- Department of Neurological Surgery, Wakayama Medical University, Wakayama, Japan.
Correspondence Address:
Takahiro Sasaki, Department of Neurological Surgery, Wakayama Medical University, Wakayama, Japan.
DOI:10.25259/SNI_806_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nao Ohtani, Takahiro Sasaki, Toshikazu Yamoto, Junya Fukai, Hiroki Nishibayashi, Naoyuki Nakao. Extremely slow-growing cerebellar ganglioglioma in an elderly patient. 02-Feb-2024;15:33
How to cite this URL: Nao Ohtani, Takahiro Sasaki, Toshikazu Yamoto, Junya Fukai, Hiroki Nishibayashi, Naoyuki Nakao. Extremely slow-growing cerebellar ganglioglioma in an elderly patient. 02-Feb-2024;15:33. Available from: https://surgicalneurologyint.com/surgicalint-articles/12728/
Abstract
Background: Gangliogliomas account for 0.4% of primary brain tumors. They mainly occur in the supratentorial compartment and typically affect only children and young adults. We present an especially rare case of cerebellar ganglioglioma in an elderly patient.
Case Description: A 76-year-old Japanese woman presented with headache and nausea from 1 month previously. She had been diagnosed with a cerebellar tumor in her childhood, but the lesion was asymptomatic at that time, and there was no evidence of an increase in size, so it had been monitored without surgery. At the time of presentation, she had not been examined for approximately ten years. On