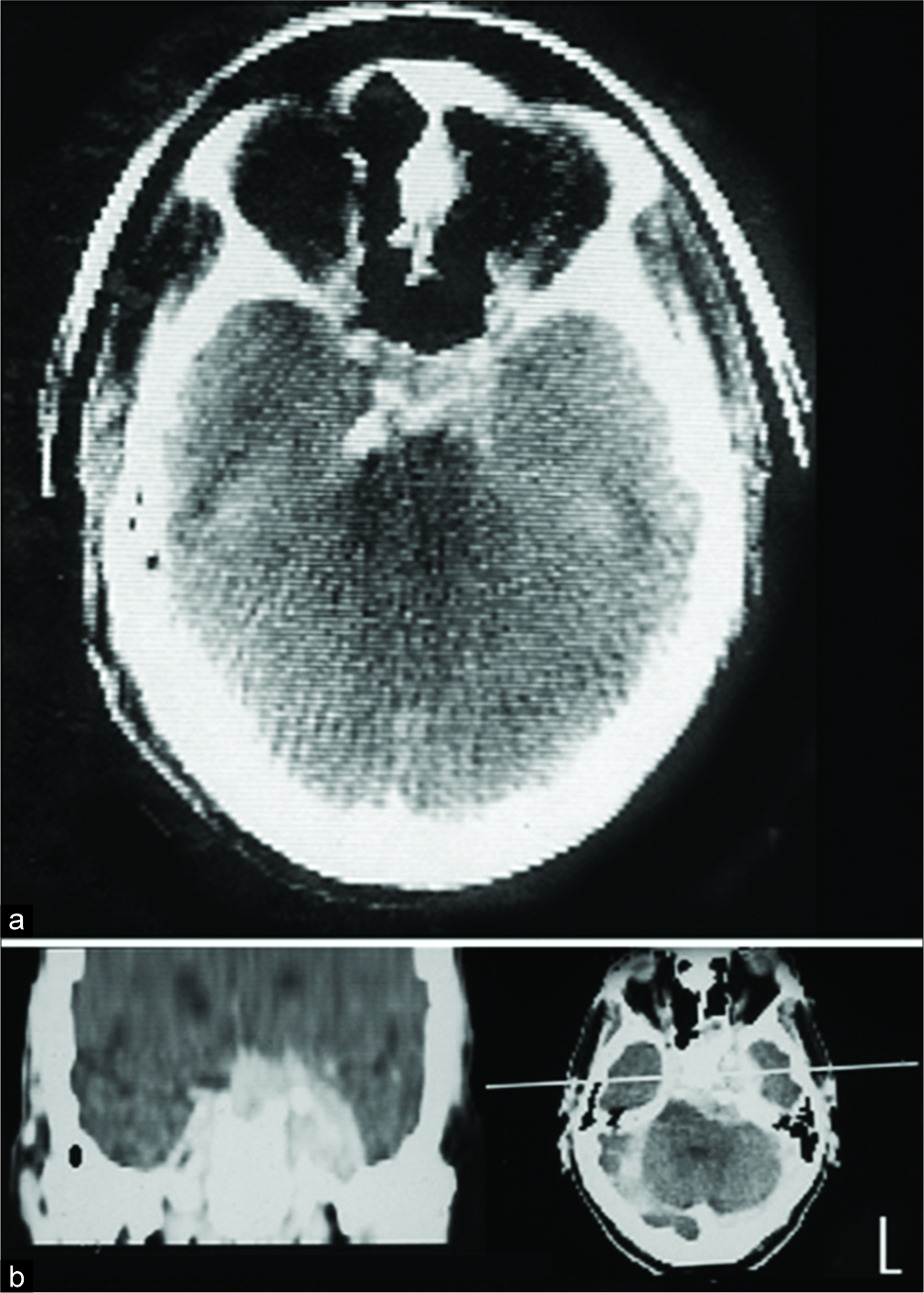
The mild eyelid droop was corrected by a small attachment to his glasses and he was able to continue his work as a dentist. In 1976, what then was called an Electric and Musical Industries (EMI) scan showed a lesion lateral to the sella that could not be easily interpreted [
Patient 2
A 51-year-old woman began having slight diplopia in 1971 caused by the left VIth nerve palsy without much interference with her daily activities. In 1975, a CT scan showed a tumor in the cavernous sinus on the left side [
