- Department of Radiology, Faculty of Medicine Universitas Airlangga - Dr. Soetomo Academic General Hospital, Surabaya, Indonesia,
- Department of Radiology, College of Medicine, University of Illinois at Chicago, Chicago, Illinois, United States,
- Department of Otorhinolaryngology, Head and Neck Surgery, Faculty of Medicine, Universitas Airlangga - Dr. Soetomo Academic General Hospital, Surabaya, Indonesia.
Correspondence Address:
Widiana Ferriastuti, Department of Radiology, Faculty of Medicine Universitas Airlangga - Dr. Soetomo Academic General Hospital, Surabaya, Indonesia.
DOI:10.25259/SNI_638_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Suga Marthawati1, Widiana Ferriastuti1, Suresh K. Mukherji2, Artono Artono3. Extraosseous Ewing sarcoma in the fossa jugular: A rare case report. 27-Oct-2023;14:382
How to cite this URL: Suga Marthawati1, Widiana Ferriastuti1, Suresh K. Mukherji2, Artono Artono3. Extraosseous Ewing sarcoma in the fossa jugular: A rare case report. 27-Oct-2023;14:382. Available from: https://surgicalneurologyint.com/surgicalint-articles/12612/
Abstract
Background: Extraosseous Ewing sarcoma (EES) is a rare case that accounts for 20% of Ewing sarcoma cases. EES is the second most prevalent pediatric malignancy after peripheral primitive neuroectodermal tumors. EES mostly arise from soft tissue and extra-skeletal. Computed tomography (CT) and magnetic resonance imaging (MRI) are primary modalities for determining tumor location, characteristics, type, and extent of tumors. In addition, for presurgical management, radio intervention with arterial embolization is needed as a preoperative.
Case Description: We present a case of a 15-year-old boy diagnosed with EES. He had a “horn-like” tumor that grew progressively on his right ear over 5 months. Head CT scan and MRI were conducted to assess the extent. Embolization was performed before surgery. The surgery was conducted to excise the tumor radically. The histology pathology examination showed EES.
Conclusion: EES rarely occurs in the head and neck. This may manifest as a solid mass with bleeding components that destroy the nearby bones, with exophytic mass. Imaging is important for early finding and detecting complications of EES.
Keywords: Computed tomography scan, Ewing sarcoma, Extraosseous Ewing sarcoma, Magnetic resonance imaging
INTRODUCTION
Extraosseous Ewing sarcoma (EES) is a rare variant of Ewing sarcoma. The EES prevalence is 10 times lower than bone Ewing Sarcoma. EES is highly malignant, particularly in young adults.[
A systematic review of 29 studies showed that the most commonly involved thoracic region is the most common site (33%), followed by extremities (31%) and then head and neck (14%).[
Another study (18 EES cases) performed a computed tomography (CT) scan in 13 patients and a magnetic resonance imaging (MRI) in five patients.[
EES rarely occurs in the head and neck. Diagnosing uncommon tumors with nonspecific clinical manifestations was challenging. An accurate diagnosis can significantly improve prognosis with a better survival rate.[
CASE DESCRIPTION
A 15-year-old Asian boy came to the ear, nose, and throat– head and neck department with the chief complaint of a rapid lump behind the right ear, which had developed fast at 5 months. This “horn-like” tumor comes from the external meatus of the right ear. The tumor tends to bleed easily [
The physical examination revealed facial right nerve VII paralyzed, conductive hearing loss of the right ear, retroauricular erythema, and a bleeding mass from the external auditory externus. The tympanic membrane cannot be evaluated. The laboratory examination showed slight leukocytosis (11.210/μL), normal hemoglobin level (10 g/dL), and normal neutrophil count (81.7).
