- Department of Neurosurgery, Al-Bashir Governmental Hospital, Amman, Jordan.
- Department of Radiology, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan.
Correspondence Address:
Bashar Abuzayed
Department of Radiology, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan.
DOI:10.25259/SNI_664_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Bashar Abuzayed1, Anas Said1, Osama Jamous1, Omar Al-Ashqar1, Hussein Al-Abadi1, Khalid Alawneh2. Extra-axial cerebellopontine angle cavernoma: A case report and review of literature. 11-Nov-2020;11:386
How to cite this URL: Bashar Abuzayed1, Anas Said1, Osama Jamous1, Omar Al-Ashqar1, Hussein Al-Abadi1, Khalid Alawneh2. Extra-axial cerebellopontine angle cavernoma: A case report and review of literature. 11-Nov-2020;11:386. Available from: https://surgicalneurologyint.com/surgicalint-articles/10387/
Abstract
Background: Extra-axial cavernomas at the cerebellopontine angle (CPA) are rare clinical entity that can radiologically mimic several lesions encountered at this location.
Case Description: A 36-year-old female patient referred to our emergency service with acute decreased level of consciousness and vomiting. Neurological examination showed Glasgow Coma Scale of 12 with downbeat nystagmus of the right eye. Brain computed tomography scan and magnetic resonance imaging showed multilobulated extra-axial mass lesion located in the right CPA. The lesion was with various signal intensities in T1- and T2-weighted images suggestive of hemorrhages of different ages. T2 gradient echo sequences showed multiple sinusoid-like channels and diffuse hemosiderin deposition. These figures were compatible with cavernous malformation. The patient was operated by retrosigmoid approach. Dissection of the mass from the trigeminal, facial, vestibulocochlear, and lower cranial nerves was performed and total resection of the tumor was achieved. Histopathological examination confirmed the diagnosis of cavernoma.
