- Department of Spine Surgery, Indore Spine Centre, Indore, Madhya Pradesh, India
- Department of Spine Services, Indian Spinal Injuries Centre, New Delhi, India
Correspondence Address:
Vaibhav Goyal
Department of Spine Services, Indian Spinal Injuries Centre, New Delhi, India
DOI:10.25259/SNI_855_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Prasad Patgaonkar1, Vaibhav Goyal1, Nandan Marathe2. Extramedullary myeloid sarcoma mimicking tuberculosis of spine: A case report and literature review. 19-Apr-2021;12:178
How to cite this URL: Prasad Patgaonkar1, Vaibhav Goyal1, Nandan Marathe2. Extramedullary myeloid sarcoma mimicking tuberculosis of spine: A case report and literature review. 19-Apr-2021;12:178. Available from: https://surgicalneurologyint.com/surgicalint-articles/10729/
Abstract
Background: A definitive diagnosis of spinal tuberculosis (TB) remains challenging. The “gold standard” is to obtain histopathological confirmation of the lesion. This analysis highlights how to avoid missing the diagnosis of an extramedullary myeloid sarcoma (EMS) versus TB.
Case Description: A 25-year-old male presented with paraparesis. Although this was first attributed to TB spondylodiscitis, a PET-CT and reevaluation of the biopsy specimen both confirmed the diagnosis of an EMS.
Conclusion: Nontubercular spinal disease should be suspected when a patient deteriorates despite the institution of antitubercular therapy for a reasonable duration. Further, microbiological and/or pathological confirmation is warranted to direct appropriate treatment and differentiate spinal TB from other entities as, in this case, an EMS.
Keywords: Myeloid sarcoma, Spine, Tuberculosis
INTRODUCTION
Extramedullary myeloid sarcoma (EMS) may involve any organ or tissue. Skin, bone, and lymph nodes are most frequently affected, with vertebral involvement being extremely rare. Here, we present a 25-year-old male who was originally diagnosed and treated for tuberculosis (TB) of spine, where the ultimate correct diagnosis was EMS.
CASE REPORT
A 25-year-old male originally presented with mid-back pain of 2 months duration. After a T8 thoracic CT-guided biopsy, he was diagnosed/treated for TB spondylitis with bed rest and appropriate antibiotic therapy. However, 1 month following his initial presentation, he developed worsening of his mid-back pain (VAS score 8), chest pain, shortness of breath, and a progressive lower extremity paraparesis (3/5 proximal and 4/5 distal).