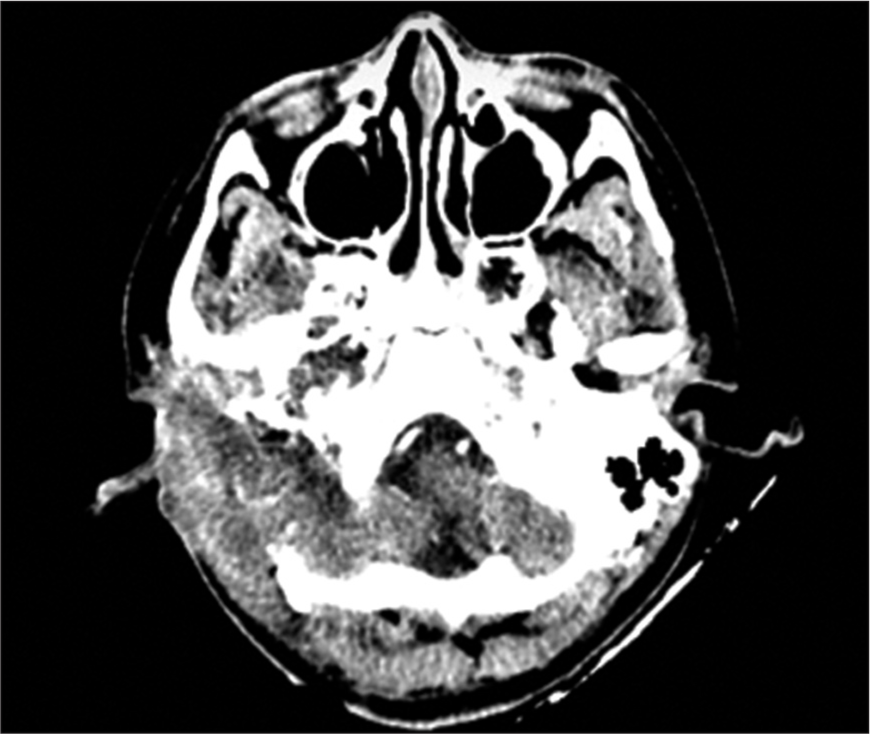
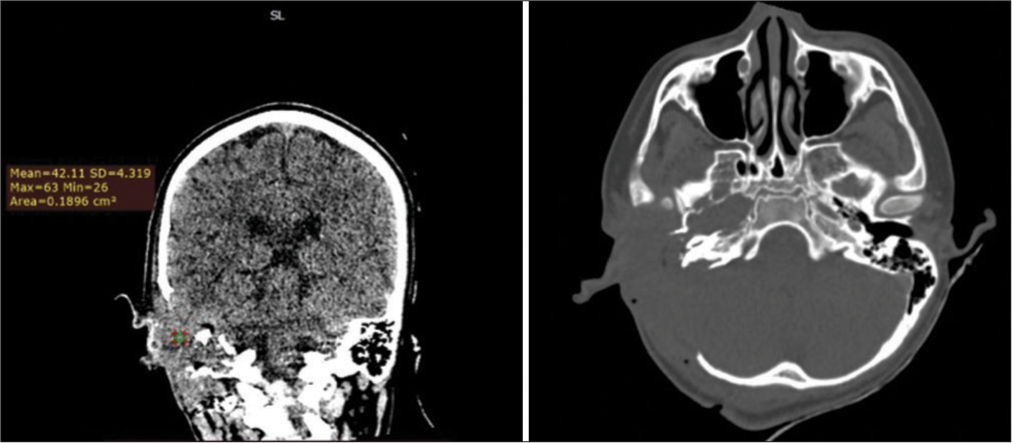
Head CT scan revealed soft-tissue solid mass enhancement (7.1 × 6.6 × 8 cm) in the right jugular fossa with an irregular border. The mass is exophytic into the middle ear, mesotympanum, and hypotympanum. It reaches the right external meatus. CT scan showed contrast enhancement (72HU) with evidence of mass-induced destruction in the right mastoid and right temporal bone. The feeding vessels come from the segment temporalis superficial and posterior segment auricular artery from the right external carotid artery (ECA) [
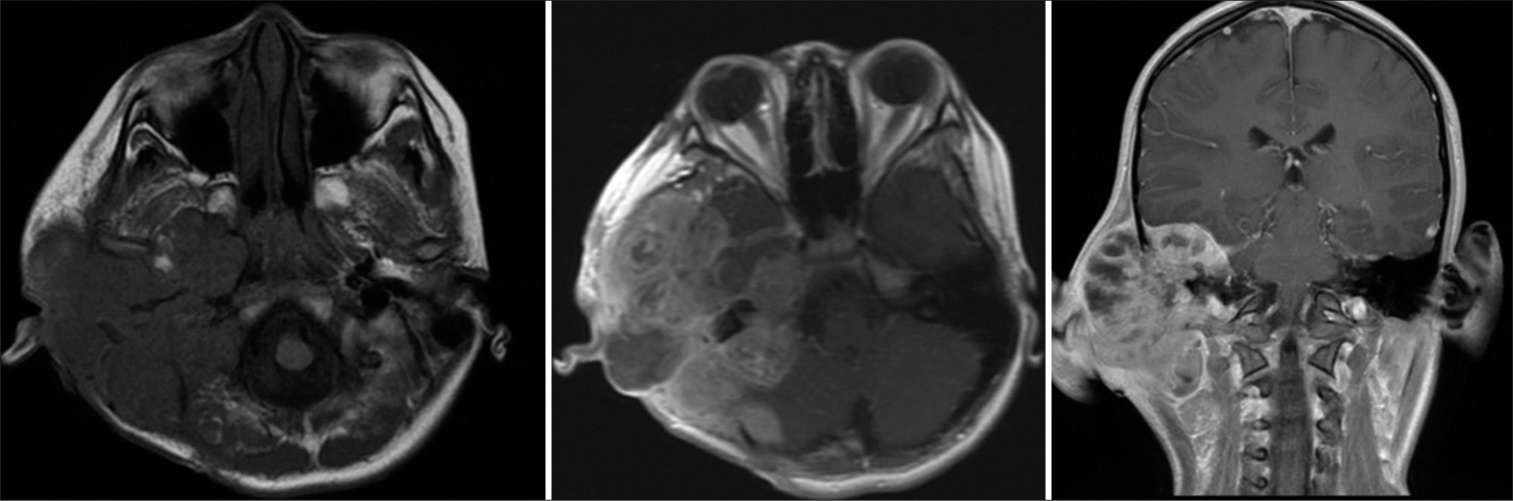
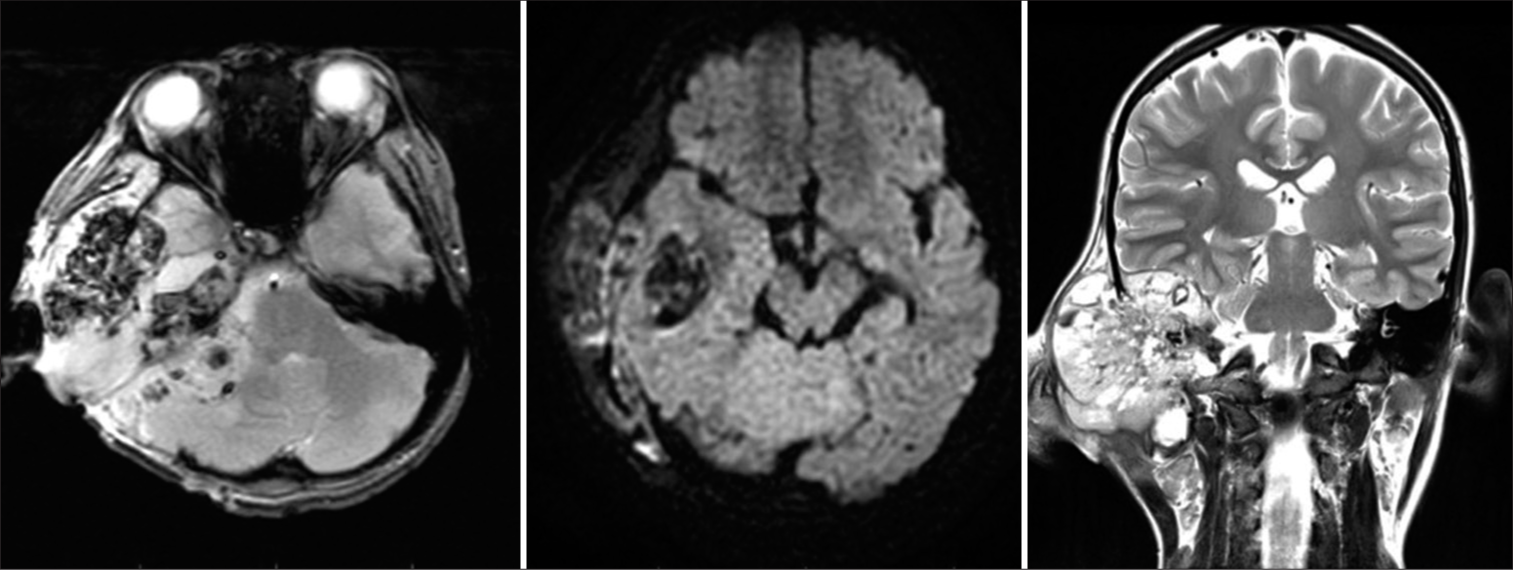
MRI demonstrated isointense to hyperintensity on the T1-weighted image, with prominent flow voids forming a “salt and pepper image” on the T2-weighted image and unrestricted diffusion in the diffusion-weighted imaging area, which lacks contrast enhancement. The mass destroyed the right mastoid, right temporal bone, and part of the sphenoid bone. There was an intracranial extradural extension. The mass compressed the right posterior fossa, right cerebellum, and right temporal lobe. The mass size was 7.8 × 6.7 × 6.6 cm extending to the right fossa