Conclusion: Although CPA cavernomas are very rare, they should be considered for differential diagnosis when evaluating CPA lesions preoperatively for better intraoperative management and postoperative outcomes.
Keywords: Cavernoma, Cavernous hemangioma, Cerebellopontine angle, Extra-axial lesion
INTRODUCTION
Cavernoma, also known as cavernous hemangioma and cavernous angioma, accounts for 10–20% of vascular malformations.[
This paper reports the clinical case of a patient with extra-axial cavernoma of CPA. Clinical, radiologic, and pathologic data are discussed, and literature review of similar cases was performed and summarized.
CASE REPORT
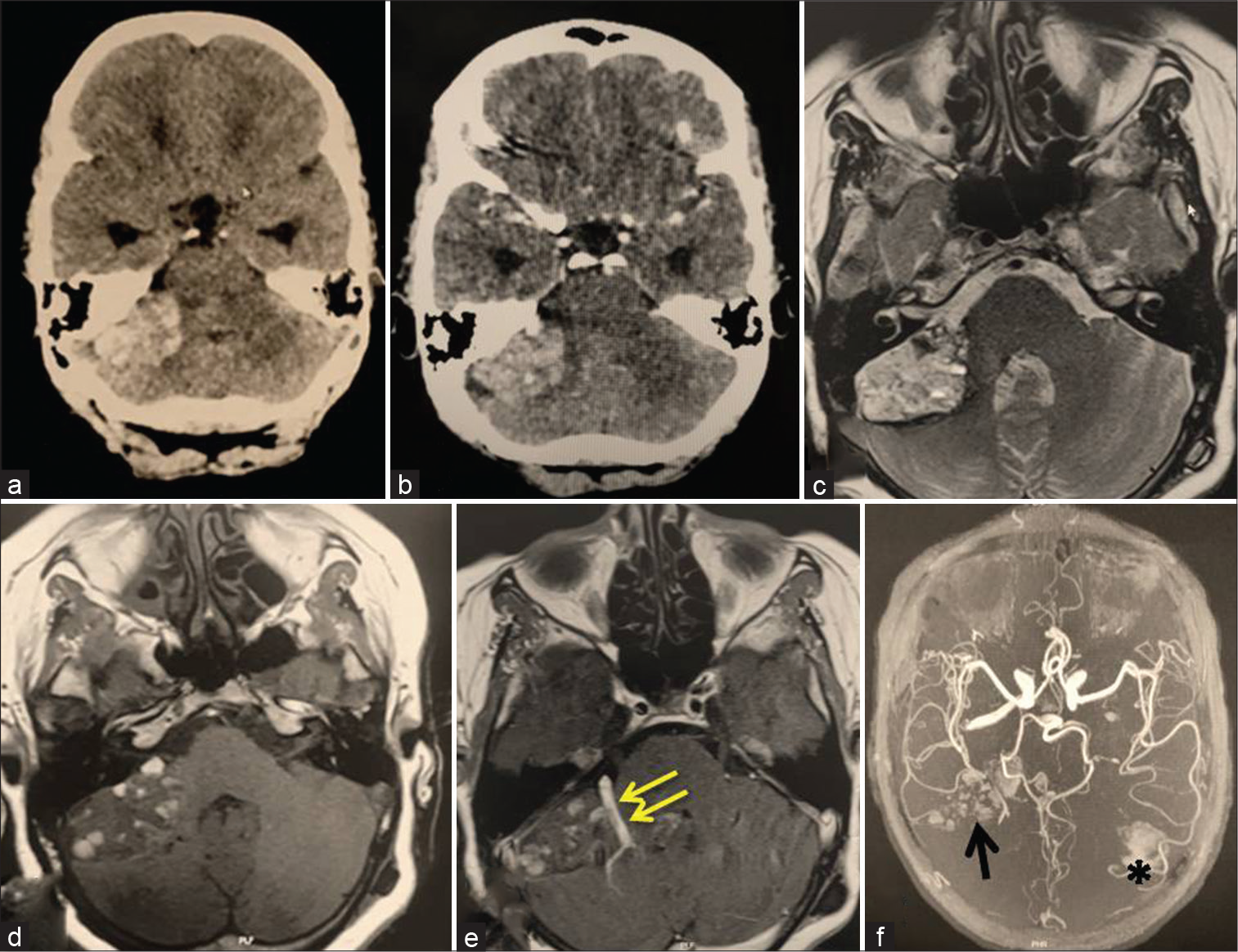
A 36-year-old female patient referred to our emergency service with acute decreased level of consciousness and vomiting. Neurological examination showed Glasgow Coma Scale of 12 with downbeat nystagmus of the right eye. No pupils abnormalities nor motor deficit were documented. Urgent brain computed tomography (CT) scan showed hyperdense lesion of the right CPA, with an associated mass effect compressing the fourth ventricle and secondary acute hydrocephalus [
Figure 1:
Preoperative brain neuroimaging showing an extra-axial vascular mass lesion involving the right cerebellopontine angle (CPA) with associated venous anomaly. (a) Brain computed tomography (CT) scan without contrast, (b) CT scan with contrast, (c) axial T2 weighted, (d) axial T1 weighted without contrast, (e) postcontrast axial T1 weighted, and (f) MR angiography. Double arrow: associated venous anomaly, arrow: sinusoid pools in the site of the lesion in the right CPA, asterisk: small intraparenchymal hematoma in the site of VP shunt insertion.
