- Department of Neurology, National Neurosciences Institute, King Fahad Medical City, Riyadh, Saudi Arabia
- Department of Intervention Neuroradiology, Medical Imaging Administration, King Fahad Medical City, Riyadh, Saudi Arabia
- Department of Clinical Laboratory Administration, National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia.
- Department of Neurosurgery, National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia.
Correspondence Address:
Naim Izet Kajtazi, Department of Neurology, National Neurosciences Institute, King Fahad Medical City, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_348_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Naim Izet Kajtazi1, Juman Al Ghamdi2, Razan Al Amoudi2, Amna Zakri2, Wafa Al Shakweer3, Mohammed Bafaquh4. Extensive cerebral venous thrombosis after resection of third ventricle colloid cyst. 08-Jun-2023;14:201
How to cite this URL: Naim Izet Kajtazi1, Juman Al Ghamdi2, Razan Al Amoudi2, Amna Zakri2, Wafa Al Shakweer3, Mohammed Bafaquh4. Extensive cerebral venous thrombosis after resection of third ventricle colloid cyst. 08-Jun-2023;14:201. Available from: https://surgicalneurologyint.com/surgicalint-articles/12354/
Abstract
Background: The third ventricle colloid cyst (CC) is a benign growth usually located in the third ventricle and can cause various neurological symptoms, including sudden death. Modern surgical interventions may still result in a wide range of complications and cerebral venous thrombosis (CVT) is among them.
Case Description: A 38-year-old female with an existing diagnosis of diabetes mellitus (DM) and hypothyroidism and a 6-month history of headaches, blurred vision, and vomiting presented to our clinic 3 days after the headaches became excessively severe. Neurological examination on admission revealed bilateral papilledema without any associated focal neurological deficits. Brain computed tomography and magnetic resonance imaging confirmed the presence of a third ventricle CC and associated non-communicating hydrocephalus involving the lateral ventricles. As a result, the patient underwent emergency bilateral external ventricular drainage (EVD) insertion followed by a third ventricular CC excision under neuronavigation through a right frontal craniotomy. Twelve days postoperatively, the patient developed further headaches followed by a generalized tonic-clonic seizure that led to no postictal neurological deficits. Nonetheless, computed tomography venography of the brain revealed extensive thrombosis of the superior sagittal sinus, inferior sagittal sinus, right sigmoid sinus, and right internal jugular vein. A newly diagnosed CVT was treated with intravenous heparin. The patient was discharged with warfarin, which was discontinued after 12 months. Ten years after her illness, she remained stable and free from any neurological deficits but still suffered from chronic mild headaches.
Conclusion: A preoperative venous study should be performed in all cases to gain a better understanding of the venous anatomy. We advocate meticulous microsurgical techniques to protect the venous system surrounding the foramen of Monro and reduce the amount of retraction during surgery.
Keywords: Cerebral venous thrombosis, Colloid cyst, Foramen of Monro, Thalamostriate vein, Third ventricle
INTRODUCTION
The third ventricle colloid cyst (CC) is a benign growth usually located in the third ventricle, at or near the foramen of Monro, which is situated at the anterior aspect of the third ventricle of the brain.[
CC can cause various symptoms, including headaches, diplopia, memory issues, and vertigo, but rarely result in sudden death. Symptomatic CCs most commonly cause headaches, nausea, and vomiting secondary to obstructive hydrocephalus. In these cases, non-communicating hydrocephalus is precipitated by blocking the egress of cerebrospinal fluid (CSF) from the lateral ventricles at the foramen of Monro, which connects the lateral and third ventricles.[
Patients diagnosed with CC usually require surgical intervention, which may include CSF diversion with a ventriculoperitoneal shunt (VP shunt), aspiration of the cyst through endoscopic, open, or stereotactic approaches, or open surgery through the interhemispheric fissure or transcortical or transsulcal approaches. Although these procedures are safe and can be performed in many institutes, there is no consensus among neurosurgeons regarding the most optimal surgical strategy, primarily due to personal preferences and the complication rates associated with different options. The most common postsurgical complications are memory deficit, bleeding, and seizures, while cerebral venous thrombosis (CVT) involving the cortical veins, deep venous system, or larger sinuses is rare, occurring in approximately 1.5% of CC cases involving intracranial surgery. Thus, one such case was the focus of this study.