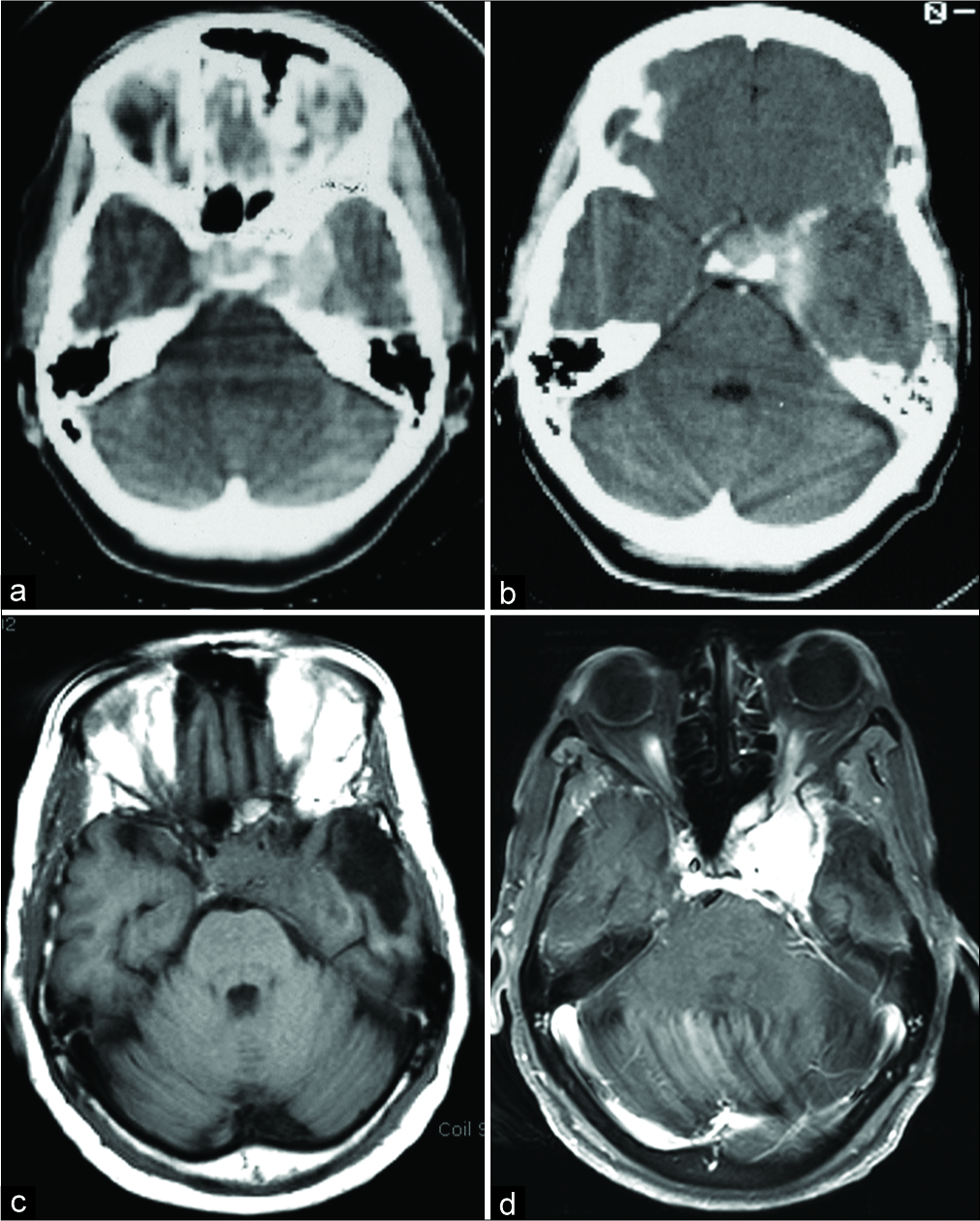
Three years later, the diplopia did interfere with her daily activities, so the left lateral rectus muscle was shorted by an ophthalmologist, which corrected her diplopia. Her condition remained stable without the appearance of any related symptoms, despite enlargement of the tumor. She died 40 years after the onset of diplopia at age 91, from ovarian cancer. The histology of the tumor was never determined, but upon presentation of her scans on numerous occasions, no one doubted meningioma as the diagnosis.
