- Department of Neurosurgery, International Medical Center, Saitama Medical University, Hidaka, Saitama, Japan
- Department of Neurosurgery, Tanabe Neurosurgical Hospital, Osaka, Japan.
Correspondence Address:
Hidetoshi Ooigawa, Department of Neurosurgery, International Medical Center, Saitama Medical University, Hidaka, Saitama, Japan.
DOI:10.25259/SNI_652_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shunsuke Ikeda1, Hidetoshi Ooigawa1, Tatsuki Kimura1, Hideki Tanabe2, Hiroki Kurita1. Facet joint thickness and lumbar instability documented on myelo-computed tomography studies in patients with lumbar degenerative disease. 22-Sep-2023;14:342
How to cite this URL: Shunsuke Ikeda1, Hidetoshi Ooigawa1, Tatsuki Kimura1, Hideki Tanabe2, Hiroki Kurita1. Facet joint thickness and lumbar instability documented on myelo-computed tomography studies in patients with lumbar degenerative disease. 22-Sep-2023;14:342. Available from: https://surgicalneurologyint.com/surgicalint-articles/12567/
Abstract
Background: Various indicators of vertebral instability in patients with lumbar degenerative disease can be identified in myelo-computed tomography (CT) studies.
Methods: Of 120 patients, 45 with lumbar degenerative spondylolisthesis (LDS; 53 lumbar lesions) and 75 with lumbar spinal stenosis alone (LSS; 105 lesions) (2015–2019) myelo-CT studies and surgery confirmed the presence of lumbar instability. Myelo-CT findings indicative of instability included facet joint thickness (FJT), fluid in the facet joint, facet tropism, and air in the facet and/or disc.
Results: For the 120 study patients, FJT was significantly elevated in both the LDS and LSS groups.
Conclusion: FJT on myelo-CT is more specific for lumbar instability than other imaging parameters when evaluating LDS. An increase in FJT suggests vertebral instability likely warranting fusion.
Keywords: Facet, Lumbar degenerative disease, Lumbar degenerative spondylolisthesis, Lumbar spinal stenosis, Spine
INTRODUCTION
Facet joint thickness (FJT),[
MATERIALS AND METHODS
Study population
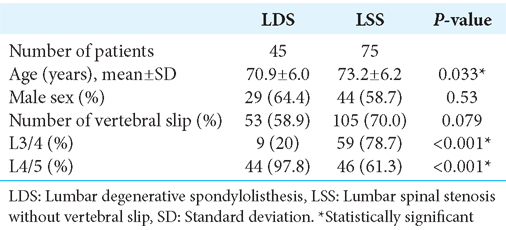
The study was approved by our Institutional Review Board. It included 120 patients, 45 with lumbar degenerative spondylolisthesis [LDS >25% slip or >3 mm,
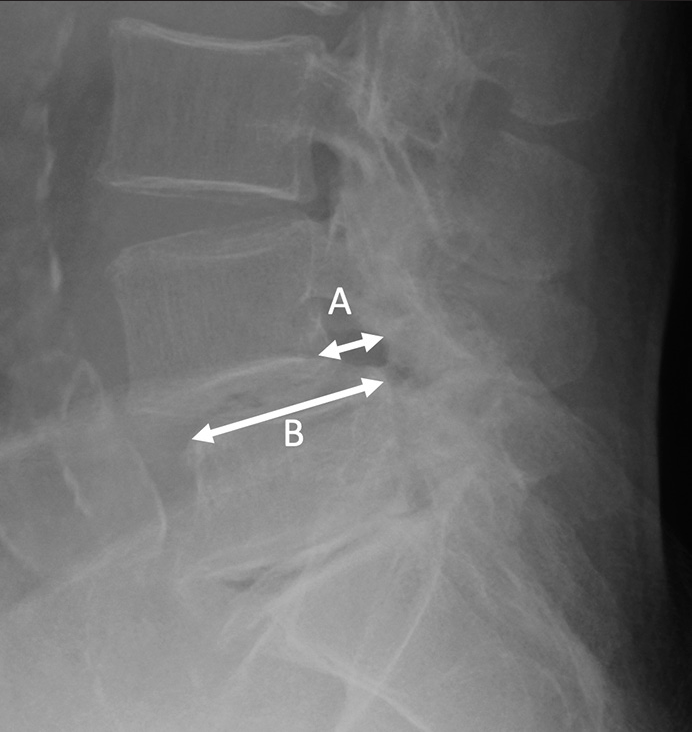
Figure 1:
Measurement of vertebral slip. (A) The distance between the tangents drawn on the posterior surface of the upper vertebral body and the posterior surface of the lower vertebral body was measured. (B) The anterior-posterior diameter of the lower vertebral body was measured. A/B × 100(%) >25(%) or A >3 mm was defined as slippage.