CASE REPORT
Clinical presentation
A 38-year-old female with DM and hypothyroidism presented to our hospital with 6-month history of headaches, blurred vision, and vomiting, noting that the headache severity suddenly worsened 3 days previously. Brain computed tomography (CT) scans from her local hospital were reviewed, indicating increased intracranial pressure associated with dilated lateral ventricles. A neurological examination performed on admission revealed bilateral papilledema without any other focal signs.
Laboratory and radiological investigations
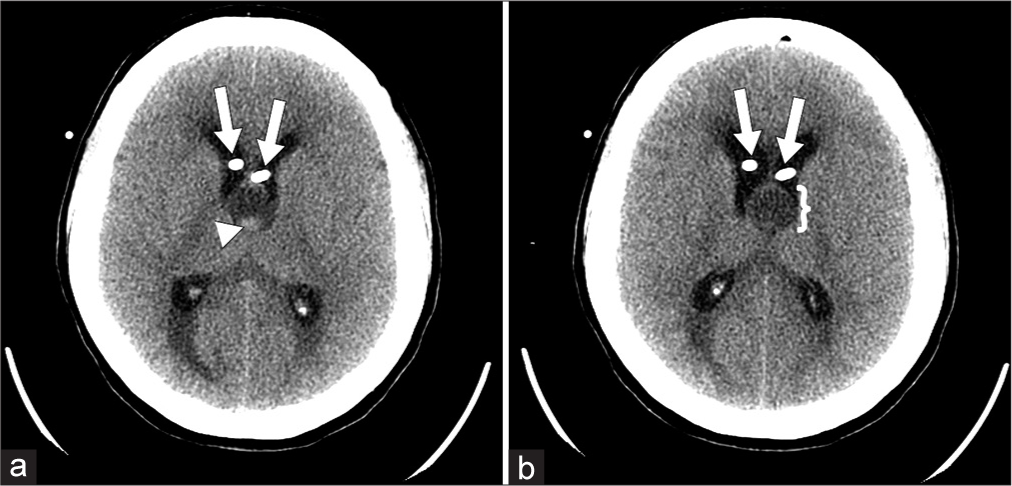
The findings yielded by all initial basic laboratory investigations were within normal limits. As shown in
Figure 1:
Brain computed tomography brain without contrast: (a and b) well-defined hypodense lesion seen at the foramen of Monroe with a hyperdense area in the dependent portion (arrowhead in image a and brackets in image b), most likely representing a colloid cyst. Two linear intraventricular hyperdensities represent bilateral external ventricular drainage shunt insertion (arrows).