Patient 3
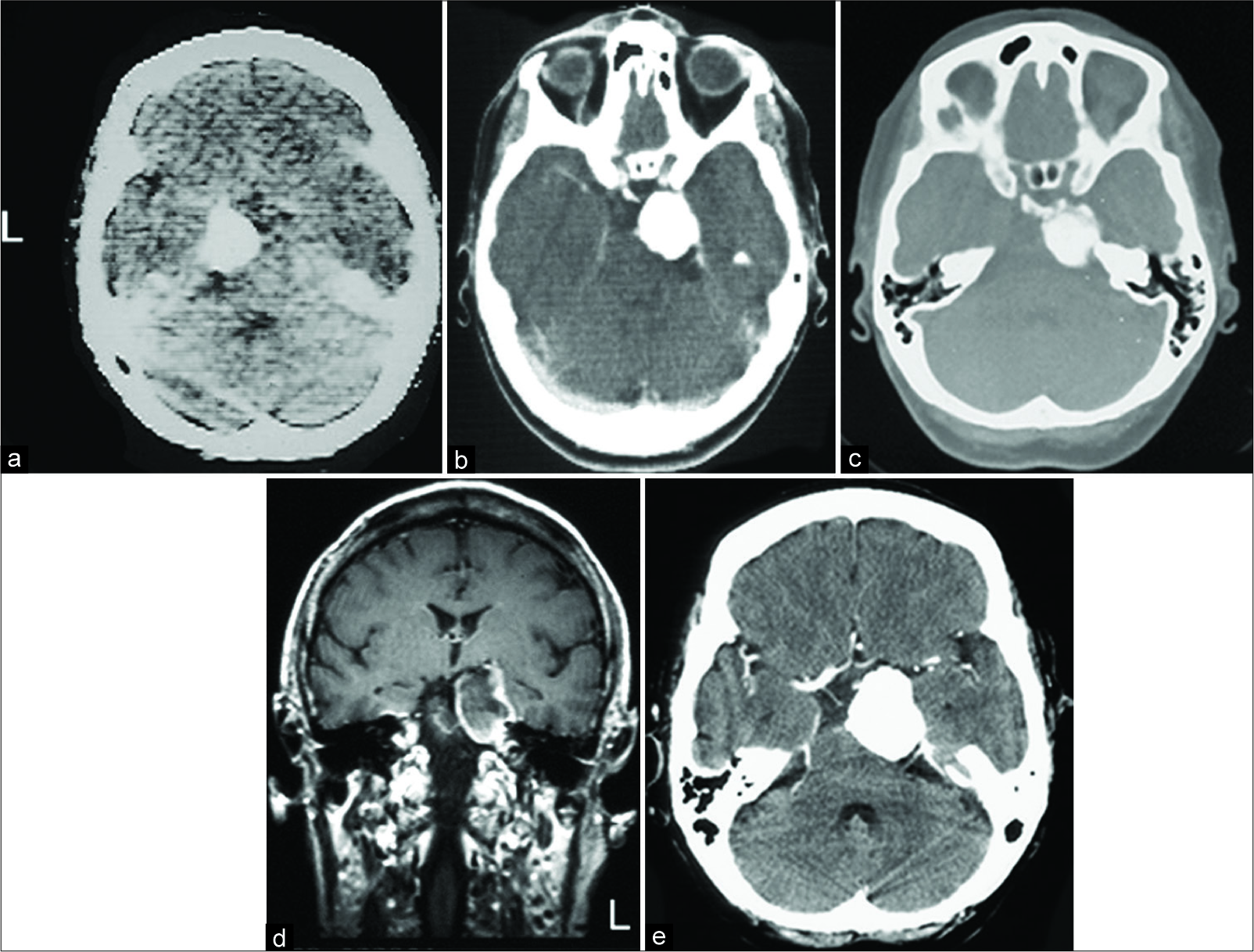
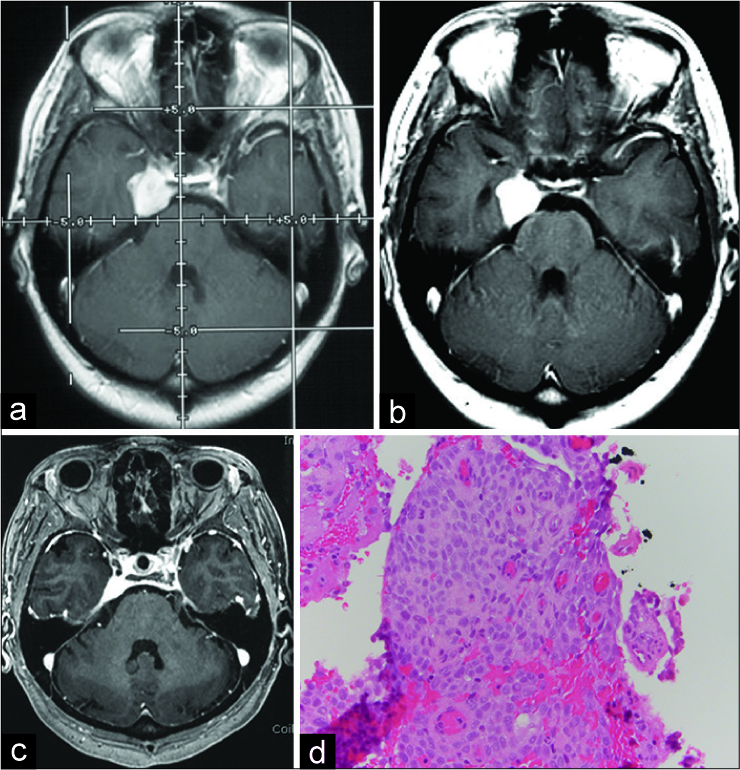
A 38-year-old woman with mild proptosis, double vision from IIIrd nerve palsy, and decreased visual acuity in the left eye, was admitted for evaluation in 1981 [
Patient 4
A 48-year-old man presented in 1994 with diplopia caused by the left VIth nerve palsy. The scan showed CSM (scan no longer available). At operation, partial removal of the tumor was done without entering deep in the cavernous sinus and was followed by conventional radiation therapy. Postoperatively, his diplopia recovered and his scans show the residual tumor [
Patient 5
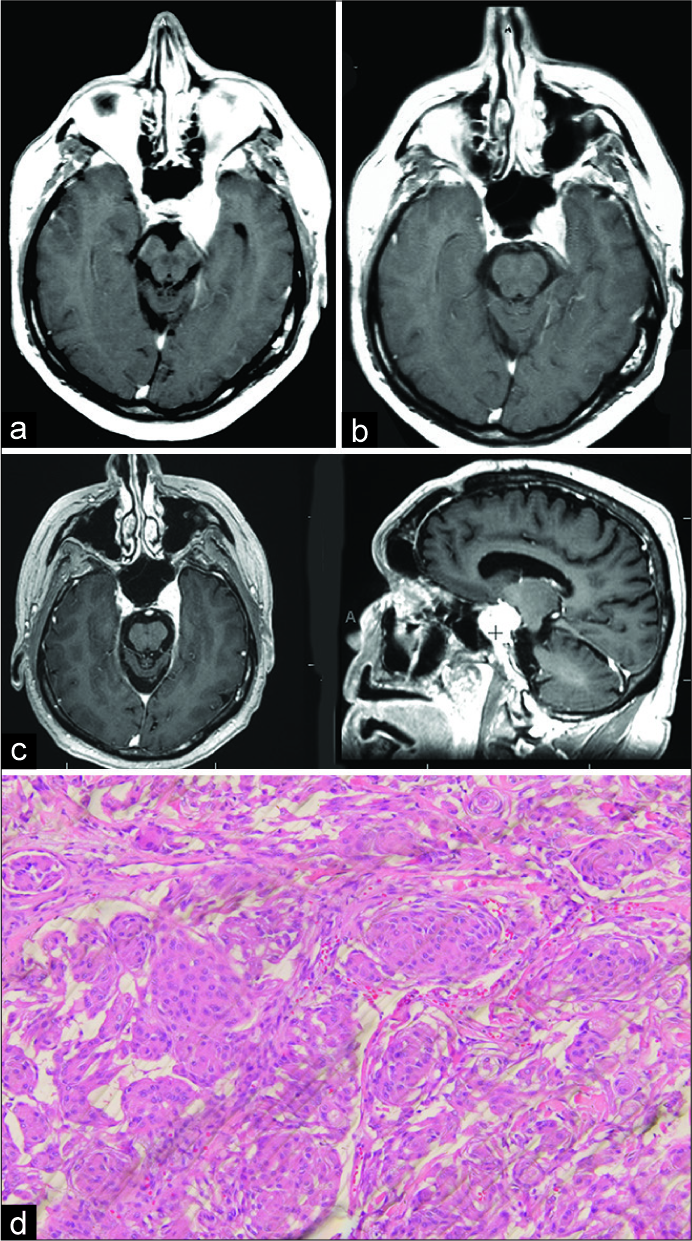
A 30-year-old woman presented in 1991 with diplopia, headaches, and right VIth nerve palsy. A magnetic resonance imaging (MRI) scan from an outside institution (not available) showed a dense lesion lateral to the sella on the right side. She also had galactorrhea and due to that a pituitary tumor located in the cavernous sinus was considered. At operation, the tumor was a part of the cavernous sinus, hard in consistency, and unlike pituitary tumors, it was very solid. Part of the tumor was removed without entering deep into the cavernous sinus, and she received postoperative radiation treatment. The histology done in 1991
