- Department of Neurosurgery, University of Baghdad, College of Medicine, Baghdad, Iraq,
- Department of Biology, University of Al-Mustansiriyah, College of Sciences, Baghdad, Iraq,
- Department of Neurosurgery, Azerbaijan Medical University, Baku, Azerbaijan, Iraq,
- Department of Neurosurgery, Neurosurgical Teaching Hospital, Baghdad, Iraq,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
DOI:10.25259/SNI_937_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mustafa Ismail1, Teeba A. Al-Ageely1, Mohamed Almustafa A. Alzerkani1, Younus M. Al-Khazaali1, Haneen A. Salih2, Aktham O. Al-Khafaji1, Zahraa M. Kareem1, Alkawthar M. Abdulsada3, Hayder R. Salih4, Samer S. Hoz5. Extracranial carotid localized fibromuscular dysplasia: A case report and literature review. 28-Oct-2022;13:498
How to cite this URL: Mustafa Ismail1, Teeba A. Al-Ageely1, Mohamed Almustafa A. Alzerkani1, Younus M. Al-Khazaali1, Haneen A. Salih2, Aktham O. Al-Khafaji1, Zahraa M. Kareem1, Alkawthar M. Abdulsada3, Hayder R. Salih4, Samer S. Hoz5. Extracranial carotid localized fibromuscular dysplasia: A case report and literature review. 28-Oct-2022;13:498. Available from: https://surgicalneurologyint.com/surgicalint-articles/11956/
Abstract
Background: Fibromuscular dysplasia (FMD) is a noninflammatory and nonatherosclerotic arteriopathy that is characterized by irregular cellular proliferation and deformed construction of the arterial wall that causes segmentation, constriction, or aneurysm in the intermediate-sized arteries. The incidence of FMD is 0.42–3.4%, and the unilateral occurrence is even rarer. Herein, we report a rare case of a localized extracranial carotid unilateral FMD associated with recurrent transient ischemic attacks (TIAs) treated by extracranial-intracranial bypass for indirect revascularization. The specific localization of the disease rendered our case unique.
Methods: We conducted a review of the PubMed Medline database search using the following combined formula: ((FMD [Title/Abstract]) AND ((isolated [Title/Abstract]) OR (localized [Title/Abstract]))) AND Internal carotid artery (ICA) (Title/Abstract). Additional resources were included by screening the reference list of the selected papers.
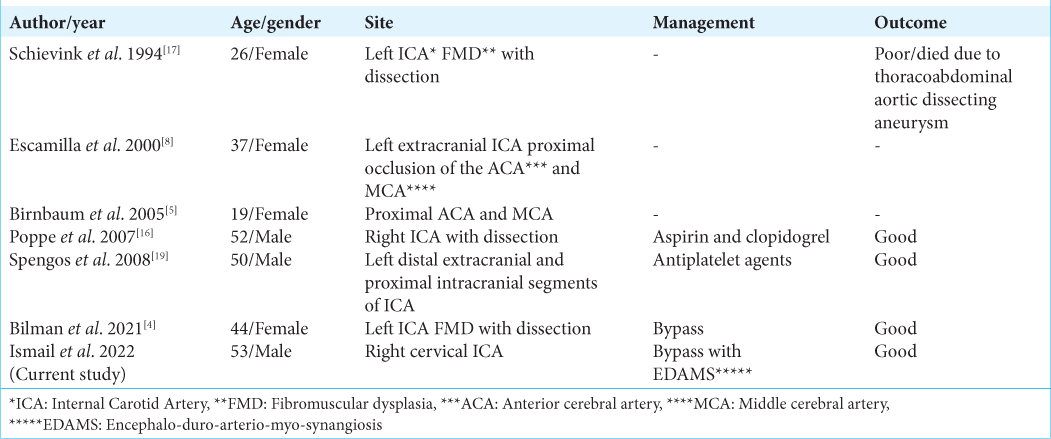
Results: A total of six cases were found, and all accounted for localized FMD affecting the ICA. The age range was between 19 and 52, the male-to-female ratio was (2:4), and all of the cases consisted of unilateral carotid FMD, mainly on the left side with a left-to-right ratio of 5:1. The management and outcome of these cases varied according to the case and associated complications.
Conclusion: Extracranial localized FMD of the ICA is a rare subtype of FMD that has little documentation in the literature. In our case, it was a localized extracranial carotid unilateral FMD associated with recurrent TIAs. The appropriate treatment was using the intracranial-extracranial bypass.
