- Department of Neurosurgery Research and Innovation, NHO Osaka National Hospital, Osaka, Japan
- Department of Biomedical Research and Innovation, NHO Osaka National Hospital, Osaka, Japan
- Department of Neurosurgery, Osaka University Graduate School of Medicine, Suita, Japan.
Correspondence Address:
Nobuyuki Izutsu, Department of Neurosurgery, NHO Osaka National Hospital, Osaka, Japan.
DOI:10.25259/SNI_57_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nobuyuki Izutsu1, Naoki Nishizawa1, Shin Nakajima1, Yonehiro Kanemura1,2, Tomohiko Ozaki3, Katsunori Asai1, Tomoki Kidani1, Koji Kobayashi1, Yosuke Fujimi1, Toshiyuki Fujinaka1. Extracranial internal carotid artery-dissecting aneurysm having a re-entry tear and causing lower cranial nerve palsies treated with flow-diverting stent: A case report. 12-Apr-2024;15:126
How to cite this URL: Nobuyuki Izutsu1, Naoki Nishizawa1, Shin Nakajima1, Yonehiro Kanemura1,2, Tomohiko Ozaki3, Katsunori Asai1, Tomoki Kidani1, Koji Kobayashi1, Yosuke Fujimi1, Toshiyuki Fujinaka1. Extracranial internal carotid artery-dissecting aneurysm having a re-entry tear and causing lower cranial nerve palsies treated with flow-diverting stent: A case report. 12-Apr-2024;15:126. Available from: https://surgicalneurologyint.com/surgicalint-articles/12856/
Abstract
Background: Extracranial internal carotid artery (ICA)-dissecting aneurysms (DAs) rarely cause re-entry tears and lower cranial nerve palsies. The therapeutic strategies for these pathologies are not well established. This report presents a case of an extracranial ICA -DA with a re-entry tear that caused lower cranial nerve palsy.
Case Description: A 60-year-old man presented with left neck pain, hoarseness, and dysphagia. Physical examination and laryngoscopy determined palsies of the left cranial nerves IX, X, and XII. Digital subtraction angiography (DSA) revealed a DA in the left extracranial ICA, and three-dimensional DSA showed entry and re-entry tears in the intimal flap. Flow-diverting stents (FDSs) were placed on the lesion that covered the entry and re-entry tears because the symptoms did not improve after five weeks of conservative treatment. A post-procedural angiogram indicated flow stagnation in the DA. Symptoms improved remarkably immediately after the procedure, and the aneurysm was almost completely occluded six months later.
