- Department of Neurosurgery, Hospital Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Portugal.
- Department of Thoracic Surgery, Hospital Pulido Valente, Alameda das Linhas de Torres, Lisbon, Portugal.
Correspondence Address:
Diogo Roque, Neurosurgery, Hospital Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Lisbon, Portugal.
DOI:10.25259/SNI_1186_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Diogo Roque1, Daniel Cabral2, Cristina Rodrigues2, Nuno Simas1. Extradural thoracic nerve root hemangioblastoma approached by a combined posterior thoracic spine and video-assisted thoracoscopic surgery: A case report. 12-Jan-2022;13:10
How to cite this URL: Diogo Roque1, Daniel Cabral2, Cristina Rodrigues2, Nuno Simas1. Extradural thoracic nerve root hemangioblastoma approached by a combined posterior thoracic spine and video-assisted thoracoscopic surgery: A case report. 12-Jan-2022;13:10. Available from: https://surgicalneurologyint.com/surgicalint-articles/11342/
Abstract
Background: Hemangioblastomas commonly occur in the posterior fossa and are typically attributed to sporadic or familial Von Hippel–Lindau disease. Spinal hemangioblastomas, found in 7–10% of patients, are usually located within the cord (i.e., intramedullary). Here, a 58-year-old male presented with a purely extradural hemangioblastoma involving a spinal root that was surgically excised.
Case Description: A 58-year-old male was admitted with a progressive paraparesis and incomplete sensory deficit. The magnetic resonance imaging documented a solid dumbbell-shaped lesion that extended through the left T3-T4 foramen resulting in nerve root and spinal cord compression. Following arterial embolization and lesion excision by both neurosurgeons and thoracic surgeons, the patient’s deficits improved. The postoperative computed tomography scan documented complete tumor removal, and the neuropathology revealed a hemangioblastoma.