Keywords: Encephalo-duro-arterio-myo-synangiosis, Extracranial – intracranial bypass, Fibromuscular dysplasia
INTRODUCTION
Fibromuscular dysplasia (FMD) is a noninflammatory and nonatherosclerotic arteriopathy that is identified by irregular cellular reproduction and deformed construction of the arterial wall, causing segmentation and constriction (with either central stenosis or the more common beads figure), or aneurysm of intermediate-sized arteries.[
The incidence of FMD is approximately (0.42–3.4%) and its unilateral occurrence is even rarer.[
Most patients with FMD are asymptomatic, and the lesion is discovered incidentally. Some patients have a myriad of symptoms, including headaches, transient ischemic attacks (TIAs), and even stroke.[
In this paper, the authors report a case of a 53-year-old male with focal extracranial carotid unilateral FMD associated with recurrent TIAs. The uncommon localization of the stenosis made the approach seemingly suitable for this case.
CASE DESCRIPTION
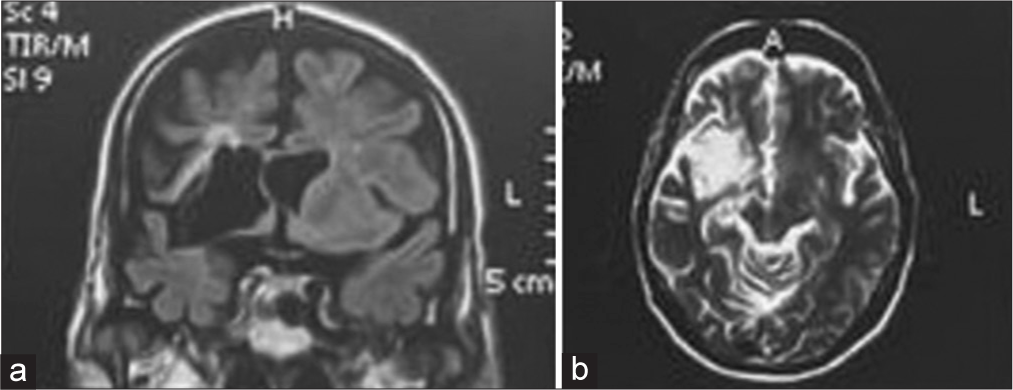
A 53-year-old male was referred to Neurosurgical Teaching Hospital in Baghdad, Iraq, with a history of recurrent TIAs with the left upper limb weakness grade 3/5. Magnetic resonance imaging [
Figure 1:
(a) Preoperative T1-weighted magnetic resonance imaging (MRI) image (coronal view) showing periventricular old ischemia alongside cerebospinal fuild (CSF)-filled cleft in the right-sided hemisphere. (b) Preoperative T2-weighted MRI image (axial view) revealing periventricular longstanding ischemic changes and unilateral CSF-filled cleft in the right hemisphere extending from the frontal horn of the lateral ventricle to the Sylvian fissure.
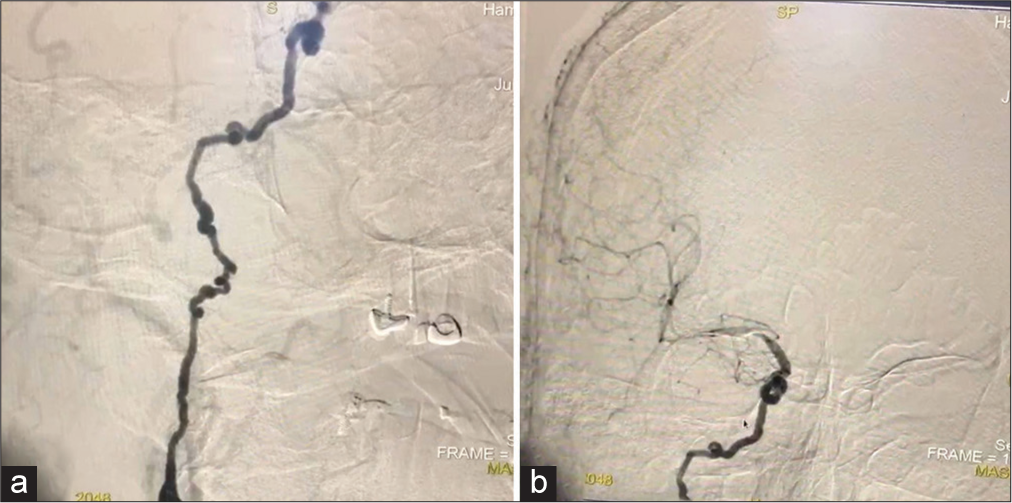
Figure 2:
(a) Preoperative digital subtraction angiography demonstrating fibromuscular dysplasia-related multifocal stenosis along the right extracranial internal carotid artery (ICA). (b) Preoperative digital subtraction angiography demonstrating the “beads-on-a-string” sign appearance along the right extracranial ICA.