admission, magnetic resonance imaging indicated a T2 hypertense cyst in the cerebellar vermis. Post-contrast T1 imaging showed an enhanced mural nodule in the cyst. Cerebral angiography showed that none of the vertebral arteries were significant feeders. The tumor was removed through posterior fossa craniotomy. The histopathological diagnosis was ganglioglioma. The patient’s headache and nausea improved after surgery.
Conclusion: Our patient presented a very rare case of extremely slow-growing elderly ganglioglioma in the cerebellum. In patients with gangliogliomas, long-term follow-up is important because the disease may become symptomatic at an older age.
Keywords: Cerebellum, Cystic tumor, Elderly, Ganglioglioma, Slow-growing tumor
INTRODUCTION
Gangliogliomas are rare, slowly growing tumors composed of neoplastic mature ganglion cells in combination with glial cells. Gangliogliomas account for just 0.4% of primary brain tumors.[
CASE DESCRIPTION
A 76-year-old Japanese woman presented with headache and nausea from 1 month previously. She had been diagnosed with a cerebellar tumor in her childhood, but the lesion was asymptomatic at that time, and there was no evidence of an increase in size, so it had been monitored without surgery. Her last magnetic resonance imaging (MRI) was performed approximately ten years before her presentation. On admission, her consciousness was alert, and physical examination revealed no ataxia or gait disturbance. Computed tomography showed a heterogeneous cystic mass in the left cerebellum without calcification [