jugular, with exophytic to the middle ear, mesotympanum, and hypotympanum until the right external meatus with feeding arteries from the superficial temporal segment and the posterior auricular artery segment of the right ECA branch [
Figure 5:
Head magnetic resonance imaging with contrast axial and coronal view, hyperintense with prominent flow voids forming a salt and pepper image on T2-weighted image, unrestricted diffusion in the diffusion-weighted imaging area, which did not show contrast enhancement, a mass was seen destroying the right mastoid, right temporal bone and part of the sphenoid looks intracranial extradural extension.
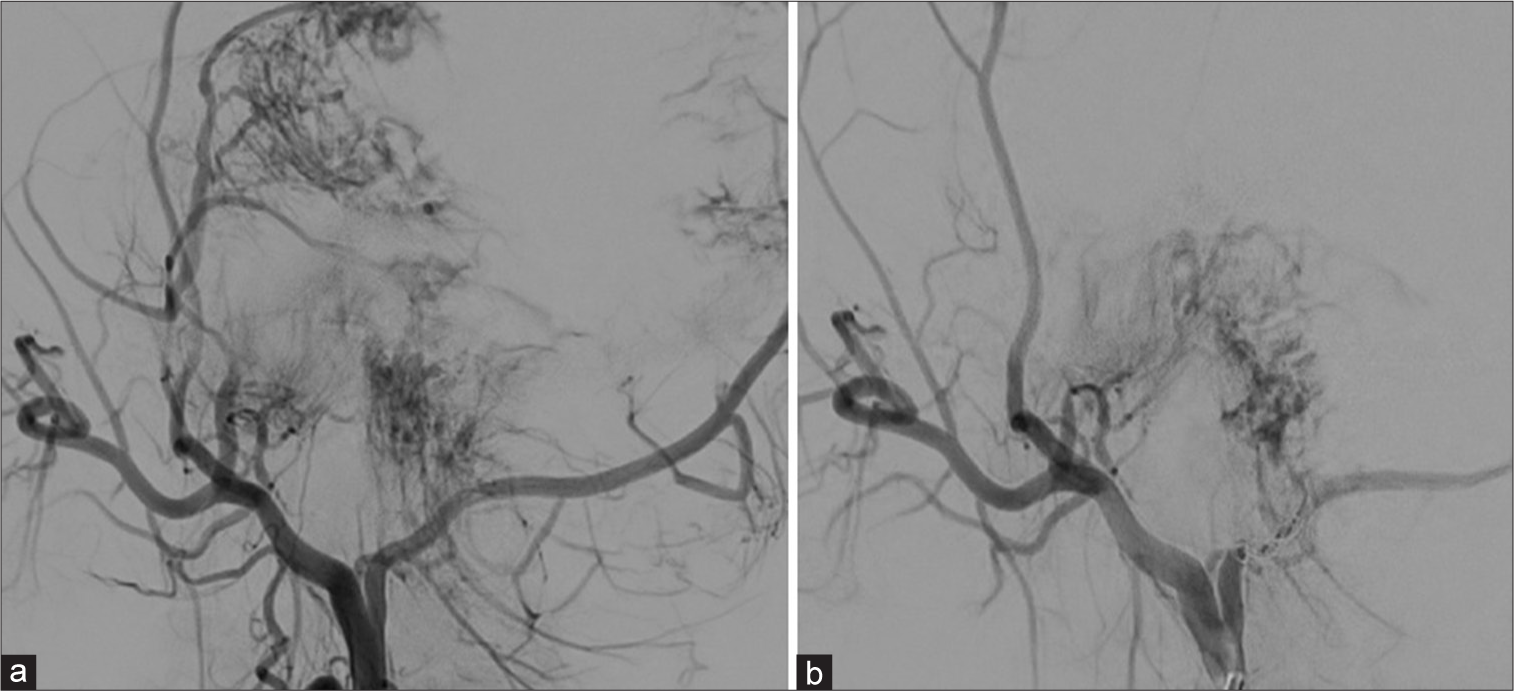
The definitive management approach for this patient involved radical surgery, preceded by digital subtraction angiography (DSA) abolition before surgery. The DSA angiography revealed a hypervascular lesion supplied by the right ECA, with branches from temporalis superficialis and right occipital arteries. We performed embolization using PVa 355-500 mm in the ECA branch to the occipital and superficial right temporalis arteries [
DISCUSSION
This patient was 15 years old. The previous studies showed that this condition commonly occurs in individuals below 20 years.[
