- Department of Neurological Surgery, Rutgers New Jersey Medical School, Newark, United States
- Department of Neurological Surgery, Rutgers Robert Wood Johnson Medical School, New Brunswick, New Jersey, United States.
Correspondence Address:
Christopher Markosian, Department of Neurological Surgery, Rutgers New Jersey Medical School, Newark, New Jersey, United States.
DOI:10.25259/SNI_757_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Markosian C1, Yan RE2, Rallo MS2. Exploring neurosurgical oncology in medical school. Surg Neurol Int 08-Dec-2023;14:418
How to cite this URL: Markosian C1, Yan RE2, Rallo MS2. Exploring neurosurgical oncology in medical school. Surg Neurol Int 08-Dec-2023;14:418. Available from: https://surgicalneurologyint.com/surgicalint-articles/12661/
Dear Editor,
We believe that neurosurgical oncology necessitates additional layers of preparation, given its multidisciplinary nature. Brain and spine tumor care is split into multiple steps involving different specialists at each, including diagnosis (encompassing neuroradiology, neuropathology, and neuro-oncology), technicality (neurosurgery and neuroanesthesiology), and treatment (neurooncology, radiation oncology, and palliative care). The complex nature of this workflow requires that the neurosurgical oncologist, often deemed to be the overseeing physician alongside the neuro-oncologist, “speak the language” of their physician colleagues. Such an approach would ensure the best possible patient outcomes based on the current treatment landscape.
Despite the importance of honing interdisciplinary expertise, neurosurgical oncologists often have difficulty pursuing such opportunities due to time constraints. A minimum of 11 years of medical education and training is required to become an attending neurosurgeon. Neurosurgical oncology typically entails the completion of additional training, such as in the form of a Ph.D. degree and/or fellowship in neuro-oncology. The 7-year residency prioritizes the mastery of surgical skills and provides exposure to some, but not all, aspects of neuro-oncology. As attending physicians, neurosurgeons continue to focus on sharpening operative skills.
Simply put, time away from the operating room hurts technical ability in neurosurgery. In comparison, the practice of oncology is often enhanced by time away from the clinic when spent on research and/or independent study of the literature. This provides an opportunity to improve patient outcomes through acquired knowledge of cutting-edge diagnostic and therapeutic strategies. Because the neurosurgical oncologist must achieve the same level of proficiency as a neuro-oncologist, one potential solution is to extend the timeline of oncology-focused education in reverse.
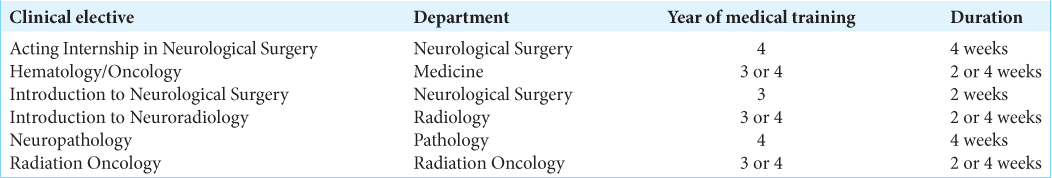