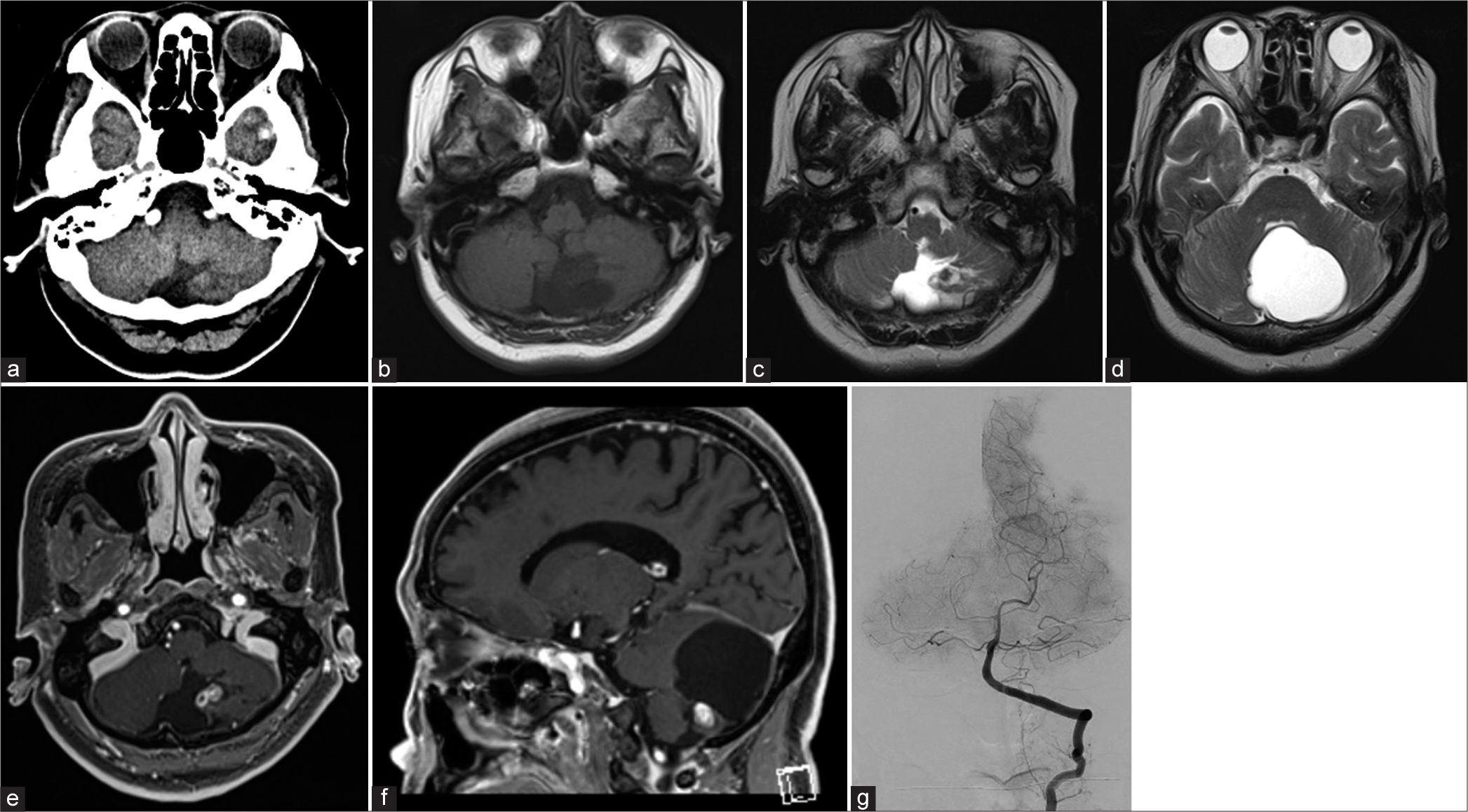
Figure 1:
Preoperative images. Preoperative computed tomography (a) shows an isodense mass in the left cerebellar tonsil. In magnetic resonance imaging, the mass shows low intensity in (b) T1-weighted images and high intensity in (c) T2-weighted images. T2 hypertense cyst (d) is located in the cerebellar vermis. Post-contrast T1-imaging shows an enhanced mural nodule in the cyst (e, axial view, and f: sagittal view). The cerebral angiography (g) shows no tumor stains.
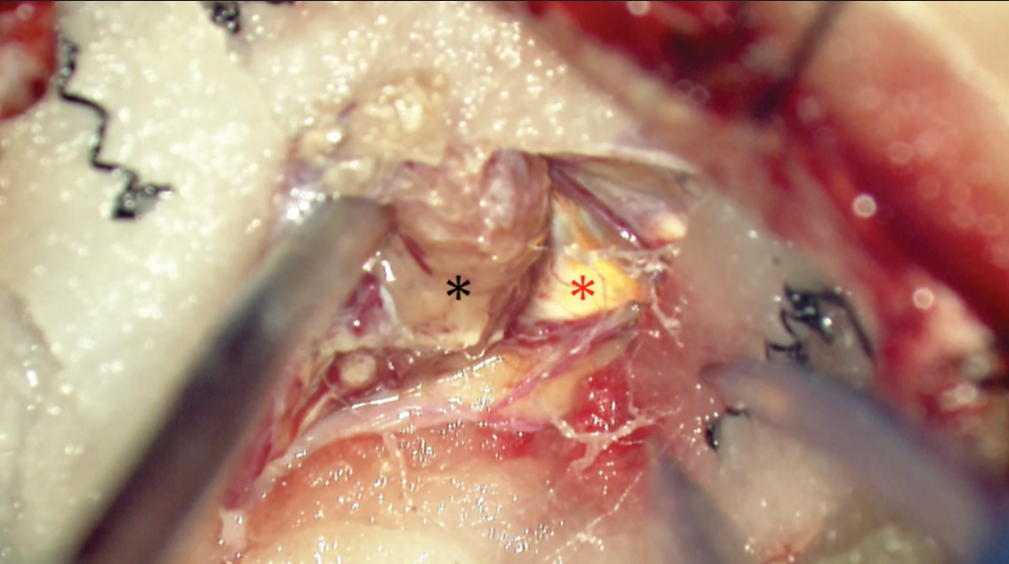
We performed tumor excision through posterior fossa craniotomy, incising the cyst and draining the xanthochromic fluid. The tumor was located within the cerebellar tonsil and was well-circumscribed from the surrounding parenchyma [
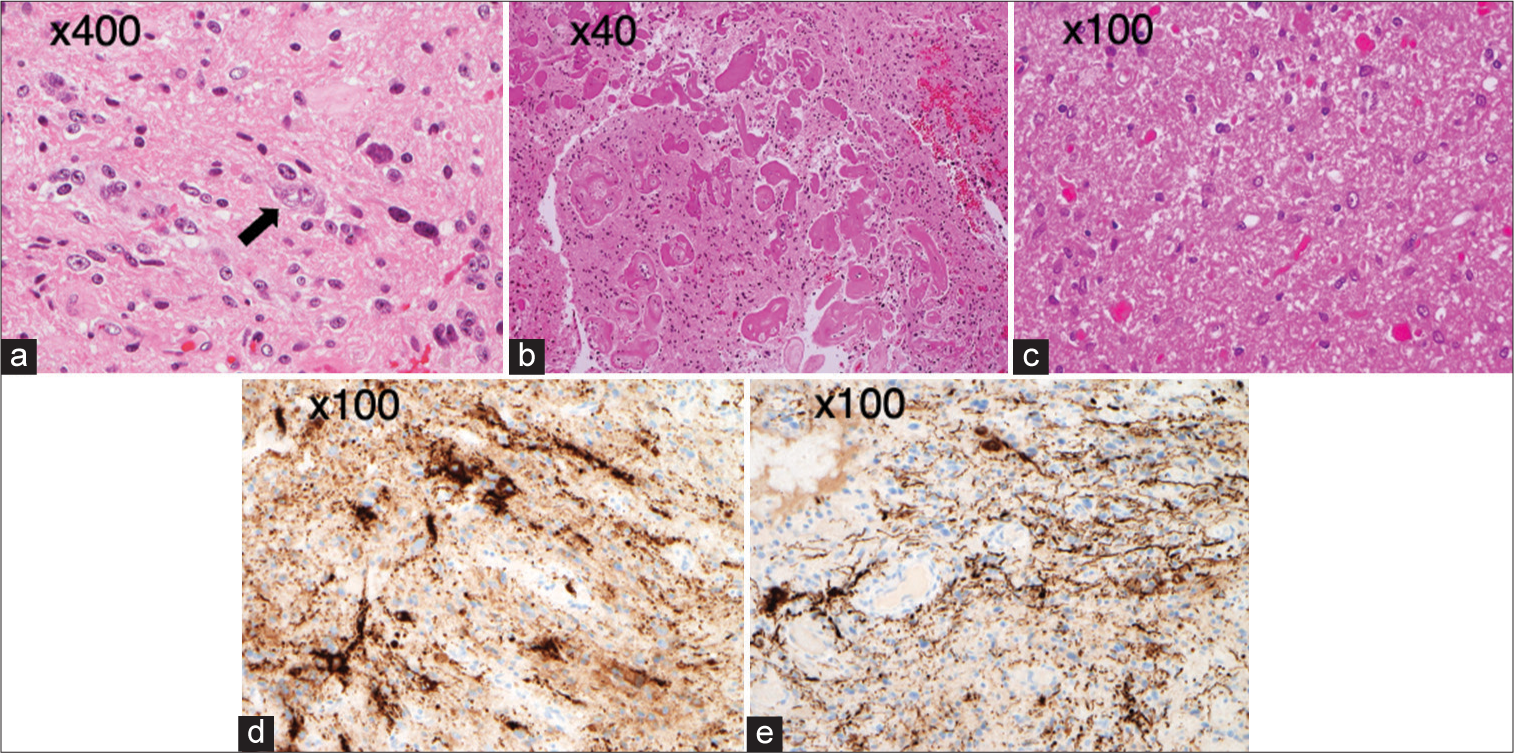
Figure 3:
Surgical specimens. Photomicrographs of the surgical specimen stained with hematoxylin and eosin show binuclear atypical ganglion-cell-like cells (a black arrow) and (a) proliferation of atypical glial cells showing mild pleomorphism between (b) hyalinized vessels, (c) eosinophilic granular bodies, and Rosenthal fibers. Immunohistochemical stains show that tumor cells are immunoreactive for (d) synaptophysin and (e) neurofilament protein.