Figure 2:
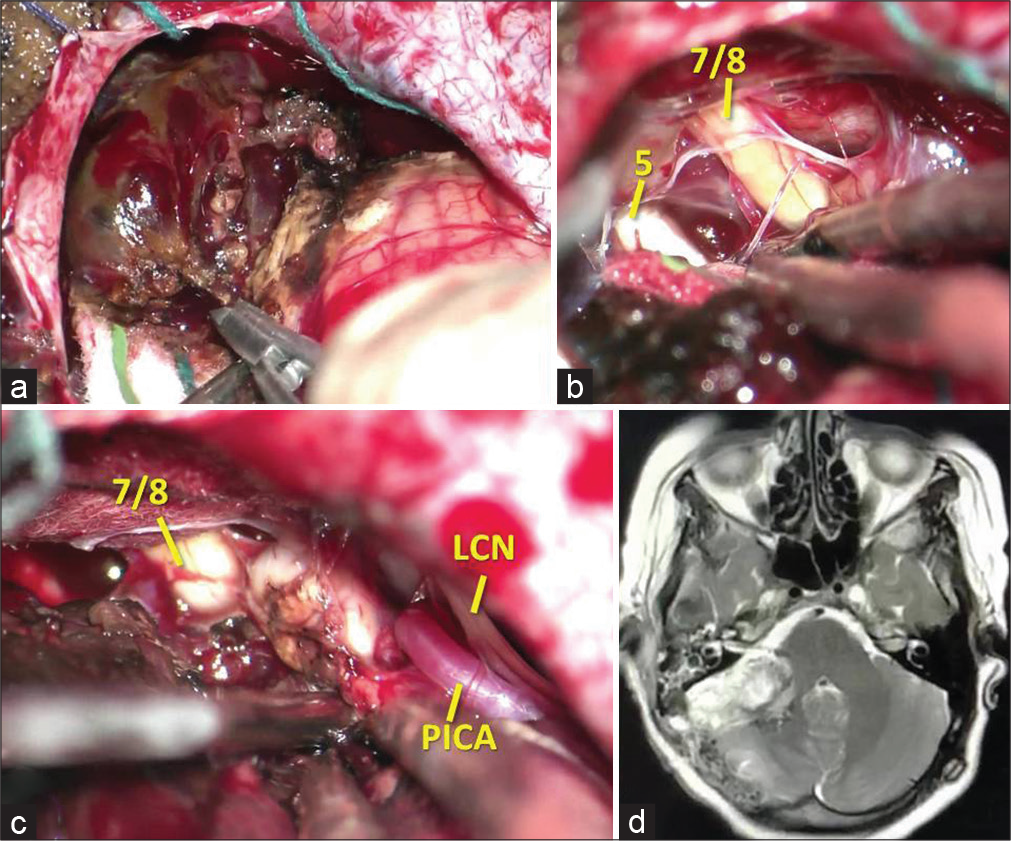
Intraoperative views showing: (a) the gross appearance of the extra-axial lesion in the cerebellopontine angle, (b) dissection of the trigeminal nerve and the facial/vestibule-cochlear complex, (c) dissection of the lower cranial nerves and posterior inferior cerebellar artery. (d) Early postoperative brain magnetic resonance imaging showing total resection of the lesion. 5: Trigeminal nerve, 7/8: Facial/vestibulocochlear complex, LCN: Lower cranial nerves, PICA: Posterior inferior cerebellar artery
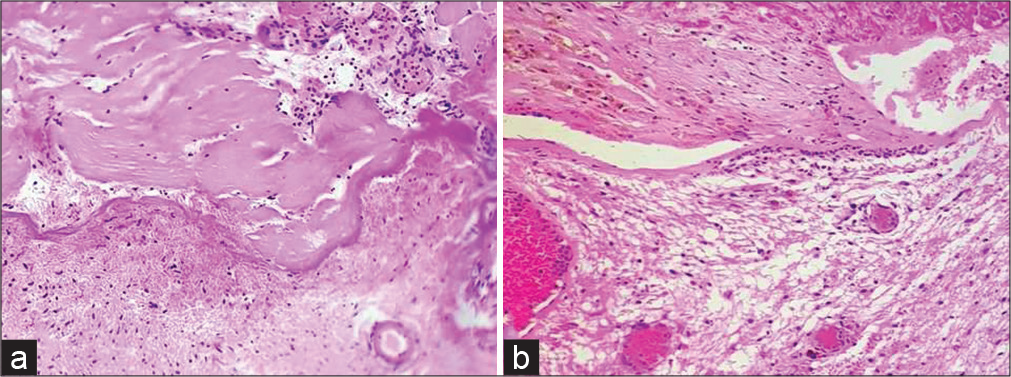
Histopathological examination revealed a lobular arrangement of dilated and congested vascular spaces lined by a single layer of endothelial cells. Intervening stroma was fibrocollagenous and devoid of nervous tissue, compatible with the diagnosis of a cavernoma [
Methods
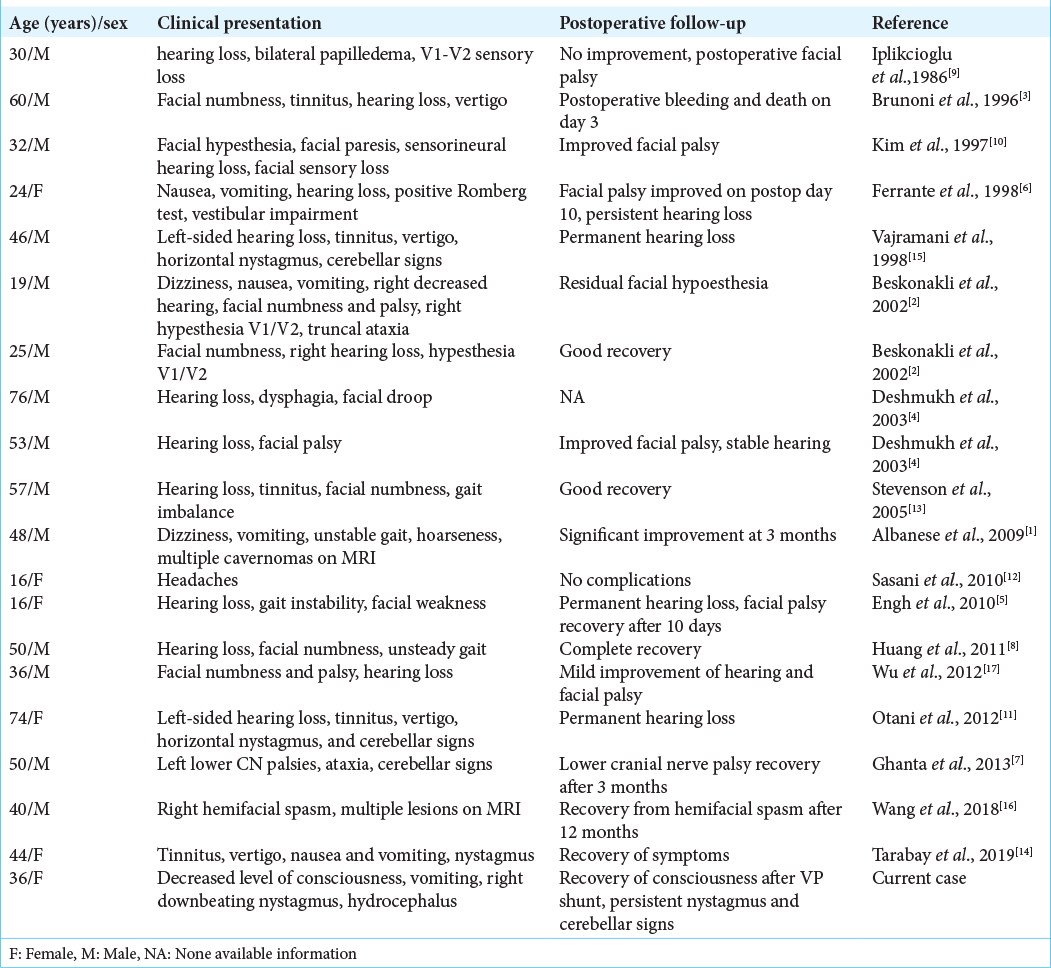
The authors performed a review of the English literature considering extra-axial CPA cavernomas published in PubMed, reported up to June 2020. Searching key words included “cavernoma,” “cavernous malformation,” “cavernous hemangioma,” “cavernous angioma,” and “cerebellopontine angle.” Case of intra-axial cavernomas of the cranial nerves in the CPA was identified and excluded. The results of the search showed a total of 19 cases of extra-axial CPA cavernoma. These cases, in addition of our case, are summarized in [
RESULTS
In the review, there were 14 males (70 %) and 6 females (30 %) (ratio M:F = 2.3:1). The age of presentation ranged between 16 and 76 years (mean = 41.6 ± 6 years), with mean age of 44.4 years for males and 35 years for females. The most common presenting symptom was vestibulocochlear which was seen in 16 patients (80%), followed by cerebellar in 10 patients (50%), trigeminal in 8 patients (40%), facial in 7 patients (35%), and lower cranial nerves’ palsy in 3 patients (15%). There was a variable overlap and combination of the symptoms and signs in the patients.