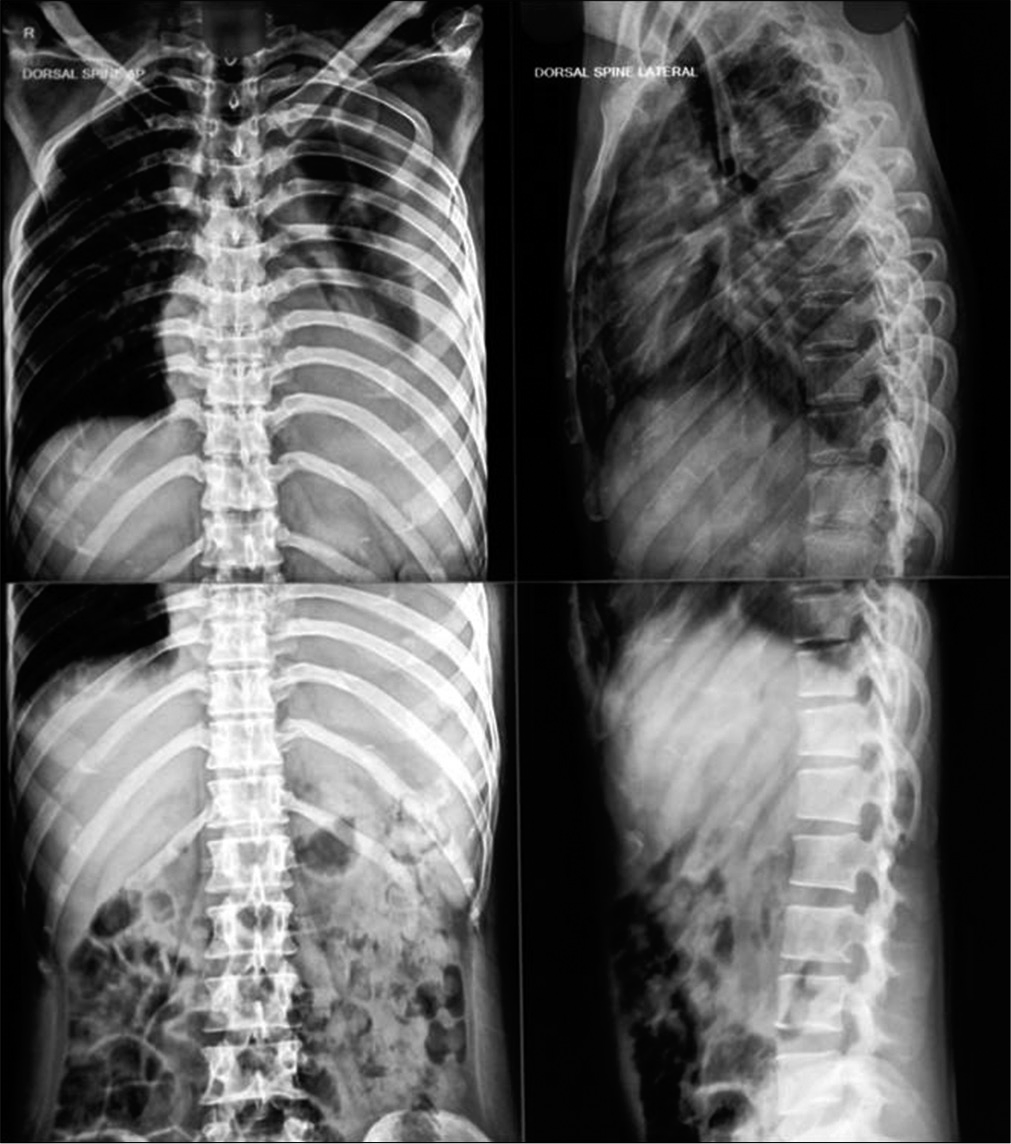
X-ray and MR studies
The chest X-ray showed a pleural effusion, while the thoracic spine X-ray demonstrated T8 vertebral collapse. Further, the thoracic spine MRI showed a posterior epidural collection extending from T7 to T9 resulting in cord compression. Of interest, lumbar X-rays and lumbar MR scan both demonstrated an additional although smaller, asymptomatic L3 vertebral body lesion [
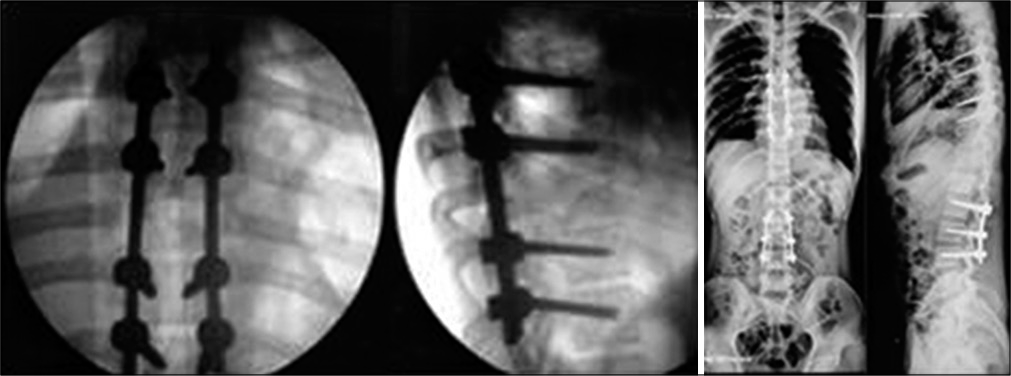
Surgery
The patient’s progressive myelopathy prompted a T8, T9 laminectomy that included a culture/biopsy of the lesion, epidural debridement, and T6-T10 pedicle screw fixation [
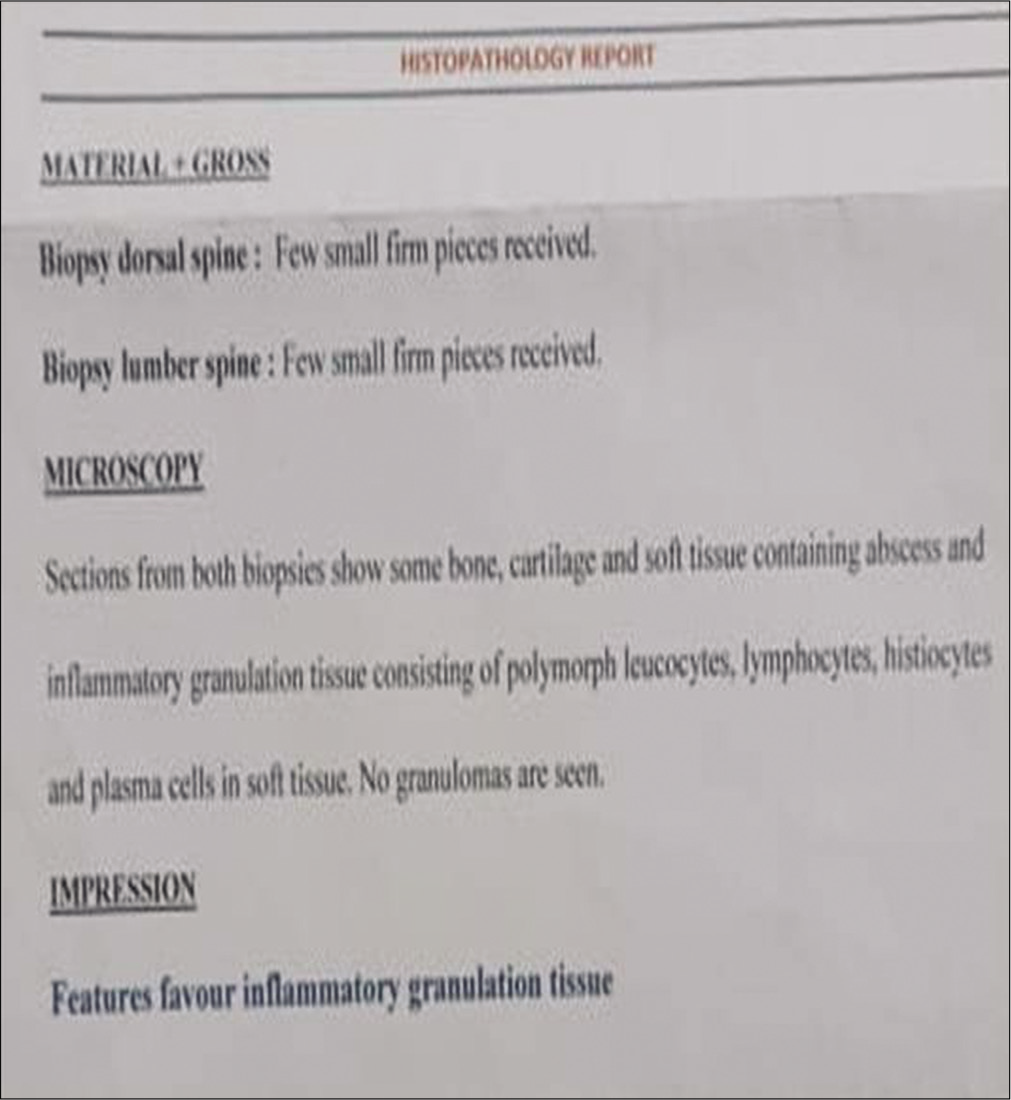
Pathology/culture
The pathology showed only inflammatory granulation tissue, and the staining for all organisms, including Mycobacterium tuberculosis (MTB), was negative [
Postoperative course
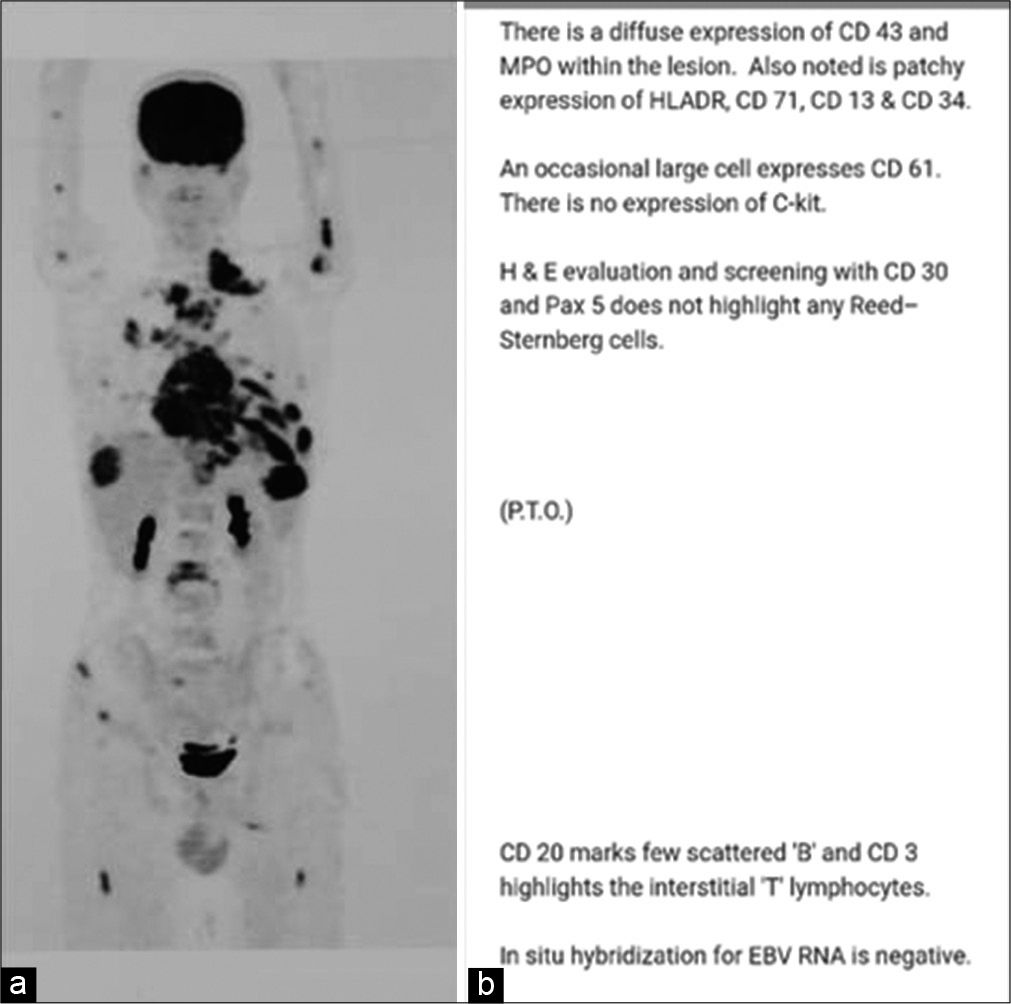
Postoperatively, the patient’s back pain (VAS score 2) improved, and he showed significant neurological recovery (e.g., 4/5 function proximally, 5/5 distally). However, within 3 days, he developed an increased left-sided pleural effusion (1700 cc). Tissue culture and MTB DNA reverse transcriptase-polymerase chain reaction of the fluid were negative. Four weeks postoperatively, when he returned with dyspnea and cough, the PET-CT scan revealed a metabolically active osteolytic lesion predominantly involving the T8 vertebral body, with extension into the T7, T9, and T11 vertebral bodies, involving the left 7th rib, as well as multiple other sites [
Figure 5:
(a) PET-CT scan showed metabolically active osteolytic lesion predominantly in D8 vertebra and in multiple regions such as D7, D9, D11 vertebral bodies, left 7th rib, sternum, and right iliac bone along with bilateral pleural effusions, mediastinal, and left supraclavicular lymphadenopathy and soft-tissue lesions in the left orbit and left temporal region of brain. (b) Surgical site biopsy and its paraffin block with further biopsy from the left 7th rib and immunohistochemistry studies confirmed it to be extramedullary myeloid sarcoma.