This patient had a solid mass (approximately 10 × 7, 6 × 81 cm) in the right fossa jugular with a bleeding component. MRI showed that this tumor had vascularization from the temporalis superficialis segment artery and posterior segment auricular artery. MRI also showed an exophytic in the middle ear, involving epi, meso, and hypotympanic until the right meatus externus. Contrast-enhanced CT scan showed rim contrast enhancement and mass destruction of the right mastoid and right temporal bone, with evidence of intracranial extradural extension.
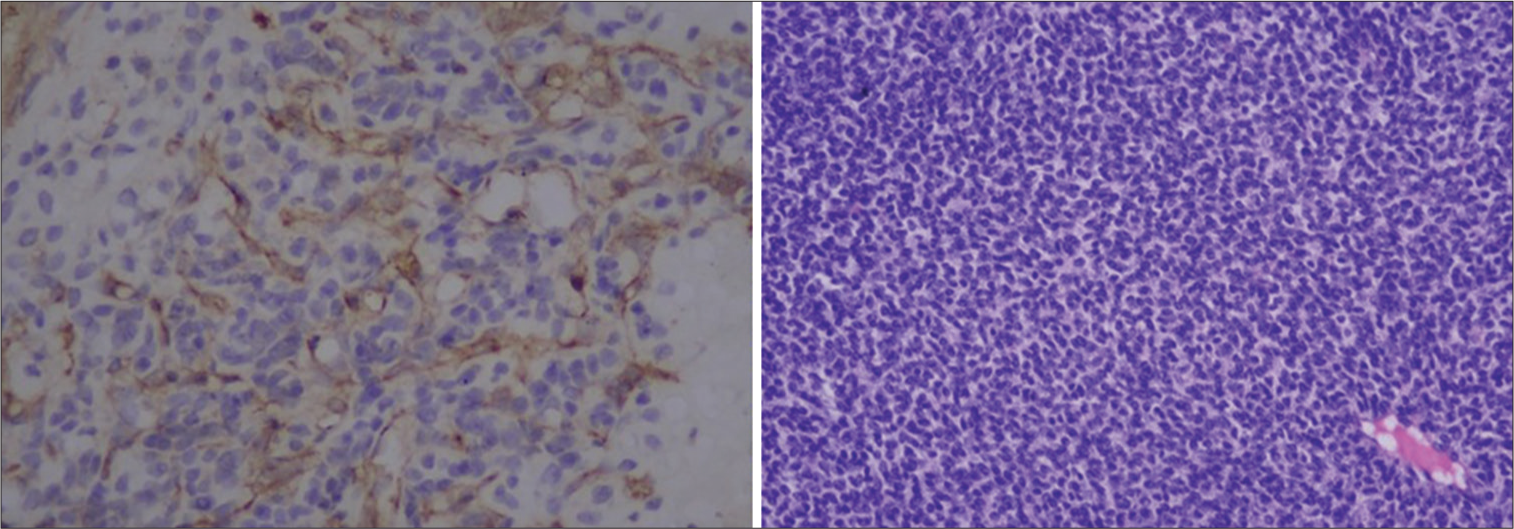
According to this finding, this case was decided to surgical intervention. Presurgical DSA to minimize intraoperative bleeding was conducted. The histopathology examination showed EES rather than a rhabdomyosarcoma though both belong to the same in the round cell family tumor. It could be a differential diagnosis, it was positive in CD-99, S-100, and synaptophysin.[
The patient had improved general condition after tumor resection but he passed away after chemotherapy. It is essential to note that the standard therapy of EES is radical resection combined with chemotherapy. Radiotherapy may also play an important role. Nevertheless, it is crucial to be aware that secondary metastases can develop.[