The patient underwent encephalo-duro-arterio-myosynangiosis (EDAMS) surgery under intraoperative neurophysiological monitoring, including somatosensory evoked potentials and motor evoked potentials. Postoperatively, the patient was conscious with stable vital signs and left-sided weakness grade 3/5, which is the same as preoperatively. A postoperative CT scan revealed no signs of new ischemia or stroke, and the patient was discharged after 5 days. Six months of follow-up revealed left-sided weakness Grade 4 with no new findings on imaging.
MATERIALS AND METHODS
We conducted a PubMed Medline database search using the following combined formula: ((FMD [Title/Abstract]) AND ((isolated [Title/Abstract]) OR (localized [Title/ Abstract]))) AND ICA [Title/Abstract]. Additional resources were obtained by screening the reference list of the selected articles.
RESULTS
A total of 16 results were found, eight of them were case reports, and only six of them accounted for localized FMD affecting the ICA. According to the reported cases, the age range was between 19 and 52, the male-to-female ratio was 2:4, and all of the cases consisted of unilateral carotid FMD, with the majority on the left side with a left-to-right ratio of (5:1). The management and outcome of these cases differed according to the case [
DISCUSSION
FMD is a rare nonatherosclerotic and noninflammatory vasculopathy resulting in arterial narrowing and the potential formation of small- and medium-sized vessel aneurysms.[
Extracranial localized FMD cases also have few reports in the literature.[
Because many patients are asymptomatic, it can be found incidentally on imaging or physical examination while investigating for any cervical bruit.[
Management of FMD depends mainly on the clinical manifestations and the pertinent anatomy of the artery involved. Conservative management of asymptomatic carotid artery FMD is advised, with monitoring and anticoagulant therapy. When FMD results in the occlusion of the artery by thrombus formation, dual antiplatelet therapy is used along with anticoagulant medications to prevent ischemic injury. Revascularization with a bypass is an option for a good outcome with fine patency of blood flow intracerebrally.[
Interventional management is usually indicated in patients with symptomatic extracranial carotid FMD. This includes surgical dilatation with or without endarterectomy for the carotid arteries. The most commonly used option is percutaneous transluminal balloon angioplasty with or without the application of stents or cerebral protection devices.[
In the present case, the localized peculiarity of the stenosis is similar in concept to Moyamoya disease (MMD), another vasculopathy characterized by progressive bilateral stenosis, and occlusion of the supraclinoid ICA leading to the development of collateral vessels. Diverse surgical techniques have been performed to manage MMD to avoid ischemic injury and such techniques may be employed in managing localized FMD of the ICA. The most commonly used methods include direct revascularization by superficial temporal artery to MCA bypass and indirect revascularization methods such as encephalo-myo-synangiosis, encephalo-duro-arteriosynangiosis, and EDAMS.[
We reviewed the literature for the reported cases of localized FMD involving the ICA. Only six cases consisted of localized carotid artery FMD; almost all of these cases involved the left-sided ICA. Treatment choices are individualized to each case, and with the evolving capabilities of endovascular procedures, outcomes for symptomatic FMD may vary significantly.
In the present case, the patient had localized FMD of the right extracranial ICA. The uncommon localization of the stenosis with the coexistence of low-flow MCA made the approach seemingly suitable for this case. Indirect revascularization by EDAMS was performed to prevent further ischemic attacks. Management of FMD varies due to the clinical manifestations observed. The surgeon’s decision for the operative intervention method differs according to the case. Suggestions for managing localized arterial stenosis in FMD of the extracranial ICA are minimal and rarely reported.