Immediately, after the operation, the diplopia and the VIth nerve palsy recovered.
Her galactorrhea recovered, her diplopia has not returned, and she is active, well and working at the writing of this paper 27 years postoperative.
DISCUSSION
The operative and radiological appearance of patients 4 and 5 are very similar. However, due to the elevated prolactin in patient 5 and somewhat different histology, it is of specific interest. For while the appearance of the tumor at operation and radiologic evaluations left no doubt for meningioma, several neuropathologists remained doubtful and could not make up their mind if the tumor was meningioma or pituitary adenoma. The outside preoperative scan for this case is not available, but the radiologist report on the angiogram states: “the finding of a blush which persists into the late venous phase without neurovascularity or early draining veins is compatible with a parasellar meningioma.” Such a flush is characteristic of meningioma and not pituitary adenoma. In addition, the meningeal tail in
Operation and radiation treatment are the two most common treatments for CSM. Especially when radical or aggressive removal of the tumor is involved, these can be associated with relatively higher mortality and morbidity[
DeMonte et al.[
Blake et al.[
Radiation treatment is used as an alternative treatment for CSM. Hasegawa et al.[
Complications of GKR are certainly less than operative complications; nevertheless, they do exist. For example, Skeie et al.[
Meanwhile, Amelot et al.[
Emotional and social complications can also occur: aside from diminished visual capacity, the esthetic disfigurement of ophthalmoplegia has a profound impact on a patient’s life, especially in younger individuals. It diminishes self- image and makes it difficult to find employment despite all qualifications; it can hinder desired social life and personal relationships. It is difficult to understand the bias and stigma a person with even lesser facial disfigurement goes through. The impact stems from the way society perceives disfigurement and the way the person reacts to the way he is treated.