All cases documented their CT scan findings reported iso- to hyperdense lesions with variable calcifications and enhancement. On MRI, most cases showed typical multilobulated reticular core like that of intra-axial cavernomas (70%) and presented a hypointense surrounding rim on T2 or T2 gradient and hyperintense on T1. Eleven cases (55%) showed postcontrast enhancement, most of them enhanced heterogeneously. The majority of cases were sporadic, except two cases reported by Albanese et al.[
The surgical approach for these lesions in all cases was the retrosigmoid approach. Intraoperatively, all lesions were hemorrhagic with xanthochromic fluid-filled cavities, and they appeared as red-purple-gray-bluish lesions, adherent to the brainstem, adherent or encasing the trigeminal, VII-VIII complex, or lower cranial nerves. Outcome after surgery was documented in 19 cases. Thirteen cases showed postoperative improvement of the neurologic symptoms/signs; four cases were stable without significant change; one case presented a worsening of facial paresis; and one patient died from massive bleeding at day 3 postoperatively.
Histologically, all cases showed typical pattern of lobular arrangement of dilated and congested vascular spaces lined by a single layer of endothelial cells. Intervening stroma was fibrocollagenous and devoid of nervous tissue.
DISCUSSION
Cavernomas are considered as cerebral angiographically occult vascular malformations. They consist of dilated vascular sinusoid channels lined by endothelium, without an associated media or adventitia and without intervening brain parenchyma, with the absence of associated feeding arteries or draining veins.[
They are benign and slow-growing lesions. Recurrent hemorrhage from the sinusoids of the vascular malformation or from the neocapillary of the cyst wall and the osmotic transport of water into the cyst are thought to induce the growth of the cyst.[
According to Deshmukh et al.,[
Histologically extra- and intra-axial cavernomas share the same pattern of lobular arrangement of dilated and congested vascular spaces lined by a single layer of endothelial cells, with fibrocollagenous intervening stroma devoid of nervous tissue. Extra-axial cavernomas typically arise from the dural surfaces or cranial nerves. Therefore, the clinical presentation is more likely to be that of cranial nerve involvement, especially the vestibulocochlear nerve (80%).
The surgical approach for these lesions in all cases was the retrosigmoid approach. This approach is proper for wide field exposure with sufficient visualization of the three CPA complexes. Intraoperatively, these lesions were described as hemorrhagic, which can cause massive bleeding.[
For CPA cavernomas, lesion debulking (with suction, curetting, or ultrasonic aspiration) must be avoided to prevent entering the vascular sinusoids. Emptying the cystic part, coagulation of the capsule, shrinking of the cavernoma, and an “en bloc” resection as far as possible with careful dissection of the cranial nerves are the main steps for resection of CPA cavernomas.[
Outcome after surgery was documented in 19 cases. Thirteen cases showed postoperative improvement of the neurologic symptoms/signs; four cases were stable without significant change; one case presented a worsening of facial paresis; and one patient died from massive bleeding at day 3 postoperatively. As an important finding of the outcome review, patients with preoperative hearing impairment remained permanent, whereas all patients (except one patient) with facial palsy had significant improvement.