Biopsy of the left 7th rib and immunohistochemistry studies confirmed that the lesion was an EMS [
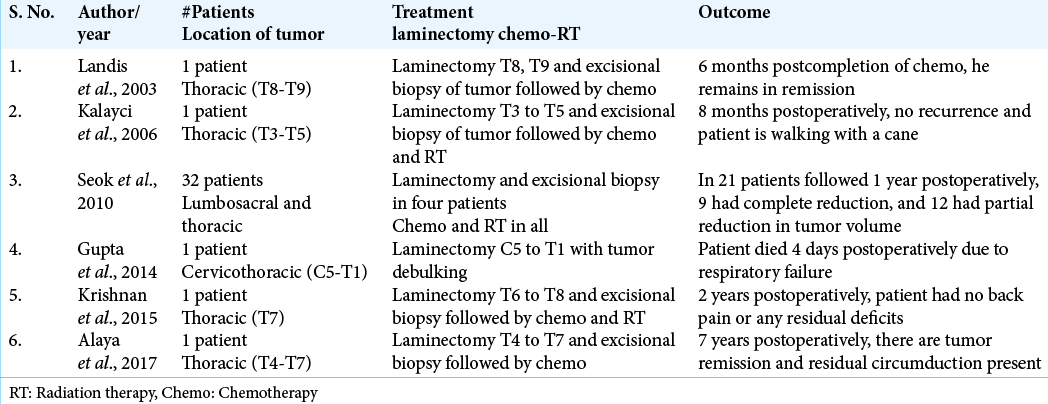
DISCUSSION
Frequency and differential diagnosis for EMS
EMS (also known as myeloid sarcoma MS, granulocytic sarcoma, or myeloblastoma) is rare. Patients ages can range from 1 to 81. EMS commonly affects skin, bone, and lymph nodes, but rarely presents in the spine.[
Diagnostic studies for EMS
EMS can present as single or multifocal lesions; 2–8% of these patients will have acute myeloid leukemia (AML). CT and MRI studies help differentiate EMS from hemorrhage or abscesses. Stölzel et al. emphasized that fluorodeoxyglucose PET-CT also additionally helped document extramedullary AML.[
CONCLUSION
EMSs of the spine are rare. They must be biopsy confirmed to differentiate them from TB spondylodiscitis (i.e., in endemic areas) and other lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Burnett A, Wetzler M, Löwenberg B. Therapeutic advances in acute myeloid leukemia. J Clin Oncol. 2011. 29: 487-94
2. Cunningham I. Extramedullary sites of leukemia relapse after transplant. Leuk Lymphoma. 2006. 47: 1754-67
3. Lan TY, Lin DT, Tien HF, Yang RS, Chen CY, Wu K. Prognostic factors of treatment outcomes in patients with granulocytic sarcoma. Acta Haematol. 2009. 122: 238-46
4. Mostafavi H, Lennarson PJ, Traynelis VC. Granulocytic sarcoma of the spine. Neurosurgery. 2000. 46: 78-83
5. Ofran Y, Rowe JM. Induction and postremission strategies in acute myeloid leukemia: What is new?. Curr Opin Hematol. 2011. 18: 83-8
6. Seok JH, Park J, Kim SK, Choi JE, Kim CC. Granulocytic sarcoma of the spine: MRI and clinical review. AJR Am J Roentgenol. 2010. 194: 485-9
7. Stölzel F, Röllig C, Radke J, Mohr B, Platzbecker U, Bornhäuser M, Paulus T. 18F-FDG-PET/CT for detection of extramedullary acute myeloid leukemia. Haematologica. 2011. 96: 1552-6
8. Suh YK, Shin HJ. Fine-needle aspiration biopsy of granulocytic sarcoma: A clinicopathologic study of 27 cases. Cancer. 2000. 90: 364-72