CONCLUSION
Here, we present a case of a 15-year-old boy diagnosed with EES characterized by a giant mass that caused bone destruction and exophytic growth toward the right ear. Prompt diagnosis and early diagnosis must be established in this patient because EES is the second most common malignancy among teenagers. Early intervention has better outcomes. Biopsy is a gold standard. CT and MRI are also important for tumor evaluation. Presurgical DSA is important to minimize intraoperative bleeding.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abboud A, Masrouha K, Saliba M, Haidar R, Saab R, Khoury N. Extraskeletal Ewing sarcoma: Diagnosis, management and prognosis. Oncol Lett. 2021. 21: 354
2. Alexander A, Hunter K, Rubin M, Bhat AP. Extraosseous Ewing’s sarcoma: Pictorial review of imaging findings, differential diagnosis, and pathologic correlation. Indian J Radiol Imaging. 2021. 31: 203-9
3. Almohaisen GA, Alhuwairini SF, Aljrayed MA, Alenezi MM, Alsaab F. Extraskeletal Ewing’s sarcoma of the head and neck region in pediatric patients: A case report and literature review. Int J Surg Case Rep. 2023. 106: 108142
4. Chatterjee P, Singh A, Kuruvilla V. Extraskeletal and skeletal Ewing sarcoma family of tumours in adults: A clinico radiological review of 50 cases. Int J Radiol Radiat Ther. 2017. 3: 192-6
5. Galyfos G, Karantzikos GA, Kavouras N, Sianou A, Palogos K, Filis K. Extraosseous Ewing sarcoma: Diagnosis, prognosis and optimal management. Indian J Surg. 2016. 78: 49-53
6. Ghandour M, Lehner B, Klotz M, Geisbüsch A, Bollmann J, Renkawitz T. Extraosseous Ewing sarcoma in children: A systematic review and meta-analysis of clinicodemographic characteristics. Children (Basel). 2022. 9: 1859
7. Ioannidou M, Tsotridou E, Samoladas E, Tragiannidis A, Kouskouras K, Sfougaris D. Unusual manifestation of extraosseous Ewing Sarcoma: Report of 3 cases. Balkan J Med Genet. 2022. 25: 77-81
8. Khosla D, Verma S, Punia RS, Dass A, Dimri K, Kaur G. Extraosseous Ewing’s sarcoma of the parapharyngeal space-a rare entity-with review of literature. Iran J Otorhinolaryngol. 2019. 31: 51-4
9. Patnaik S, Yarlagadda J, Susarla R. Imaging features of Ewing’s sarcoma: Special reference to uncommon features and rare sites of presentation. J Cancer Res Ther. 2018. 14: 1014-22
10. Xie CF, Liu MZ, Xi M. Extraskeletal Ewing’s sarcoma: A report of 18 cases and literature review. Chin J Cancer. 2010. 29: 420-4