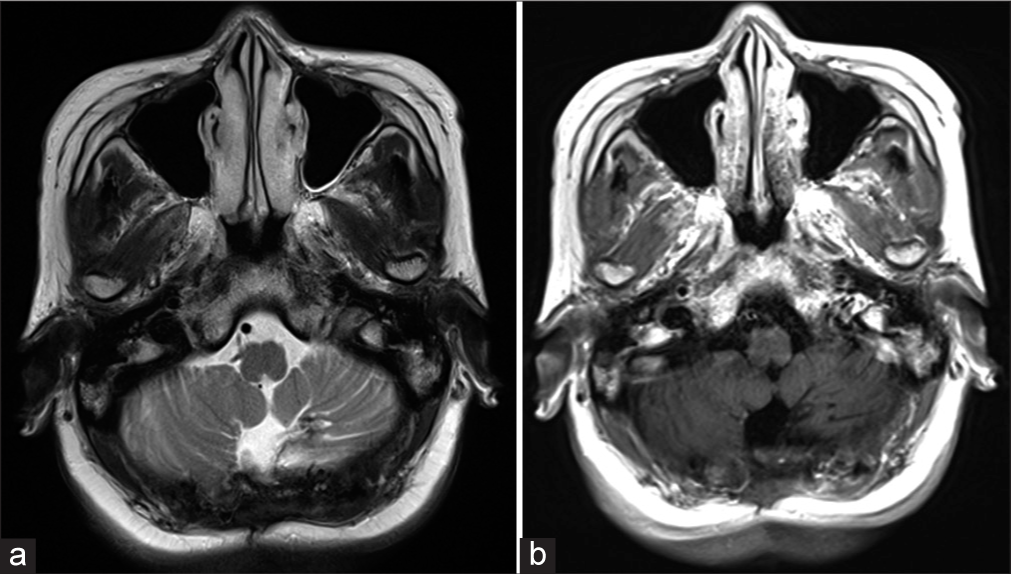
The patient’s headache and nausea improved after surgery. She exhibited no cerebellar symptoms postoperatively and had a favorable postoperative course, so she was discharged to home two weeks after surgery. At the 1-year follow-up, postoperative MRI showed total tumor removal, and there has been no recurrence [
DISCUSSION
Gangliogliomas are well-differentiated, slow-growing glioneuronal neoplasms composed of a combination of neoplastic ganglion and glial cells, molecularly characterized by mitogen-activated protein kinase pathway alteration.[
This case involved a cystic tumor with nodules in the cerebellum of an elderly patient. The differential diagnoses include hemangioblastoma, pilocytic astrocytoma, and metastatic tumor.[
Gangliogliomas are well-differentiated and indolent tumors with excellent prognosis. Surgical resection is the standard of care for ganglioglioma and generally yields a good outcome.[
CONCLUSION
We presented a rare case of extremely slow-growing ganglioglioma in the cerebellum in an elderly patient. Long-term follow-up of ganglioglioma is important because it may become symptomatic at an older age.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Dahiya S, Haydon DH, Alvarado D, Gurnett CA, Gutmann DH, Leonard JR. BRAFV600E mutation is a negative prognosticator in pediatric ganglioglioma. Acta Neuropathol. 2013. 125: 901-10
2. El Hamrouni I, Raftopoulos C, Duprez T, Wilms G. Cerebellar ganglioglioma in a young woman. Neurol Neurol Sci Open Access. 2020. 3: 1014
3. Jang EW, Cho JH, Chang JH, Ahn JY. Cerebellar ganglioglioma in an old patient. J Korean Neurosurg Soc. 2007. 42: 53-5
4. Komboz F, Zechel S, Malinova V, Mielke D, Rohde V, Abboud T. Infratentorial ganglioglioma mimicking a cerebellar metastasis. Int J Neurosci. 2022. 2: 1-5
5. WHO Classification of Tumours Editorial Boa, editors. WHO classification of tumors series: Central nervous system tumours. Lyon, France: International Agency for Research on Cancer; 2021. 6: Available from: https://publications.iarc.fr/601 [Last accessed on 2023 Sep 19]
6. Yust-Katz S, Anderson MD, Liu D, Wu J, Yuan Y, Olar A. Clinical and prognostic features of adult patients with gangliogliomas. Neuro Oncol. 2014. 16: 409-13