Conclusion: Here, we describe a 58-year-old male with a purely extradural thoracic foraminal T3-T4 dumbbell-shaped hemangioblastoma successfully treated by both embolization and surgical excision.
Keywords: Extradural hemangioblastoma, Spinal cord compression, Von Hippel–Lindau disease
INTRODUCTION
Hemangioblastomas are benign tumors that are either sporadic or associated with Von Hippel–Lindau disease (VHLD).[
CASE REPORT
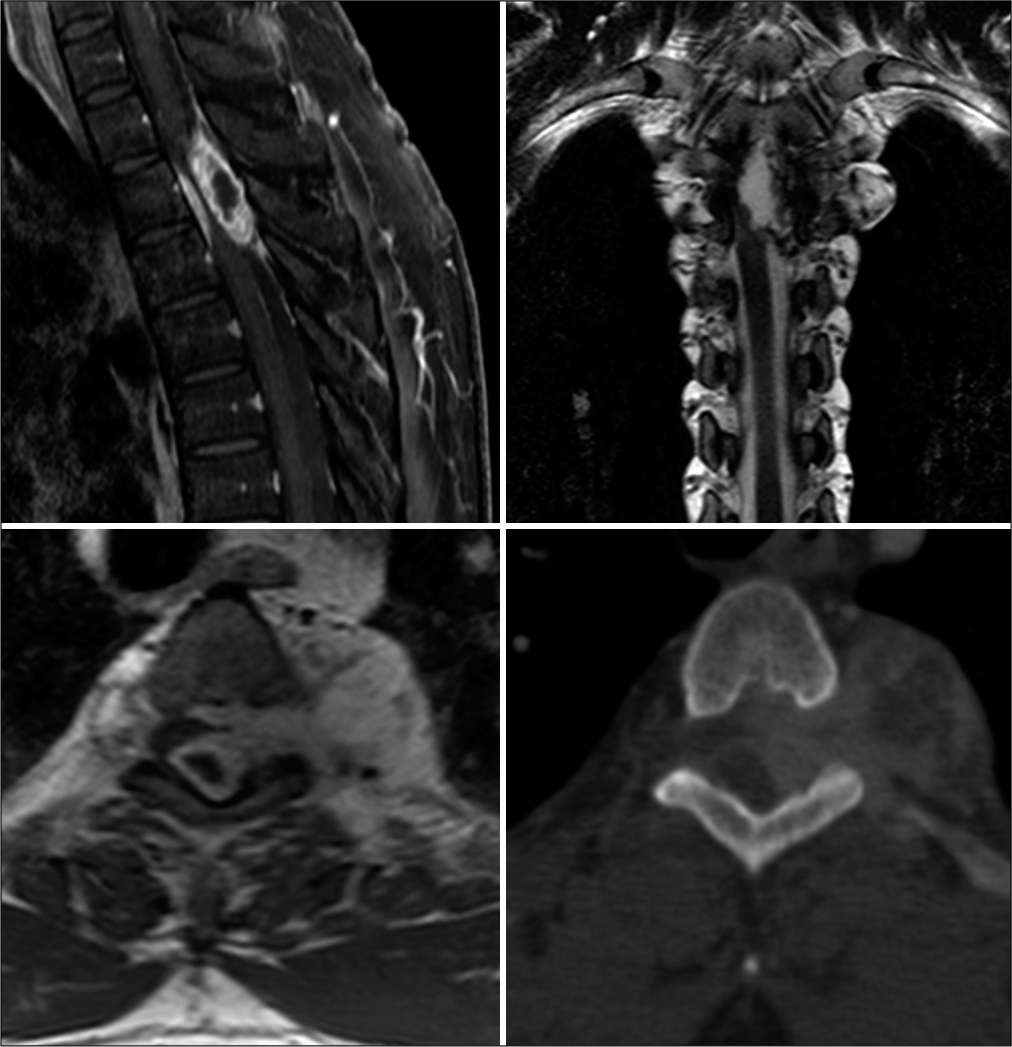
A 58-year-old male presented with a 6-month history of the gradual onset of an asymmetrical paraparesis (i.e., left leg 1/5 and right leg 3/5 proximal/2/5 distal with incomplete T4 sensory level). The patient had a familial history of VHLD. The thoracic magnetic resonance imaging (MRI) revealed a left T3-T4 intraforaminal/intracanalicular solid lesion with cord compression with extension through the foramen (i.e., measuring 40 × 35 × 35 mm – transverse × anterior-posterior × cephalocaudal axes). It was hypointense/isointense on T1 hyperintense on T2/short-tau inversion recovery and uniformly enhanced with gadolinium. The preoperative computed tomography (CT) scan documented chronic T3 vertebral body scalloping and left T3-T4 foramen widening [
Figure 1:
Preoperative MRI and CT features of the lesion. Top left: sagittal T1-weighted spectral presaturation with inversion recovery sequence with gadolinium enhancement showing the hyperintense solid component of the lesion inside the dorsal spinal canal, with a small hypointense cystic component. Top right: coronal T2-weighted sequence showing the severe compression on the spinal cord from the lesion