Conclusion: Herein, an extracranial ICA -DA with a re-entry tear that caused lower cranial nerve palsy did not improve after five weeks of conservative treatment. FDS placement promptly resolved the aneurysm and symptoms. Thus, FDS placement may be an effective treatment option for extracranial ICA-DAs with re-entry tears or lower cranial nerve palsies.
Keywords: Dissecting aneurysm, Elongated styloid process, Extracranial internal carotid artery, Flow-diverting stent, Lower cranial nerve palsy
INTRODUCTION
Extracranial internal carotid artery (ICA) dissection often results in true lumen stenosis with an intramural hematoma. Contrastingly, extracranial ICA dissection occasionally forms a dissecting aneurysm (DA),[
CASE DESCRIPTION
A 60-year-old man presented with sudden onset of left neck pain after rotating his head to the right, followed by hoarseness and dysphagia. The patient had no significant history of other diseases. The physical examination determined the poor elevation of the left soft palate and leftward deviation of the tongue on protrusion. Laryngoscopy revealed left-sided vocal cord paralysis. Magnetic resonance imaging and magnetic resonance angiography showed dilatation of the left ICA, and diffusion-weighted imaging indicated no cerebral ischemic lesions. Digital subtraction angiography (DSA) revealed a DA in the left distal cervical ICA extending into the petrous portion [
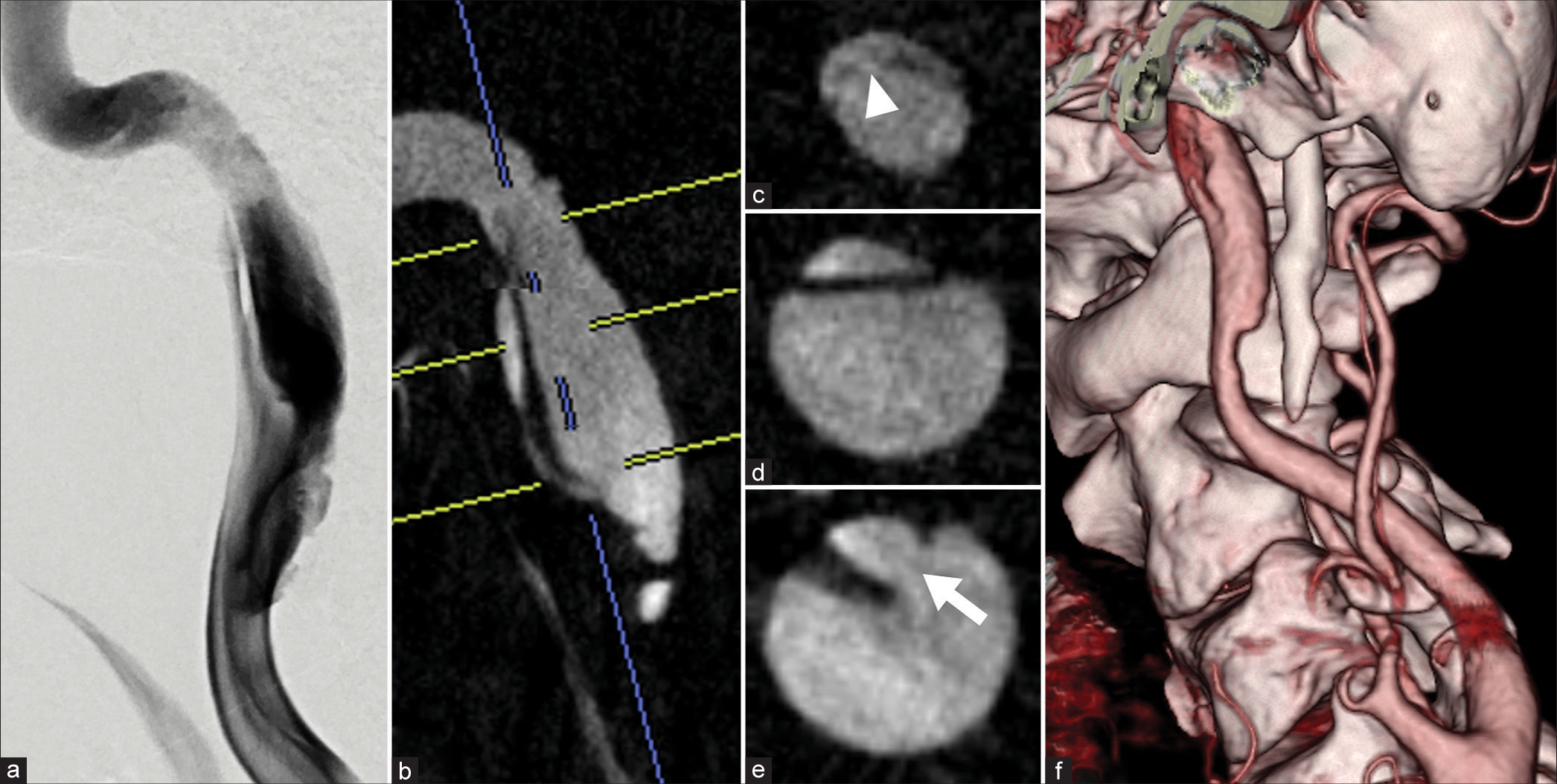
Figure 1:
(a) Digital subtraction angiogram demonstrating the left extracranial internal carotid artery-dissecting aneurysm. (b-e) Three-dimensional digital subtraction angiograms indicate an intimal flap and narrowing of the true lumen. (c) Axial images indicate a re-entry tear (arrowhead) in the upper line level, (d) an intimal flap in the middle line level, (e) and an entry tear (arrow) in the lower line level. (f) Computed tomographic angiogram demonstrating an elongated left styloid process near the dissecting aneurysm.