For example, Ryan et al.[
CSM is usually treated by operation, radiation, or both. The available literature, some of which is reported here, indicates that both treatments are effective. However, the degree to which each treatment contributes is difficult to measure; it is mostly assumed. The main goal of any treatment for CSM is to prevent growth of the tumor and to prevent occurrence of ophthalmoplegia. Because the tumor grows slowly over years, it is difficult to assess the degree of the prevention of growth due to radiation treatment. The actual therapeutic effect of radiation is also difficult to measure, unless the ophthalmoplegia is eliminated or at least reduced. The results of an operation on reducing tumor volume and its therapeutic effects are immediately apparent, but the complication rate is higher and growth still can continue.
Furthermore, because the onset of diplopia is independent of the size of the tumor, we do not know when diplopia will occur. Moreover, if it does, shortening of the muscle as in the case of patient 2 or other noninvasive symptomatic treatments as reported by Amelot et al.[
Despite a detailed presentation of potential outcome, few patients can truly understand the impact of the physical disability and facial disfigurement caused by ophthalmoplegia before they actually undergo the operation. If a radical operation is recommended, patients often accept this option, despite the potential postoperative ophthalmoplegia, believing that in order to avoid death they must undergo the operation. However, even untreated, death seldom occurs. Or, a patient may accept operation hoping that an existing ophthalmoplegia recovers. Thus, recommendation for a treatment carries an awesome ethical responsibility. Discussion of blindness, paralysis, and death is not easy to hear. Patients seldom grasp what they will go through and accept the treatment based on trust.
Nevertheless, in the end, a patient needs to know why and for what reason a treatment is recommended and the doctor needs to know why the patient accepts or turns down a treatment. At times, one like patient 1 may be unreasonably hesitant to accept an operation due to older age or other reasons and suffers serious consequences of blindness. Without coercion, such a patient needs encouragement if the planned operation is not as risky as the patient perceives.
As a review by Klinger et al.[
Today, the trajectory of the growth of the tumor can easily be determined by clinical follow-up combined with radiologic studies such as MRI. Certainly, patients in this study showed that disturbing diplopia may not occur for a long time. Thus, there seems to be no urgency in treating CSM with either operation or radiation treatment, especially if it is asymptomatic, or the symptoms are not disturbing to the patient and can be treated with noninvasive treatment. A certain period of “wait and see” can delay the potential complications of an operation and radiation until the evidence indicates their needs based on symptoms and the patient’s desire. Nevertheless, in some patients, as in patients 4 and 5, diplopia can cause considerable limitation in their function to work; in such cases, a limited operation to relieve symptoms, followed by radiation, seems reasonable.
CONCLUSION
Ophthalmoplegia, whether spontaneous or resulting from treatments of CSM, is a serious complication. Facial disfigurement can cause adverse effects in the patient’s self-image, social status, ability to find employment, and personal relationships. Treatment of CSM is seldom urgent. In most patients, it is preferable to wait until there is evidence for the need of operation, radiation, or both. Minor symptoms, such as slight diplopia of lateral gaze, can be treated with corrected eyeglasses or shortening of the lateral rectus muscle of the eye. Operations, especially radical or aggressive ones, are associated with high mortality and morbidity. Radiation treatment slows down and shrinks some tumors but can have some complications over a long time. Thus, in most patients, neither surgery nor radiation needs to be the starting treatment. A period of “wait and see” may be best, until, based on the evidence, operation, radiation, or both become needed.