and its component extending through the left T3-T4 foramen to form an intrathoracic component. Bottom left: axial T1-weighted sequence with gadolinium enhancement showing the mainly solid lesion. Bottom right: bone window axial CT scan showing the corresponding foramen widening.
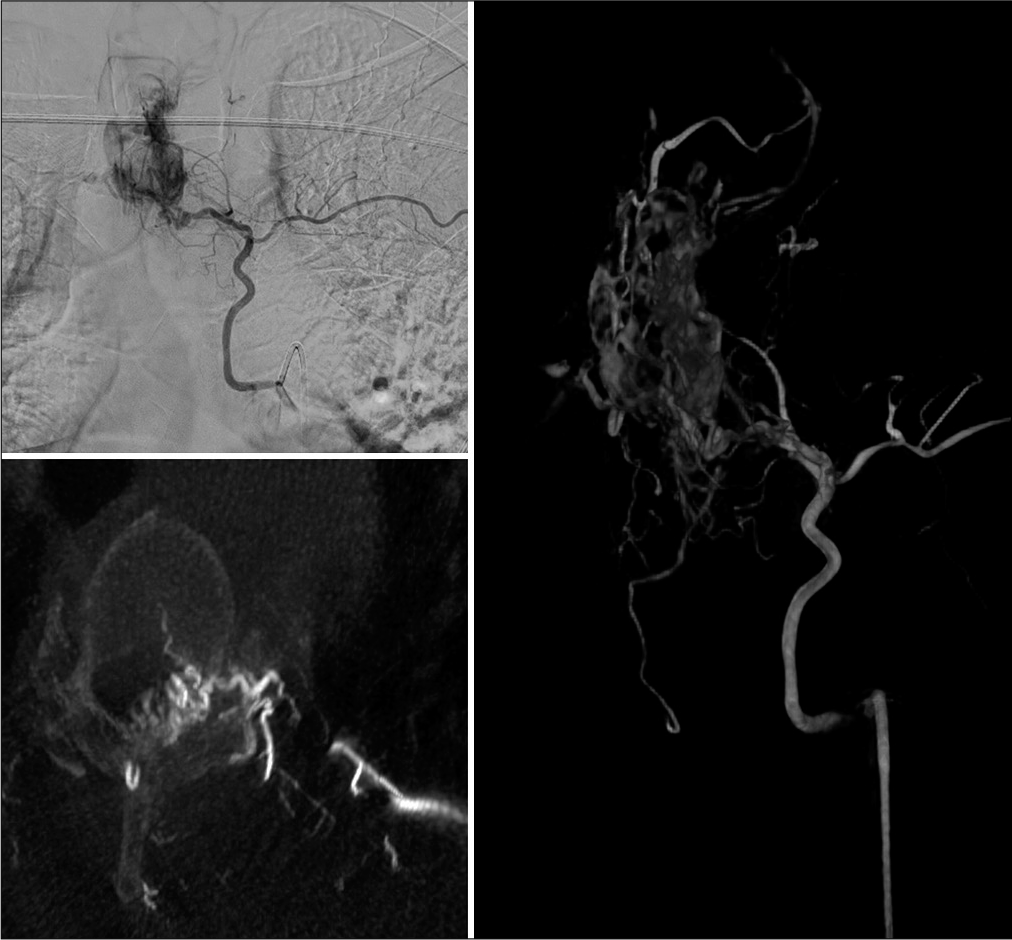
Angiography and preoperative embolization
Angiography revealed that the tumor was fed from the left T4 intercostal artery which was selectively embolizated 24 h before surgery [
Figure 2:
Preoperative angiography. Top left: anterior-posterior view showing the hypervascular lesion component in the spinal canal. Bottom left: feeding vessel to the lesion traversing the left T3-T4 foramen seen on axial CT angiography. Right: three-dimensional angiographic reconstruction of the vasculature of the lesion and the main feeding vessel deriving from the left T4 intercostal artery.
Surgery
Neurosurgery first performed a T2, T3, and T4 laminectomy and a left unilateral T3-T4 facetectomy; this allowed for en bloc resection of the intraforaminal/intracanalicular extradural tumor. At surgery, the left T3 nerve root that was adherent to the tumor was sacrificed. Second, the thoracic surgeons removed the intrathoracic component of the tumor using video-assisted thoracoscopy.
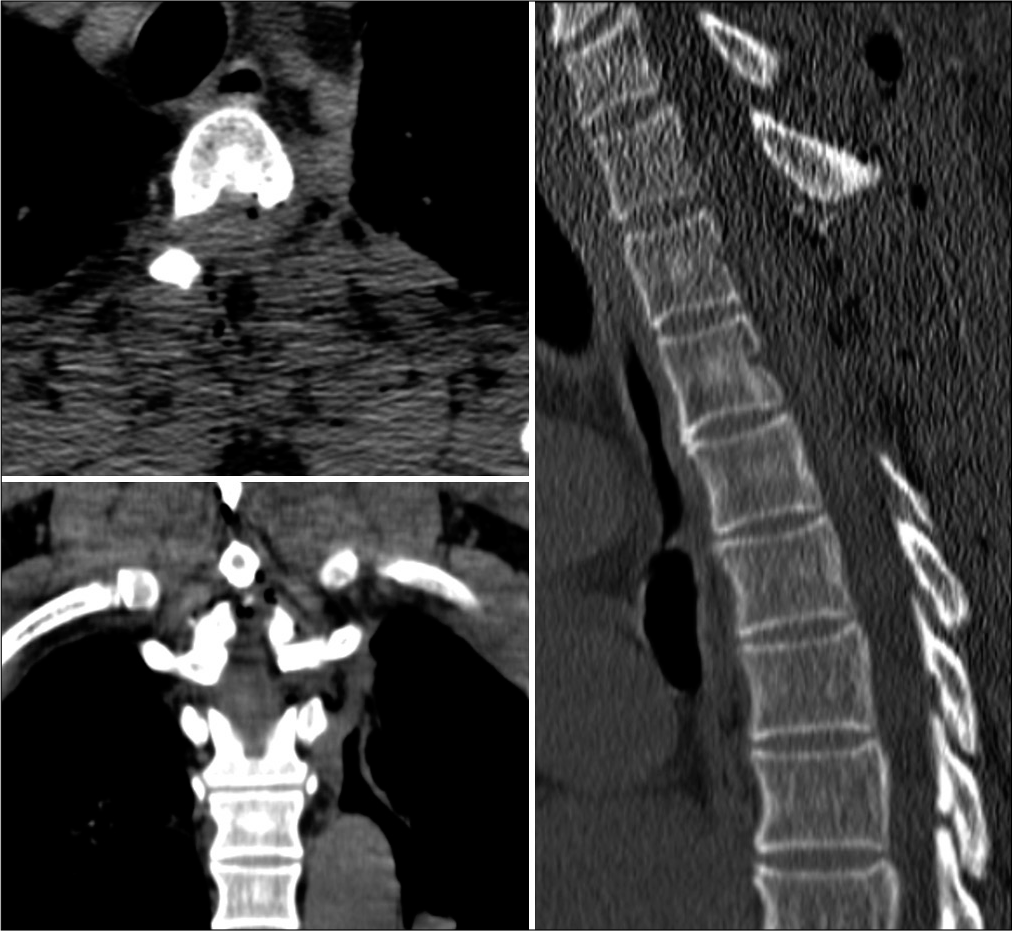
Postoperative course and CT
Postoperatively, the patient was neurologically intact and the postoperative CT documented complete tumor removal [
When discharged 3 days later, he had residual 3/5 left leg and 4/5 right leg weakness.
MRI 3 months later confirmed no tumor recurrence and his neurological status continued to improve with 4/5 paraparesis being able to walk with the aid of walkers.
Pathology
