- Department of Neurosurgery, Kansai Rosai Hospital, Amagaski, Hyogo, Japan.
Correspondence Address:
Shingo Toyota, Department of Neurosurgery, Kansai Rosai Hospital, Amagaski, Hyogo, Japan.
DOI:10.25259/SNI_896_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shingo Toyota, Tomoaki Murakami, Takeshi Shimizu, Kanji Nakagawa, Takuyu Taki. Exoscopic carotid endarterectomy using movable 4K 3D monitor: Technical note. 25-Oct-2021;12:540
How to cite this URL: Shingo Toyota, Tomoaki Murakami, Takeshi Shimizu, Kanji Nakagawa, Takuyu Taki. Exoscopic carotid endarterectomy using movable 4K 3D monitor: Technical note. 25-Oct-2021;12:540. Available from: https://surgicalneurologyint.com/surgicalint-articles/11197/
Abstract
Background: Carotid endarterectomy (CEA) using conventional surgical microscope has been already established as golden standard. Recently, exoscope was introduced into the field of neurosurgery, and various merits of it have been reported. We report the experiences of exoscopic CEA using a movable 4K 3D monitor and discuss the feasibility of it.
Methods: We report a consecutive series of 15 cases of exoscopic CEA for internal carotid artery (ICA) stenosis using a movable 4K 3D monitor between January 2020 and April 2021. We utilized ORBEYE as an exoscope system and a 31-inch movable 4K 3D monitor, which was installed in the Maquet Moduevo ceiling supply unit.
Results: In all 15 cases, the procedures were accomplished only using the ORBEYE. There were no operative complications due to the use of the exoscope. In response to the operative site, the 4K 3D monitor was moved to face the operator. Even when the angle of the visual axis of the exoscope against the horizontal plane was small during the surgical manipulation in the distal portion of ICA, the operator was able to maintain a comfortable posture.
Conclusion: Using the movable 4K 3D monitor, exoscopic CEA can be performed ergonomically. The operator can manipulate the distal portion of the ICA or proximal portion of the common carotid artery in a comfortable posture and face the monitor by adjusting its position.
Keywords: Carotid endarterectomy, Exoscope, Movable monitor, ORBEYE
INTRODUCTION
Carotid endarterectomy (CEA) using a conventional surgical microscope has been established as a gold standard. There are many reports on improving its safety and efficiency.[
For the use of ORBEYE, a 55-inch 4K 3D monitor is usually installed in front of the operator and is often semi-fixed.[
It is highly important that the exoscope enables ergonomically comfortable surgical manipulation even when the angle of the operative visual axis against the horizontal plane is small,[
MATERIALS AND METHODS
Fifteen consecutive patients who underwent CEA using ORBEYE with a 31-inch movable 4K 3D monitor between January 2020 and April 2021 were targeted, and surgical outcomes and complications were examined retrospectively. The 31-inch movable 4K 3D monitor was installed in the Maquet Moduevo ceiling supply unit (Getinge Group Japan. Tokyo, Japan) [
Figure 1:
Set-up of 31-inch movable 4K 3D monitor. The 31-inch movable 4K 3D monitor installed in the Maquet Moduevo ceiling supply unit. The monitor can be moved in response to the operative site. (a) A 31-inch movable 4K 3D monitor (b) Maquet Moduevo ceiling supply unit c: ORBEYE™ main body d: A 55-inch 4K 3D monitor (covered by blue cloth).
The indication of CEA was as follows: In symptomatic patients, the degree of stenosis should be >50%, and in asymptomatic patients, the degree of the stenosis should be greater than 80%. Carotid artery stenosis was evaluated using the NASCET method.[
The mean age of the patients was 76 ± 6-years-old, 93% were male, and 53% had right-side carotid stenosis. Of the patients, 33% were symptomatic and 63% had unstable plaque. The mean degree of stenosis was 71 ± 12%.
Surgery was performed under general anesthesia in all patients. The patient was placed in a supine position and the head rotated to the contralateral side. The Lone Star disposal retractor system (CooperSurgical, Inc., Trumbull, Connecticut, USA) was utilized as previously reported.[
All endarterectomy procedures were performed using the Pruitt-Inahara Carotid Shunt system (LeMaitre Vascular, Inc., Burlington, Massachusetts, USA). In all cases, systemic heparinization (3000–5000 IU) was performed just before insertion of the shunt system, without reversal with protamine.
RESULTS
In all 15 cases, the procedures were accomplished only using the exoscope. There were no operative complications due to the use of ORBEYE.