We propose that medical school presents the ideal time for the preparation of future neurosurgical oncologists. The broad-scope knowledge acquired in foundational topics along with physiology, pathology, and pharmacology provides a ripe opportunity to delve into the field. Furthermore, medical students are unable to develop their surgical adeptness at this stage. To achieve this objective, a set of clinical electives across relevant disciplines, including hematology/oncology, neurosurgery, neuropathology, neuroradiology, and radiation oncology, can be pursued by 3rd- and 4th-year medical students outside of the core curriculum at Rutgers New Jersey Medical School [
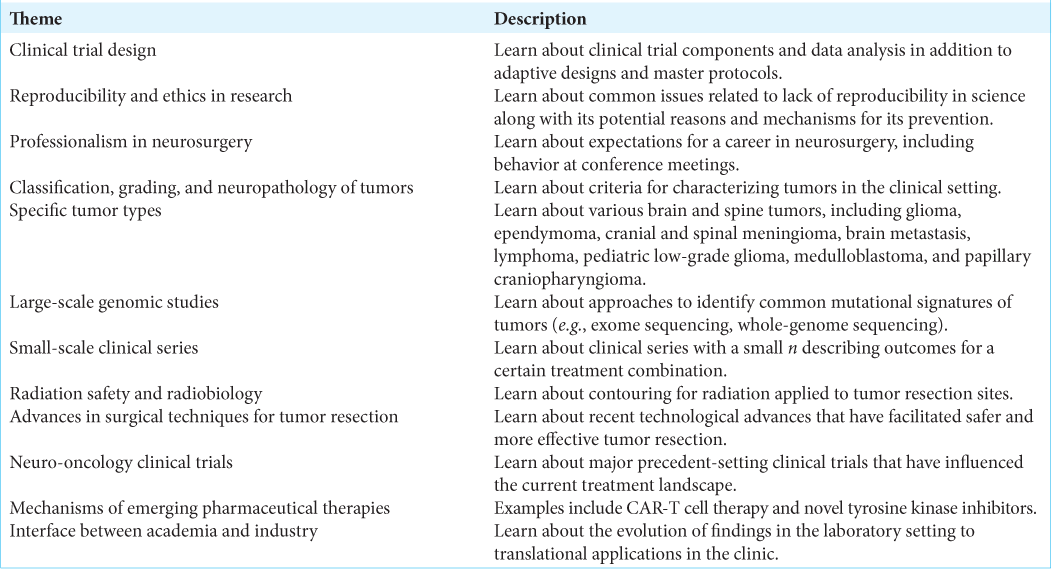
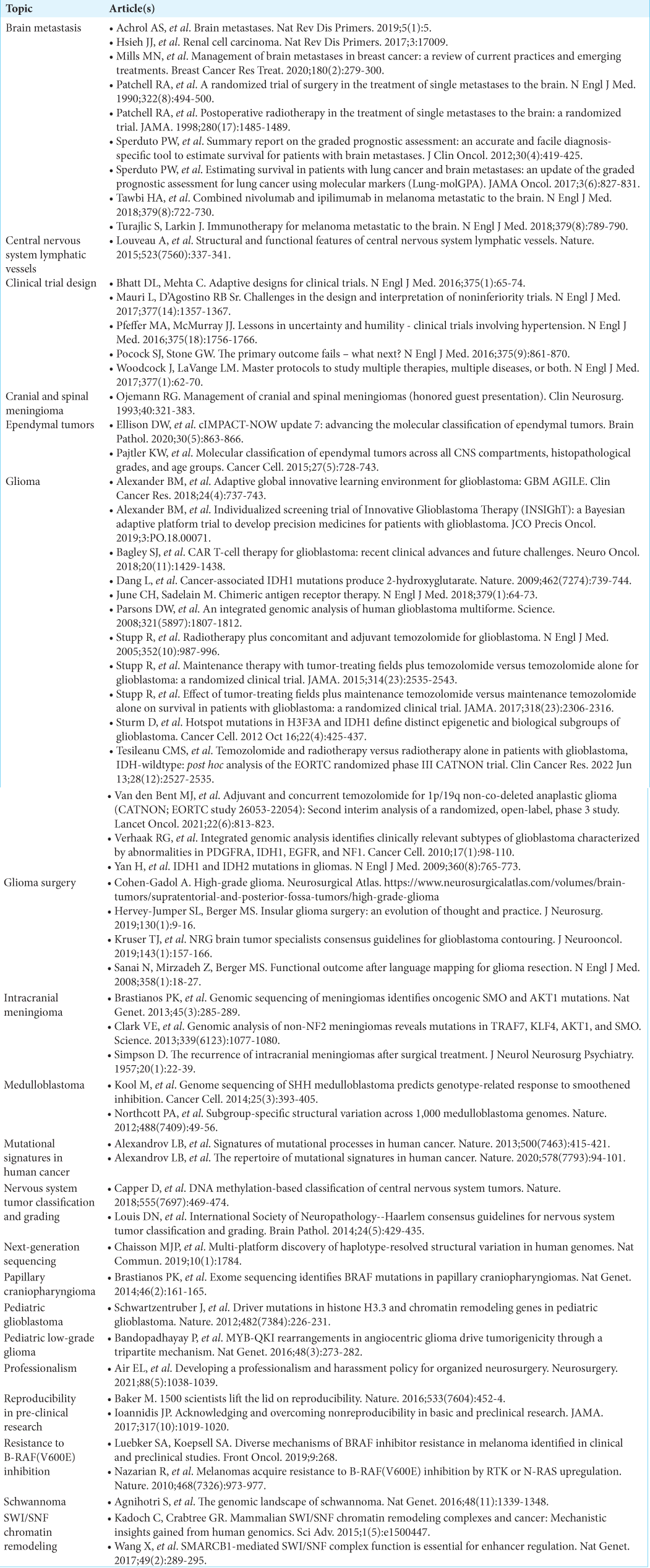
In addition, inspired by the curriculum established for neuro-oncology fellows and the World Health Organization Classification of Tumors of the Central Nervous System, we recently organized extracurricular focused learning sessions that covered essential principles of neuro-oncology over 2 years under the direction of a neurosurgical oncologist [
Furthermore, we discovered that ongoing separate experiences in bench and clinical research created learning opportunities for one another. We also occasionally elected to have one participant, sometimes a guest physician from another field, to lead the discussion on a preferred topic.
Such a model of learning was anecdotally successful in facilitating an apprehension of neurosurgical oncology and related specialties.
To the best of our knowledge, a similar approach to prepare neurosurgical oncologists beginning in medical school has not been implemented elsewhere. There is precedent for such a curriculum, given that neuro-oncology fellows do not necessarily focus on technical skills and are given dedicated time for research and independent learning. Habits developed early in the timeline of a neurosurgical oncologist will pave the way for a productive career. In addition, interactions with different physicians at an early stage, whether through tumor boards or conference meetings hosted by professional organizations, such as the American Association for Cancer Research, American Association of Neurological Surgeons, American Society for Radiation Oncology, American Society of Clinical Oncology, Congress of Neurological Surgeons, and Society for Neuro-Oncology, can further facilitate interdisciplinary learning. Such an initiative may also be effective for neurosurgery residents, though careful planning around their intensive schedules is essential for its successful execution. We believe that a comparable strategy can be implemented at other medical schools for the training of future neurosurgical oncologists.
Ethical approval
Not applicable.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
We thank Dr. Pankaj K. Agarwalla (Department of Neurological Surgery, Rutgers New Jersey Medical School) for his mentorship in addition to guidance and participation in our focused learning sessions.