The histological analysis confirmed a hemangioblastoma; immunohistochemistry showed diffuse positivity for CD34 and vimentin, partial positivity for S100 protein, and focal positivity to EMA.
DISCUSSION
Only 7–10% of hemangioblastoma lesions occur in the spine.[
Extradural hemangioblastomas are found in the thoracic spine in 54% of cases followed by the lumbar spine.[
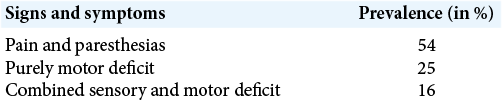
The most common signs and symptoms presenting extradural hemangioblastoma are shown in [
Preoperative MRI studies show these tumors readily enhance with contrast, while CT studies demonstrate more chronic bony changes (i.e., vertebral scalloping or foraminal enlargement).[
CONCLUSION
A 58-year-old male with a family history of Type 2 VHLD presented with a left T3-T4 purely extradural dumbbell thoracic hemangioblastoma that, once embolized, was readily excised in two stages by neurosurgery followed by thoracic surgery teams.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arumalla K, Deora H, Rao S, Shashidhar A, Rao MB. Spinal extradural hemangioblastoma: A systematic review of characteristics and outcomes. J Craniovertebr Junction Spine. 2020. 11: 254-61
2. Aytar MH, Yener U, Ekşi MŞ, Kaya B, Özgen S, Sav A. Purely extradural spinal nerve root hemangioblastomas. J Craniovertebr Junction Spine. 2016. 7: 197-200
3. Bisceglia M, Muscarella LA, Galliani CA, Zidar N, Ben-Dor D, Pasquinelli G. Extraneuraxial hemangioblastoma: Clinicopathologic features and review of the literature. Adv Anat Pathol. 2018. 25: 197-215
4. Laviv Y, Rappaport ZH. Cord compression due to extradural thoracic nerve root hemangioblastoma. Br J Neurosurg. 2015. 29: 281-4
5. Purandare HR, Misra BK. Thoracic nerve root hemangioblastoma: A rare cause of posterior mediastinal mass. World Neurosurg. 2012. 78: 192.E1-3