CONCLUSION
Cavernomas are benign lesions and usually have a good prognosis after total resection. Although very rare, cavernomas should be considered for differential diagnosis when evaluating CPA lesions preoperatively for better intraoperative management and postoperative outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Albanese A, Sturiale CL, D’Alessandris QG, Capone G, Maira G. Calcified extra-axial cavernoma involving lower cranial nerves: Technical case report. Neurosurgery. 2009. 64: E135-6
2. Beskonakli E, Kaptanoglu E, Okutan O, Solaroglu I, Taskin Y. Extra-axial cavernomas of the cerebellopontine angle involving the seventh-eighth nerve complex. Neurosurg Rev. 2002. 25: 222-4
3. Brunoni A, Chiappetta F. Cystic extra-axial cavernoma of the cerebellopontine angle. Surg Neurol. 1996. 46: 475-6
4. Deshmukh VR, Albuquerque FC, Zabramski JM, Spetzler RF. Surgical management of cavernous malformations involving the cranial nerves. Neurosurgery. 2003. 53: 352-7
5. Engh JA, Kostov D, St Martin MB, Yeaney G, Rothfus W, Hirsch B. Cavernous malformation tumors: A case study and review of the literature. Otol Neurotol. 2010. 31: 294-8
6. Ferrante L, Acqui M, Trillò G, Antonio M, Nardacci B, Celli P. Cavernous angioma of the 8th cranial nerve. A case report. Neurosurg Rev. 1998. 21: 270-6
7. Ghanta RK, Tangella P, Koti K, Dandamudi S. A rare case of an extra-axial cavernous angioma in the cerebellopontine angle. J Neurosci Rural Pract. 2013. 4: 210-2
8. Huang H, Xu K, Qu L, Li Y, Yu J. Cystic cavernous malformation of the cerebellopontine angle: Case report and literature review. World J Surg Oncol. 2011. 9: 36
9. Iplikcioglu AC, Benli K, Bertan V, Ruacan S. Cystic cavernous hemangioma of the cerebellopontine angle: Case report. Neurosurgery. 1986. 19: 641-2
10. Kim M, Rowed DW, Cheung G, Ang LC. Cavernous malformation presenting as an extra-axial cerebellopontine angle mass: Case report. Neurosurgery. 1997. 40: 187-90
11. Otani N, Wada K, Sakakibara F, Takeuchi S, Nagatani K. A cystic haemorrhagic lesion located in the cerebellopontine angle cistern. Cavernous angioma. J Clin Neurosci. 2012. 19: 1551-1608
12. Sasani M, Bayhan M, Cakiroglu G, Ozer A. Extra axial cavernous hemangioma of the cerebellopontine angle with intratumor hemorrhage: Case report and review. Neurosurg Q. 2010. 20: 23-6
13. Stevenson CB, Johnson MD, Thompson RC. Cystic cavernous malformation of the cerebellopontine angle, Case illustration. J Neurosurg. 2005. 103: 931
14. Tarabay A, Rocca A, Maeder P, Simonin A, Messerer M, Daniel RT. Extra-axial cavernoma of the cerebellopontine angle: A case study and review of literature. World Neurosurg. 2019. 128: 415-21
15. Vajramani GV, Devi I, Hegde T, Srikanth SG, Shankar SK. Cystic cavernous malformation of the cerebellopontine angle. Clin Neurol Neurosurg. 1998. 100: 133-7
16. Wang L, Jiang M, Yin H, Huang M, Zhu L, Liang X. Cavernous angioma of the cerebellopontine angle presenting as hemifacial spasm. Neurol India. 2018. 66: 1826-8
17. Wu B, Liu W, Zhao Y. Coexistence of extra-axial cavernous malformation and cerebellar developmental venous anomaly in the cerebellopontine angle. World Neurosurg. 2012. 78: 375.e5-9