Declaration of patient consent
The author certifies that he has obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The author acknowledges and appreciates the unrestricted financial philanthropic support of his lab by Mr. Frank Linden, Mr. and Mrs. Samuel Krauss Jr., and Dr. and Mrs. Donald W. King.
References
1. al-Mefty O, Kersh JE, Routh A, Smith RR. The long-term side effects of radiation therapy for benign brain tumors in adults. J Neurosurg. 1990. 73: 502-12
2. Amelot A, van Effenterre R, Kalamarides M, Cornu P, Boch AL. Natural history of cavernous sinus meningiomas. J Neurosurg. 2018. 1: 1-8
3. Blake PY, Miller NR, Long DM. Treatment of cavernous sinus meningiomas. J Neurosurg. 1995. 82: 702-3
4. DeMonte F, Smith HK, al-Mefty O. Outcome of aggressive removal of cavernous sinus meningiomas. J Neurosurg. 1994. 81: 245-51
5. Hasegawa T, Kida Y, Yoshimoto M, Koike J, Iizuka H, Ishii D. Long-term outcomes of gamma knife surgery for cavernous sinus meningioma. J Neurosurg. 2007. 107: 745-51
6. Klinger DR, Flores BC, Lewis JJ, Barnett SL. The treatment of cavernous sinus meningiomas: Evolution of a modern approach. Neurosurg Focus. 2013. 35: E8-
7. Michael AS, Paige ML. MR imaging of intrasellar meningiomas simulating pituitary adenomas. J Comput Assist Tomog. 1988. 12: 944-6
8. Newell R, Marks I. Phobic nature of social difficulty in facially disfigured people. Br J Psychiatry. 2000. 176: 177-81
9. Park KJ, Kano H, Iyer A, Liu X, Tonetti DA, Lehocky C. Gamma knife stereotactic radiosurgery for cavernous sinus meningioma: Long-term follow-up in 200 patients. J Neurosurg. 2018. 1: 1-0
10. Ryan S, Oaten M, Stevenson RJ, Case TI. Facial disfigurement is treated like an infectious disease. Evol Hum Behav. 2012. 33: 639-46
11. Skeie BS, Enger PO, Skeie GO, Thorsen F, Pedersen PH. Gamma knife surgery of meningiomas involving the cavernous sinus: Long-term follow-up of 100 patients. Neurosurgery. 2010. 66: 661-8
12. Sughrue ME, Rutkowski MJ, Aranda D, Barani IJ, McDermott MW, Parsa AT. Factors affecting outcome following treatment of patients with cavernous sinus meningiomas. J Neurosurg. 2010. 113: 1087-92
13. Yu E, Forghani R. Sellar, parasellar and clival region: Skull base cancer imaging. Thieme. J Laryngol Otol. 2018. 132: 759-






Jim Ausman
Posted December 1, 2019, 11:50 am
I have known Dr. Javad Hekmatpanah for over 50 years. This paper is superb and a testimony to him as a fine clinician, wise neurosurgeon and sensitive person. I agree with everything he says. His approach to the treatment of Caveronus Sinus Meningiomas (CSM) is reasonable. Treatment choices should be made on the basis of Risk and Benefit for the patient. No Treatment, is an option and also carries a Risk and Benefit. The lowest risk with the highest benefit is the choice to make in any treatment. In CSM the risks of surgery are high not only surgically but also personally as Javad describes so well. Radiation, including GKR, have long term complications that may not be seen for several decades. If one is uncertain of the diagnosis, either waiting or a performing a biopsy is a reasonable choice to make in deciding risks.
This paper should be read by all residents and neurosurgeons as an example of wisdom and judgment from experience which places the Patient First, not the desires of the doctor or hospital. These are lessons to be learned to become an outstandng physician.
Thank you, Javad, for another example of your excellence as a physician and person.