The diagnosis was left cranial nerve IX, X, and XII palsies caused by compression from the DA, which was further caused by the elongated styloid process. Expecting spontaneous recovery of ICA dissection, we initiated conservative treatment. Anticoagulant therapy with heparin was started to prevent artery-to-artery embolism due to a thrombus within the false lumen. One week later, however, we changed the antithrombotic therapy to dual antiplatelet therapy with acetylsalicylic acid (100 mg/d) and clopidogrel (75 mg/d) in preparation for an emergency stent placement for ICA occlusion due to false lumen thrombosis. During the four weeks of conservative treatment, the patient developed aspiration pneumonia due to severe dysphagia and was required to stop oral intake and start tube feeding. Surgical treatment was planned as the patient’s symptoms did not improve, and the DSA exhibited no changes in the aneurysm. We chose flow-diverting stent (FDS) placement, expecting a reduction in the DA size and preservation of ICA blood flow. FDS placement was performed five weeks after onset.
The procedure was performed under general anesthesia and systemic heparinization. After the placement of an 8-Fr sheath introducer in the right common femoral artery, an 8-Fr guiding catheter was delivered proximal to the lesion in the left ICA. Using a coaxial system with a micro-guidewire, an inner-catheter and a 5-Fr catheter (AXS Catalyst 5 115 cm, Stryker Neurovascular, Fremont, CA, USA), was delivered distal to the lesion through the true lumen. In this procedure, the 5-Fr catheter occluded the true lumen, and antegrade blood flow through the false lumen was clearly observed. The lesion length was 37 mm, and the diameters were 4.9 mm in the distal ICA and 5.4 mm in the proximal ICA. We selected Surpass Streamline 5.0 mm × 50 mm (Stryker Neurovascular, Fremont, CA, USA) as the FDS and placed it in the true lumen from the petrosal portion to the cervical portion of the ICA to cover the entry and re-entry tears. Two telescoping surpass-streamline FDSs were placed due to stent shortening due to dilatation on the lesion. After FDS deployment, balloon angioplasty was performed over the entire length of the FDS. A post-FDS placement DSA demonstrated blood flow stagnation in the DA and true lumen dilation [
Figure 2:
(a) Digital subtraction angiogram (DSA) immediately after stent placement exhibiting blood flow stagnation in the dissecting aneurysm. (b) DSA after 7 d exhibiting regression of the dissecting aneurysm. (c) Three-dimensional DSA after 7 d indicates the remaining thrombosis in the dissecting aneurysm (arrowhead). (d) DSA after six months exhibiting almost complete occlusion of the dissecting aneurysm. (e) Three-dimensional DSA after six months indicating thrombosis regression in the dissecting aneurysm. (f) Reconstructed image from three-dimensional DSA after six months indicating the positional relationship between the flow-diverting stent and the styloid process.
Cranial nerve palsy improved remarkably immediately after FDS placement. The DSA performed 7 d after FDS placement exhibited regression and thrombosis of the DA [
DISCUSSION
We described a case of extracranial ICA-DA with a re-entry tear and high blood flow through the false lumen, which caused cranial nerve IX, X, and XII palsies. The DA and symptoms associated with the lower cranial nerve palsies were promptly resolved with FDS placement.
Extracranial ICA dissection forms DA at an incidence of 13.9%,[
Surgical and endovascular treatment options available for ICA-DA include surgical or internal trapping with or without blood flow reconstruction, such as external carotid artery-radial artery graft-middle cerebral artery bypass and superficial temporal artery-middle cerebral artery bypass, resection with artificial vessel grafting, coil embolization of the DA with or without stents, and stent placement alone using a conventional carotid artery stent or FDS. Recently, stent placement for ICA-DA has been reported to be less invasive and highly effective. Satisfactory angiographic and clinical results have been reported in patients with ICA-DAs treated with FDS.[
Cranial nerve palsy is present in 12% of adult patients with spontaneous extracranial ICA dissection, and 5.2% of patients have lower cranial nerve palsies.[
ICA dissection caused by an elongated styloid process has been reported as vascular Eagle’s syndrome. Elongated styloid processes are defined as those longer than 30 mm that compress the cervical nerves or arteries. Some cases of ICA dissection with an elongated styloid process that was treated by stent placement have been described.[
Although case reports of FDS placement for extracranial ICA-DA having a re-entry tear or causing cranial nerve palsy are limited, the patients were successfully treated, and FDS placement is, therefore, a promising treatment option. Further investigations are necessary to increase our understanding of the treatment strategies for patients with these pathological conditions.