In response to the operative site, the 4K 3D monitor was moved to face the operator. When the distal portion of the ICA was manipulated, the visual axis of the exoscope was directed rostral and the monitor was moved to the rostral side [
Figure 2:
Simulation of right-side CEA (a) When the distal portion of the ICA is manipulated, the visual axis of the exoscope is set to the rostral direction and the monitor is moved to the rostral side to face the operator. (b) When the proximal portion of the CCA is manipulated, the visual axis is set to the caudal direction and the monitor is moved to the caudal side. *31-inch movable 4K 3D monitor. CEA: Carotid endarterectomy, ICA: Internal carotid artery, CCA: Common carotid artery.
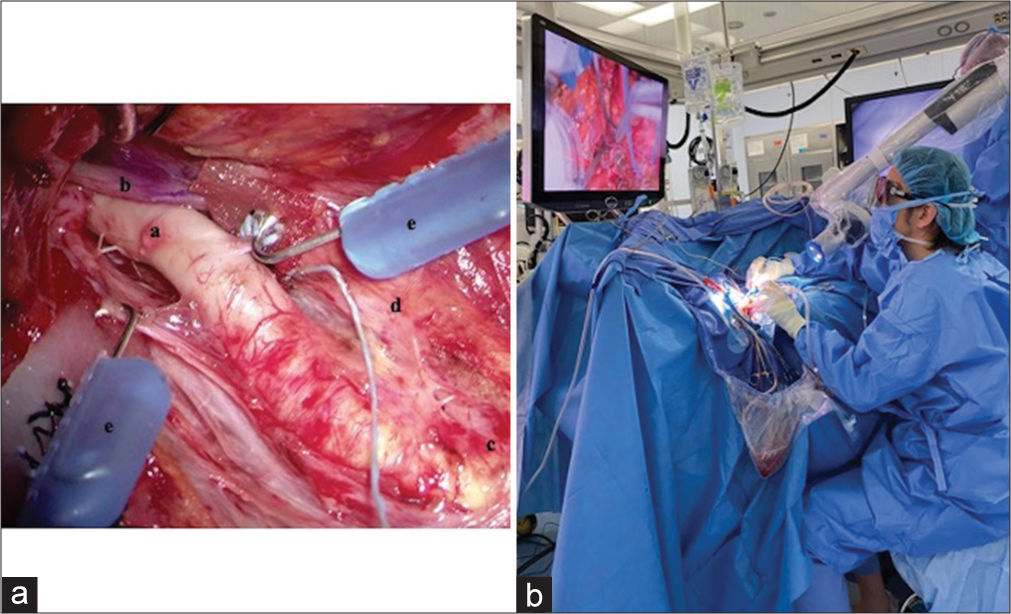
Figure 3:
(a) Intraoperative photograph during CEA for right symptomatic ICA stenosis. In order to expose the distal ICA portion as much as possible, the hypoglossal nerve and distal ICA portion were dissected and mobilized using ORBEYE. The connective tissue surrounding the ICA was hooked and lifted to obtain a shallow operative field. a: distal ICA portion, b: the hypoglossal nerve, c: carotid bifurcation, d: external carotid artery, e: hooks of the Lone Star retractor system. (b) Intraoperative posture of the operator during CEA for right symptomatic ICA stenosis. Using ORBEYE, the operator was able to maintain a comfortable posture even when the angle of the operative visual axis against the horizontal plane was small during surgical manipulation in the distal portion of the ICA. CEA: Carotid endarterectomy, ICA: Internal carotid artery.
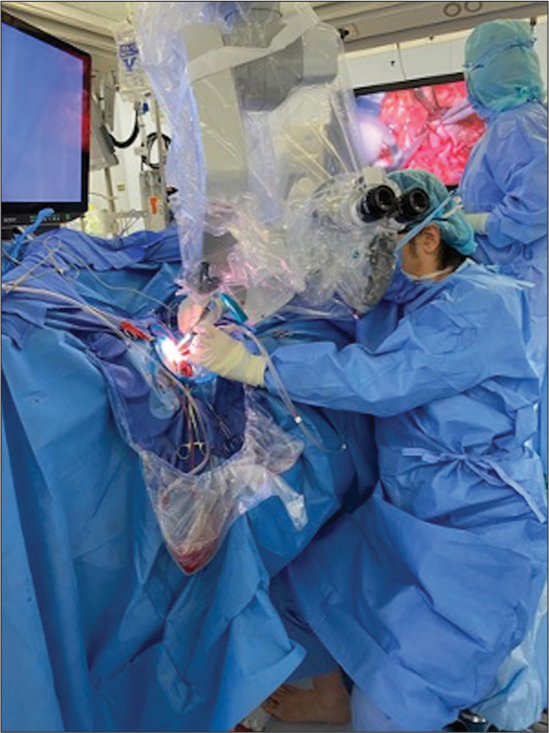
Figure 4:
Intraoperative posture of the operator during CEA for right symptomatic ICA stenosis. Using a conventional surgical microscope, the distance from the operator’s eyes to the operative field increased, and he was forced to be in a posture that extended his arms when the angle of the visual axis against the horizontal plane was small during surgical manipulation in the distal portion of the ICA. CEA: Carotid endarterectomy, ICA: Internal carotid artery.