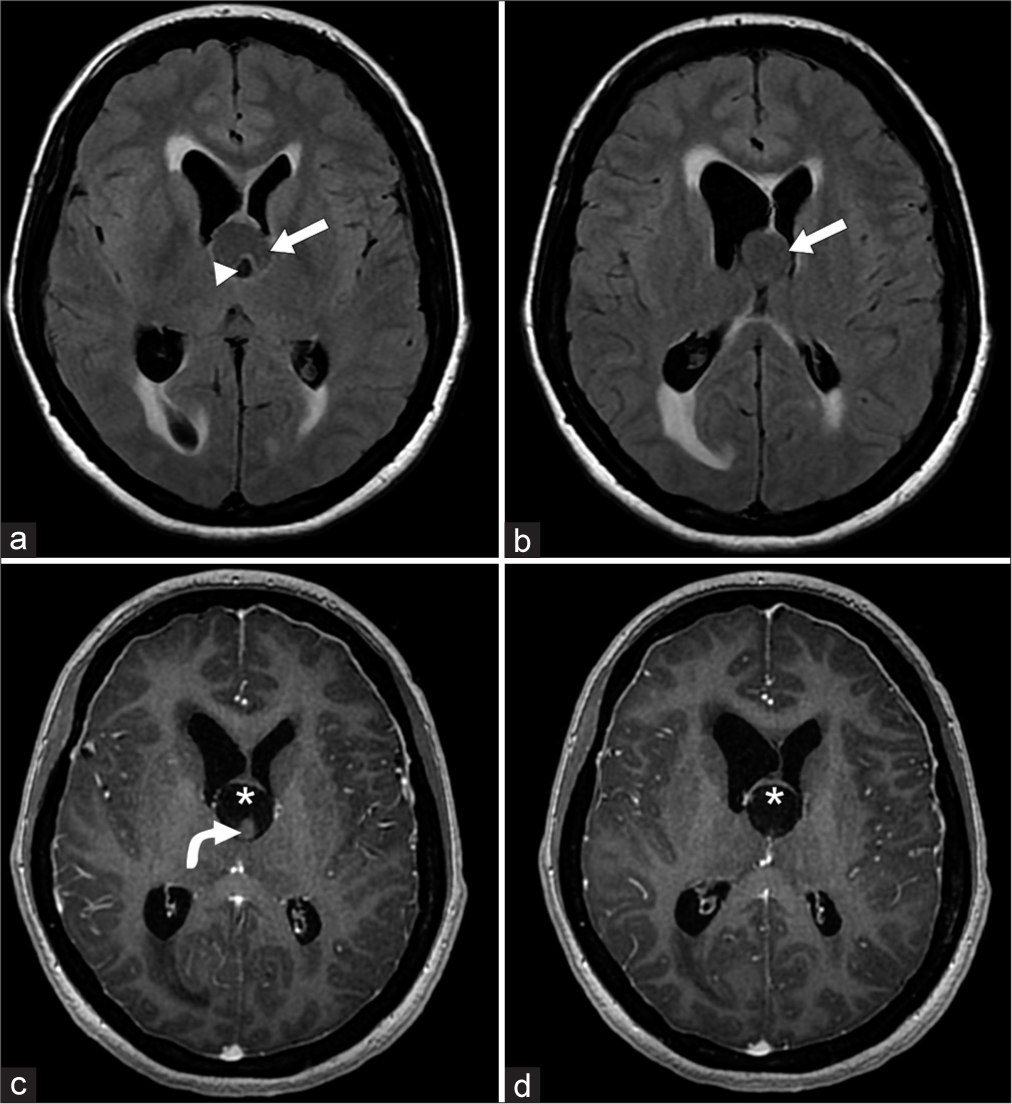
Figure 2:
Brain MRI with contrast. Axial FLAIR (fluid attenuated inversion recovery). Image a and b Legend: A well-defined predominantly cystic lesion (arrow) measuring approximately 19 mm in diameter at the foramen of Monroe. The hypointense area within the cystic lesion corresponds to hyperdensity at the dependent portion on the prior CT scan (arrowhead). The lesion causes anterior displacement of the forniceal pillars and lateral deviation of the posterior part of both frontal horns of lateral ventricles. No significant suppression relative to CSF was observed in the FLAIR images. Brain MRI, axial 3D with contrast. Image c and d Legend: No significant enhancement is observed in the lesion after contrast administration (asterisk) or in the isointense area within the cystic lesion (curved white arrow).
Interim treatment
The patient underwent emergency bilateral external ventricular drainage (EVD) insertion and was subjected to a third ventricular CC excision under neuronavigation through a right frontal craniotomy 3 days later. Although the CC was large and strongly adhered to the roof of the third ventricle, contained gelatinous material with a whitish cheesy solid portion, and was surrounded by the plexus of veins, the procedure was performed without any complications.