CONCLUSION
Herein, FDS placement promptly resolved the extracranial ICA-DA with a re-entry tear and causing lower cranial nerve palsies when five weeks of conservative treatment had not improved the DA and symptoms. Spontaneous resolution of the DA with a re-entry tear and high blood flow through the false lumen may be rare. In addition, early decompression of the affected cranial nerves may lead to early improvement of the symptoms. FDS placement may, therefore, be an effective treatment option for extracranial ICA-DAs with re-entry tears or causing lower cranial nerve palsy. Furthermore, early FD stent placement may be better than conservative treatment in patients with these pathological conditions.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akamatsu Y, Sato K, Endo H, Matsumoto Y, Tominaga T. Ruptured vertebral artery dissecting aneurysm concurrent with spontaneous cervical internal carotid artery dissection: A report of three cases and literature review. World Neurosurg. 2017. 107: 1048.e1-6
2. Baptista-Sincos AP, Simplício AB, Sincos IR, Leaderman A, Neto FS, MorAuthor A. Flow-diverting stent in the treatment of cervical carotid dissection and pseudoaneurysm: Review of literature and case report. Ann Vasc Surg. 2018. 46: 372-9
3. Beaty N, Patel M, Martinez C, Hollis L. Use of flow diverter stent for treatment of a cervical carotid artery dissection and pseudoaneurysm causing Horner’s syndrome. BMJ Case Rep. 2021. 14: e241156
4. Debette S, Grond-Ginsbach C, Bodenant M, Kloss M, Engelter S, Metso T. Differential features of carotid and vertebral artery dissections: The CADISP study. Neurology. 2011. 77: 1174-81
5. Diana F, Frauenfelder G, Saponiero R, Iaconetta G, Romano DG. Endovascular flow diversion in cervical internal carotid artery dissections. World Neurosurg. 2022. 162: 10
6. Hooker JD, Joyner DA, Farley EP, Khan M. Carotid stent fracture from stylocarotid syndrome. J Radiol Case Rep. 2016. 10: 1-8
7. Kidoguchi T, Fukui I, Abe H, Mori K, Tamase A, Yamashita R. Carotid artery stenting for spontaneous internal carotid artery dissection presenting with hypoglossal nerve palsy: A case report. Surg Neurol Int. 2022. 13: 225
8. Mokri B, Silbert PL, Schievink WI, Piepgras DG. Cranial nerve palsy in spontaneous dissection of the extracranial internal carotid artery. Neurology. 1996. 46: 356-9
9. Okada Y, Mitsui N, Ozaki H, Sanada T, Yamamoto S, Saito M. Carotid artery dissection due to elongated styloid process treated by acute phase carotid artery stenting: A case report. Surg Neurol Int. 2022. 13: 183
10. Paraskevas KI, Batchelder AJ, Naylor AR. Fate of distal false aneurysms complicating internal carotid artery dissection: A systematic review. Eur J Vasc Endovasc Surg. 2016. 52: 281-6
11. Pfaff JA, Weymayr F, Killer-Oberpflazer M. Fracture of a flow diverter in the cervical internal carotid artery due to Eagle syndrome. Neurointervention. 2023. 18: 72-5
12. Rizwan M, Smith C, Faro S, Malas MB. Transcarotid artery stenting for carotid artery pseudoaneurysm using flow reversal technique. J Vasc Surg Cases Innov Tech. 2018. 4: 115-8
13. Tan D, Crockett MT, Chiu AH. Delayed tine displacement of a CASPER carotid artery stent due to styloid process compression. Clin Neuroradiol. 2019. 29: 567-9
14. Yano T, Sasaki I, Kiyohara K, Kawanishi M. Carotid stent fracture due to Eagle syndrome after endovascular stenting for the treatment of acute ischemic stroke caused by internal carotid artery dissection: Case report. J Neuroendovascular Ther. 2019. 13: 454-61