CONCLUSION
The scarce nature of craniocerebral FMD poses particular diagnostic and therapeutic challenges. Traditional surgical and endovascular management options exist, but individualized planning is essential with each case, especially with ICA occlusion or weak flow. In our case, the localized stenosis of the extracranial ICA is a rare subtype of FMD, rendering our case unique since isolated FMD involving the ICA has only a few documents in the literature.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al-Nouri O, Pan J, Mannava K. Endovascular treatment of concomitant carotid fibromuscular dysplasia and atherosclerotic disease after failed open surgical treatment. Vasc Endovasc Surg. 2019. 53: 250-4
2. Bartels E, Bartels S, Poppert H. Diagnosis of nonatherosclerotic carotid disease. Perspect Med. 2012. 1: 244-9
3. Begelman SM, Olin JW. Fibromuscular dysplasia. Curr Opin Rheumatol. 2000. 12: 41-7
4. Bilman V, Apruzzi L, Baccellieri D, Sanvito F, Bertoglio L, Chiesa R. Symptomatic internal carotid artery dissection and kinking in a patient with fibromuscular dysplasia. J Vasc Bras. 2021. 20: e20200243
5. Birnbaum LA, Sherry R, Pereira E. Isolated intracranial fibromuscular dysplasia presents as stroke in a 19-year-old female. Arq Neuropsiquiatr. 2005. 63: 318-20
6. Brinza EK, Gornik HL. Fibromuscular dysplasia: Advances in understanding and management. Cleve Clin J Med. 2016. 83: S45-51
7. Cardounell SZ, Gonzalez L, editors. Carotid Artery Fibromuscular Dysplasia. Treasure Island, FL: StatPearls; 2021. p.
8. Escamilla F, Espigares A, Hervas R, Fernandez MD, Vela R, Garcia T. Fibromuscular dysplasia with moyamoya phenomenon in a patient with Alport’s syndrome. A Type IV collagen disorder. Rev Neurol. 2000. 30: 736-40
9. Isono M, Ishii K, Kamida T, Inoue R, Fujiki M, Kobayashi H. Long-term outcomes of pediatric moyamoya disease treated by encephalo-duro-arterio-synangiosis. Pediatr Neurosurg. 2002. 36: 14-21
10. Leary MC, Finley A, Caplan LR. Cerebrovascular complications of fibromuscular dysplasia. Curr Treat Options Cardiovasc Med. 2004. 6: 237-48
11. Lopez-Gonzalez MA, Zhao X, Ramanathan D, Eastin TM, Minwoo S. High flow bypass for right giant cavernous internal carotid artery aneurysm with fibromuscular dysplasia of cervical internal carotid artery: Microsurgical 2-D video. Surg Neurol Int. 2020. 11: 177
12. Maramattom BV, Thomas J, Panicker D, Gopalakrishnan CV. Extensive fibromuscular dysplasia in a young girl treated with bilateral STA-MCA bypass. Neurol India. 2022. 70: 792-3
13. McDonald A. A case of isolated intracranial fibromuscular dysplasia. Cureus. 2020. 12: e8755
14. Olin JW, Pierce M. Contemporary management of fibromuscular dysplasia. Curr Opin Cardiol. 2008. 23: 527-36
15. Plouin PF, Perdu J, La Batide-Alanore A, Boutouyrie P, Gimenez-Roqueplo AP, Jeunemaitre X. Fibromuscular dysplasia. Orphanet J Rare Dis. 2007. 2: 28
16. Poppe AY, Minuk J, Glikstein R, Leventhal M. Fibromuscular dysplasia with carotid artery dissection presenting as an isolated hemianopsia. J Stroke Cerebrovasc Dis. 2007. 16: 130-4
17. Schievink WI, Björnsson J, Piepgras DG. Coexistence of fibromuscular dysplasia and cystic medial necrosis in a patient with Marfan’s syndrome and bilateral carotid artery dissections. Stroke. 1994. 25: 2492-6
18. Sharma AM, Kline B. The United States registry for fibromuscular dysplasia: New findings and breaking myths. Tech Vasc Interv Radiol. 2014. 17: 258-63
19. Spengos K, Vassilopoulou S, Tsivgoulis G, Papadopoulou M, Vassilopoulos D. An uncommon variant of fibromuscular dysplasia. J Neuroimaging. 2008. 18: 90-2
20. Stanley JC, Gewertz BL, Bove EL, Sottiurai V, Fry WJ. Arterial fibrodysplasia: Histopathologic character and current etiologic concepts. Arch Surg. 1975. 110: 561-6
21. Stewart MT, Moritz MW, Smith RB, Fulenwider JT, Perdue GD. The natural history of carotid fibromuscular dysplasia. J Vasc Surg. 1986. 3: 305-10
22. Subramanian A, Aggarwal G, Agarwal D, Lalwani S. Internal carotid artery fibromuscular dysplasia in a child: Incidental postmortem finding after head injury. J Lab Physicians. 2017. 9: 60-3
23. Takenaka K, Shimizu K, Ando T, Sakai N, Yamada H. Fibromuscular dysplasia with cerebral infarction in children case report. Neurol Med Chir (Tokyo). 1989. 29: 912-6
24. Touzé E, Oppenheim C, Trystram D, Nokam G, Pasquini M, Alamowitch S. Fibromuscular dysplasia of cervical and intracranial arteries. Int J Stroke. 2010. 5: 296-305