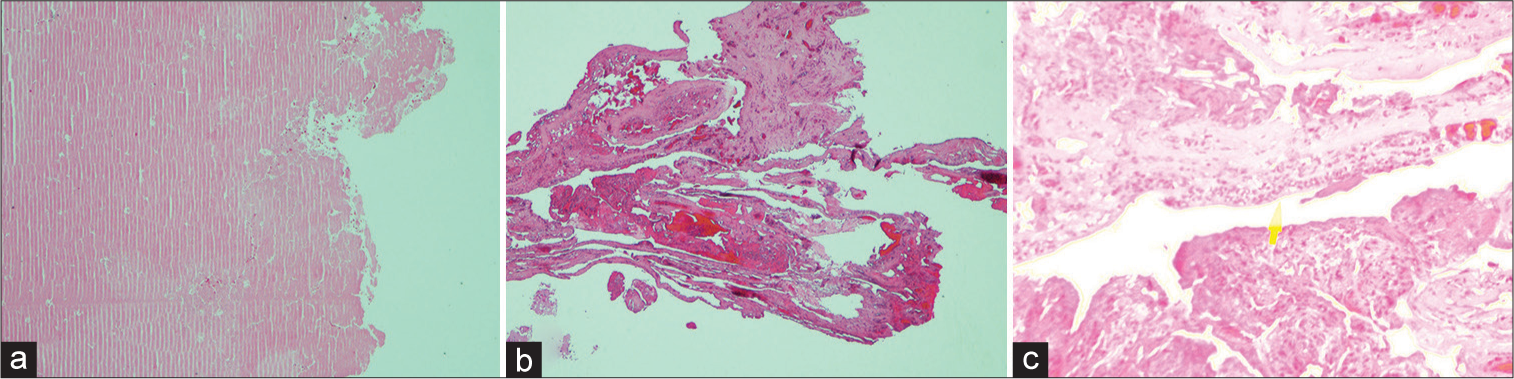
Histopathology findings
Histological sections from the cyst wall showed a small piece of fibrovascular tissue with no epithelial lining, consistent with a CC, whereas the section from the cyst nodule contained eosinophilic, colloid-like material [
Follow-up and clinical outcome
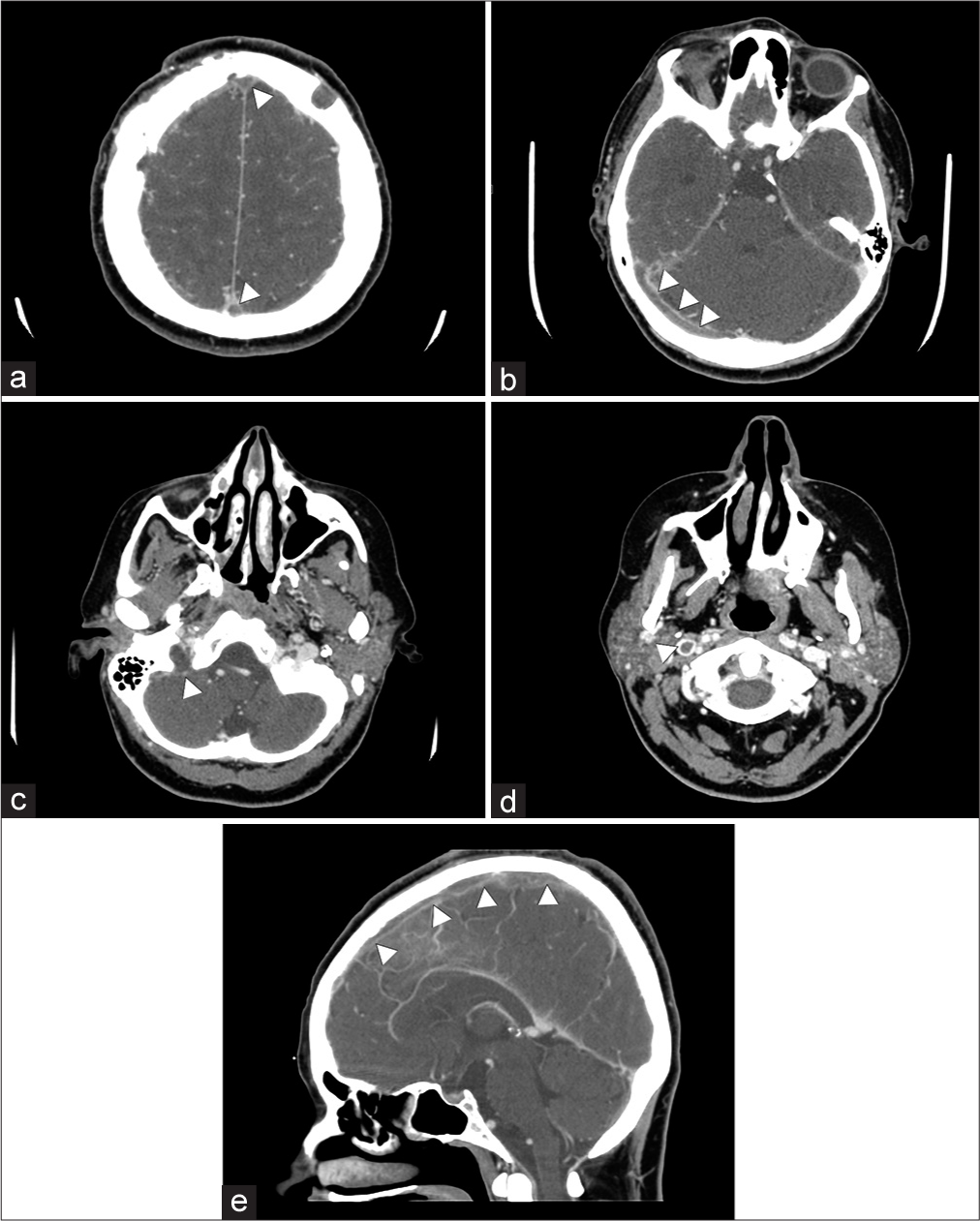
Twelve days after surgery, the patient developed further headaches. A few days later, she experienced a 5-min generalized tonic-clonic seizure, during which she bit her tongue and her eyeballs rolled upward. At this time, she also noticed oozing from the surgical site on the right side of the head but reported no new neurological deficits. However, as shown in
Figure 4:
Brain computed tomography (CT) venography. (a-d) CT venography shows an extensive filling defect at the level of the anterior and posterior superior sagittal sinus (arrowheads in a), right transverse sinus (arrowheads in b), right sigmoid sinus (arrowhead in c), and right internal jugular vein with peripheral calcification (arrowhead in d). (e) Sagittal CT venogram shows an extensive filling defect of the superior sagittal sinus (arrowheads in e).
DISCUSSION
Brain tumors involving the third ventricle are rare and are estimated to account for only 0.6−0.9% of all cases.[
To avoid venous infarction, Apuzzo recommended vascular imaging as a part of the preoperative planning process and emphasized the importance of preserving the venous system when treating CC cases.[
The case reported here pertains to a patient with DM and hypothyroidism in whom extensive venous infarction occurred 20 days after CC surgical excision. The thrombosis rate in this patient was extensive and was attributed to injury to a single draining vein; according to the surgeon, retraction to the frontal lobe was appropriate, no retraction injury occurred, and the utilization of bipolar coagulation was not aggressive. The surgical team, however, noticed a complex venous plexus surrounding the CC, which could be just a congested normal vein that was difficult to tell as there were no preoperative venous images, and intraoperatively, the CC was large enough to allow appropriate evaluation of these venous plexuses. It is also worth noting that the transcorticaltransventricular approach is less likely to lead to venous infarction than the midline approach (i.e., transhemispherictranscallosal approach).