Myelo-CT documentation of instability
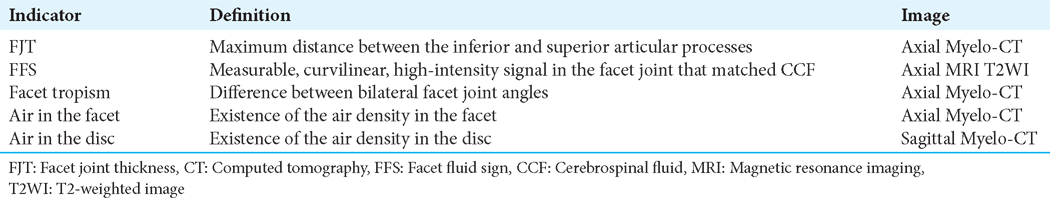
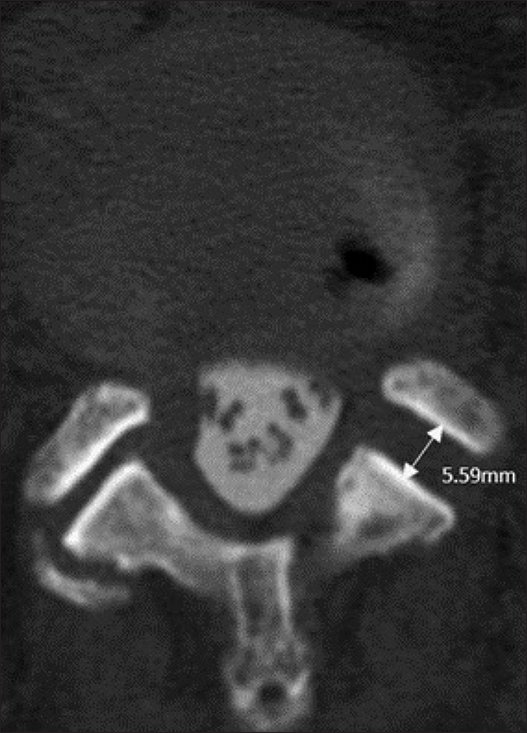
Myelo-CT criteria for lumbar instability included the assessment of FJT, FFS, facet tropism, air in the facet, and air in the disc [
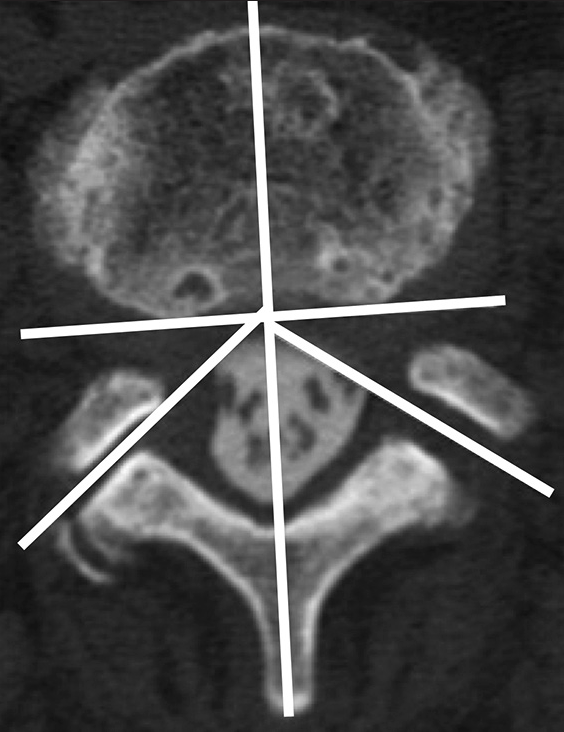
Figure 4:
Measurement of facet tropism. A line parallel to the posterior surface of the vertebral body was drawn, and a line perpendicular to this line and passing through the base of the spinous process was drawn. The angle between this line and facet was measured on the left and right, and the difference was taken as facet tropism.