The average time of microsurgical procedure in this series was 175 ± 17 min. It was 159 ± 41 min in our previous series of 15 cases using conventional microscope. There was no significant difference.
DISCUSSION
CEA reduces the risk of disabling stroke or death in patients with advanced carotid stenosis, and its effectiveness has been demonstrated in many large studies.[
CEA for high cervical ICA stenosis is considered technically demanding because of the difficulty in dissecting the distal ICA portion.[
The usefulness of exoscopes, including ORBEYE, has been reported in neurosurgical fields,[
To the best of our knowledge, there are no reports to emphasize the advantages of the movable monitor in the use of exoscopes. For the use of ORBEYE, a 55-inch 4K 3D monitor is usually installed in front of the operator and is semi-fixed.[
CONCLUSION
Using a movable 4K 3D monitor, exoscopic CEA can be performed ergonomically. In response to the operative site, the 4K 3D monitor was moved to face the operator. Even when the angle of the visual axis of the exoscope against the horizontal plane was small during surgical manipulation in the distal portion of the ICA, the operator was able to maintain a comfortable posture.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Batzdorf U, Gregorius FK. Surgical exposure of the high cervical carotid artery: Experimental study and review. Neurosurgery. 1983. 13: 657-61
2. 3. Frim DM, Padwa B, Buckley D, Crowell RM, Ogilvy CS. Mandibular subluxation as an adjunct to exposure of the distal internal carotid artery in endarterectomy surgery, Technical note. J Neurosurg. 1995. 83: 926-8 4. Furui T, Hasuo M. Indwelling double-balloon shunt for carotid endarterectomy, Technical note. J Neurosurg. 1984. 60: 861-3 5. Iwata T, Toyota S, Kudo A, Nakagawa K, Shimizu T, Murakami T. Microsurgery “Under the Eaves” using ORBEYE: A case of dural arteriovenous fistula of the anterior cranial fossa. World Neurosurg. 2020. 138: 178-81 6. Izumo T, Ujifuku K, Baba S, Morofuji Y, Horie N, Matsuo T. Initial experience of ORBEYE surgical microscope for carotid endarterectomy. Asian J Neurosurg. 2019. 14: 839-42 7. Kondo T, Ota N, Göhre F, Kinoshita Y, Noda K, Kamiyama H. High cervical carotid endarterectomy-outcome analysis. World Neurosurg. 2020. 136: e108-18 8. Matsumoto K, Yamamoto S, Turuzono K, Yoshimura K, Ohta T, Hayakawa T. Fixative method of carotid shunt using a Sugita’s fenestrated aneurysm clip as a device in carotid endarterectomy technical note. Surg Neurol. 2006. 66: 328-30 9. Murai Y, Sato S, Yui K, Morimoto D, Ozeki T, Yamaguchi M. Preliminary clinical microneurosurgical experience with the 4K3-dimensional microvideoscope (ORBEYE) system for microneurological surgery: Observation study. Oper Neurosurg (Hagerstown). 2019. 16: 707-16 10. Barnett HJM, Taylor DW, Haynes RB, Sackett DL, Peerless SJ. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991. 325: 445-53 11. Nossek E, Schneider JR, Kwan K, Kulason KO, Du V, Chakraborty S. Technical aspects and operative nuances using a high-definition 3-dimensional exoscope for cerebral bypass surgery. Oper Neurosurg (Hagerstown). 2019. 17: 157-63 12. Oertel JM, Burkhardt BW. Vitom-3D for exoscopic neurosurgery: Initial experience in cranial and spinal procedures. World Neurosurg. 2017. 105: 153-62 13. Sasaki T, Nakamura Y, Yomo S, Sekiguchi Y, Kodama K, Ichikawa Y. The posterior cervical triangle approach for high carotid artery exposure in carotid endarterectomy. J Neurosurg. 2012. 116: 680-4 14. Shima T, Okada Y, Nishida M, Yamane K. A newly developed shunt system for carotid surgery: T-shaped silicone shunt tubes and clamping devices: Technical note. Neurosurgery. 1998. 42: 1182-4 15. Shimizu T, Toyota S, Nakagawa K, Murakami T, Mori K, Kishima H. Retrosigmoid approach in the supine position using ORBEYE: A consecutive series of 14 cases. Neurol Med Chir (Tokyo). 2021. 61: 55-61 16. Sundt TM, Houser OW, Sharbrough FW, Messick JM. Carotid endarterectomy: Results, complications, and monitoring techniques. Adv Neurol. 1977. 16: 97-119 17. Toyota S, Kumagai T, Goto T, Mori K, Taki T. Utility of the lone star retractor system in microsurgical carotid endarterectomy. World Neurosurg. 2017. 101: 509-13 18. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004. 351: 1493-501