We posit that even though the patient had no notable medical history (apart from DM and hypothyroidism), a non-diagnosed transient or hypercoagulable state led to this unfortunate complication. Thus, we suggest that the coagulopathic state of each patient should be carefully evaluated before the CC surgical procedure, while also reducing the amount of retraction during surgery, particularly lateral retraction. We advocate meticulous microsurgical techniques to protect the venous system surrounding the foramen of Monro, during which excessive bipolar coagulation should be avoided. Finally, preoperative vascular imaging should be performed to understand the anatomy of the venous system and improve identification of veins that could be at risk.[
CONCLUSION
This case highlights the possibility of cerebral venous thrombosis as a potential complication after third ventricle colloid cyst surgery. A preoperative venous study should be performed in all cases to gain a better understanding of the venous anatomy. We advocate meticulous microsurgical techniques to protect the venous system surrounding the foramen of Monro and reduce the amount of retraction during surgery.
Learning points
Utilization of the appropriate surgical technique is essential, especially when the patient has significant ventricular dilatation and hydrocephalus, for which the transcortical-transventricular approach is suggested The patient needs to be evaluated carefully for any unrecognized transit hyper-coagulopathy A preoperative venous study (such as MRV) should be performed in all cases to gain a better understanding of the venous anatomy and to identify veins that might be at risk for injury A microsurgical technique is always preferable, as is minimal use of bipolar coagulation.
Declaration of patient consent
The Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmed SI, Javed G, Laghari AA, Bareeqa SB, Aziz K, Khan M. Third ventricular tumors: A comprehensive literature review. Cureus. 2018. 10: e3417
2. Almubarak AO, Alobaid A, Qoqandi O, Bafaquh M. Minimally invasive brain port approach for accessing deep-seated lesions using simple syringe. World Neurosurg. 2018. 117: 54-61
3. Apuzzo ML. Commentary. Neurosurgery. 1990. 26: 542
4. Apuzzo ML. Surgery of masses affecting the third ventricular chamber: Techniques and strategies. Clin Neurosurg. 1988. 34: 499-522
5. Barbagallo GM, Raudino G, Visocchi M, Maione M, Certo F. Out-of-third ventricle colloid cysts: Review of the literature on pathophysiology, diagnosis and treatment of an uncommon condition, with a focus on headache. J Neurosurg Sci. 2019. 63: 330-6
6. Chan RC, Thompson GB. Third ventricle colloid cysts presenting with acute neurological deterioration. Surg Neurol. 1983. 19: 358-62
7. Dandy WE. Diagnosis, localization and removal of tumours of the third ventricle. Bull Johns Hopkins Hosp. 1922. 33: 188-9
8. Hirsch JF, Zouaoui A, Renier D, Pierre-Kahn A. A new surgical approach to the third ventricle interruption of the striothalamic vein. Acta Neurochir (Wien). 1979. 47: 135-47
9. Sugita K, Kobayashi S, Yokoo A. Preservation of large bridging veins during brain retraction. J Neurosurg. 1982. 57: 856-8
10. Symss NP, Ramamurthi R, Kapu R, Rao SM, Vasudevan MC, Pande A. Complication avoidance in transcallosal transforaminal approach to colloid cysts of the anterior third ventricle: An analysis of 80 cases. Asian J Neurosurg. 2014. 9: 51-7
11. Tenny S, Thorell W, editors. Colloid brain cyst. StatPearls. Treasure Island, FL: StatPearls Publishing; 2021. p. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470314 [Last accessed on 2023 May 27]
12. Wallmann H. A colloid cyst in the third cerebral ventricle and a lipoma in the choroid plexus. Virchows Arch Pathol An at. 1858. 14: 385-8
13. Yadav YR, Parihar V, Pande S, Namdev H. Endoscopic management of colloid cysts. J Neurol Surg A Cent Eur Neurosurg. 2014. 75: 376-80
14. Yadav YR, Yadav N, Parihar V, Kher Y, Ratre S. Management of colloid cyst of third ventricle. Turk Neurosurg. 2015. 25: 362-71