Statistical analysis
Student’s t-test, Pearson’s Chi-square test and multivariate analysis with multiple logistic regression analysis were carried out. The level of significance was set at 5% (P ≤ 0.05), and all analyses were performed using SPSS, version 23.0 (IBM, Armonk, NY).
RESULTS
Neuroradiological indices
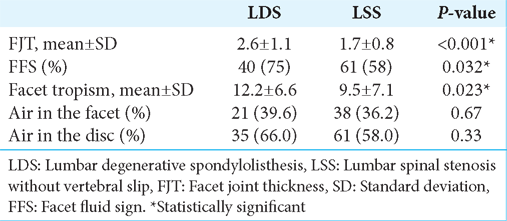
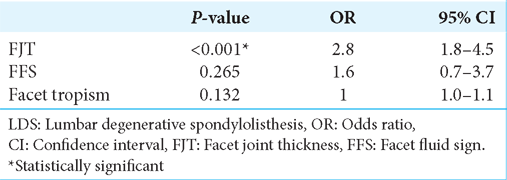
FJT was significantly elevated (2.6 ± 1.1 mm) in the LSD group versus the LSS group (1.7 ± 0.8 mm) [
DISCUSSION
FJT major myelo-CT indicator of lds instability warranting fusion
This study demonstrated that FJT was elevated especially in patients with LDS and was thus a crucial sign of dynamic vertebral instability and the need for fusion. Hasegawa et al. verified that an increased facet joint volume was associated with lumbar segmental instability.[
FSS additional myelo-CT finding for instability
FFS has become an important indicator of lumbar instability. Yamada et al. defined significant facet joint opening as >2 mm as (FJO); 70% of patients with FJO had FFS.[
Facet tropism consistent with instability
Facet tropism is indicative of degeneration within a facet joint and is also predominantly associated with the LSD group.[
Fusion rates
We performed decompression or fusion largely based on dynamic myelo-CT studies confirming significant instability (i.e., >3 mm or 25% olisthy) in LDS patients, while 97.3% of LSS patients without these findings underwent decompressions alone.
CONCLUSION
In patients with LDS, FJT on myelo-CT studies most specifically confirmed lumbar instability warranting fusion versus any other imaging parameter.
Ethical Approval
The author(s) declare that they have obtained ethical approval from IRB/IEC’ to ‘The authors declare that they have obtained ethical approval from our institution’s IRB’ in the Ethical Approval section.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Caterini R, Mancini F, Bisicchia S, Maglione P, Farsetti P. The correlation between exaggerated fluid in lumbar facet joints and degenerative spondylolisthesis: Prospective study of 52 patients. J Orthop Traumatol. 2011. 12: 87-91
2. Chaput C, Padon D, Rush J, Lenehan E, Rahm M. The significance of increased fluid signal on magnetic resonance imaging in lumbar facets in relationship to degenerative spondylolisthesis. Spine (Phila Pa 1976). 2007. 32: 1883-7
3. Cho BY, Murovic JA, Park J. Imaging correlation of the degree of degenerative L4-5 spondylolisthesis with the corresponding amount of facet fluid. J Neurosurg Spine. 2009. 11: 614-9
4. Gao T, Lai Q, Zhou S, Liu X, Liu Y, Zhan P. Correlation between facet tropism and lumbar degenerative disease: A retrospective analysis. BMC Musculoskelet Disord. 2017. 18: 483
5. Hasegawa K, Kitahara K, Shimoda H, Hara T. Facet joint opening in lumbar degenerative diseases indicating segmental instability. J Neurosurg Spine. 2010. 12: 687-93
6. Ko S, Chae S, Choi W, Kim JY, Kwon J, Doh J. The prevalence of facet tropism and its correlation with low back pain in selected community-based populations. Clin Orthop Surg. 2019. 11: 176-82
7. Yamada K, Toyoda H, Takahashi S, Tamai K, Suzuki A, Hoshino M. Facet joint opening on computed tomography is a predictor of poor clinical outcomes after minimally invasive decompression surgery for lumbar spinal stenosis. Spine (Phila Pa 1976). 2022. 47: 405-13
8. Yamada K, Toyoda H, Takahashi S, Tamai K, Suzuki A, Hoshino M. Relationship between facet joint opening on CT and facet joint effusion on MRI in patients with lumbar spinal stenosis: Analysis of a less invasive decompression procedure. J Neurosurg Spine. 2022. 36: 376-84