- Department of Functional Neurosurgery, Federal Center of Neurosurgery, Nemirovich-Danchenko 132/1,
- Department of Neuroscience, Institute of Medicine and Psychology, Novosibirsk State University, Pirogova,
- Department of Pathology, Novosibirsk State Medical University, Krasnyy Prospekt 52, Novosibirsk, Russia.
Correspondence Address:
Vidzhai Dzhafarov
Department of Pathology, Novosibirsk State Medical University, Krasnyy Prospekt 52, Novosibirsk, Russia.
DOI:10.25259/SNI_546_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vidzhai Dzhafarov, Jamil Rzaev, Galina Moysak, Eugenia Voronina. Facial pain as an initial manifestation of intramedullary cervical spinal cord tumor: A case report and literature review. 04-Jul-2020;11:173
How to cite this URL: Vidzhai Dzhafarov, Jamil Rzaev, Galina Moysak, Eugenia Voronina. Facial pain as an initial manifestation of intramedullary cervical spinal cord tumor: A case report and literature review. 04-Jul-2020;11:173. Available from: https://surgicalneurologyint.com/surgicalint-articles/10113/
Abstract
Background: Facial pain resembling trigeminal neuralgia is not a common clinical feature of cervical spinal cord tumor. Depending on nature of the facial pain, differential diagnosis tends to include neurovascular conflict, multiple sclerosis, cerebellopontine angle tumors, herpes zoster, facial injuries, and other conditions involving trigeminal nerve, ganglion, and root. Here, we present a unique case of pain in trigeminal distribution due to an intramedullary tumor in the upper cervical spinal cord.
Case Description: A 27-year-old male was admitted with complaints of intense facial pain on the right side lasting for several years. MRI revealed an intramedullary lesion at the C1 level and no signs of a neurovascular conflict or a demyelination. This lesion was removed microsurgically, with the subtotal resection immediately abolishing the pain and causing no additional neurological deficit. Histological analysis revealed ganglioglioma, Grade 1. After 5-day hospital stay, the patient was discharged home; 2-year follow-up showed no tumor recurrence on MRI and persistent relief of facial pain.
Conclusion: Secondary trigeminal neuralgia may be explained by a pathological process in vicinity of the spinal trigeminal nuclei. Removing the tumor may be expected to provide complete and lasting pain relief.
Keywords: Facial pain, Ganglioglioma, Intramedullary tumor, Secondary trigeminal neuralgia, Spinal cord tumor, Trigeminal neuralgia
INTRODUCTION
Surgical treatment of facial pain includes many kinds of procedures such as microvascular decompression (MVD), radiofrequency rhizotomy, percutaneous balloon compression, glycerol gangliolysis, stereotactic radiosurgery, trigeminal nucleotomy, motor cortex stimulation (MCS), and mass lesion resection.[
CASE DESCRIPTION
In 2017, a 27-year-old male patient presented to us with complaints of severe paroxysmal and continuous right- sided facial pain. He described his pain as a constant severe burning sensation with intermittent intensive lancinating (sharp) pain in the distribution of all three branches of the trigeminal nerve. This paroxysmal pain could be provoked by a light touch of the skin surface, chewing, and toothbrushing. This burning facial pain with short lasting episode of eyelid ptosis on the right side started in 2014 and later he also started experiencing severe paroxysmal pain that did not respond to oral carbamazepine but improved with pregabalin (75 mg). Over the years, the pain worsened and the medication dose had to be increased. In 2016, a Gamma Knife radiosurgery (90 Gy) was performed in another institution, targeting the right trigeminal nerve root, but no pain improvement was observed during subsequent 15 months. By that time, the patient was taking pregabalin (600 mg) with partial control of the pain. He suffered minor side effects but other anticonvulsants failed to produce any significant pain reduction. His had no history of any head or neck injuries, sinus or dental surgery, cancer, or any facial pain in his family. Neurological examination was normal except for allodynia, dysesthesia, and hyperpathia in the area of pain combined with symmetric slight increase in deep tendon reflexes. There were many paroxysmal pain trigger zones on the skin of the right side of the face. Pain intensity according to the numeric rating scale was 9 (other scalings were: BPI – 103, BNIPS – 5, and DN4 – 6). MRI examination detected an intramedullary lesion located at the upper cervical (C0-C1) level on the right side; there was no evidence of any neurovascular conflict or other relevant findings [
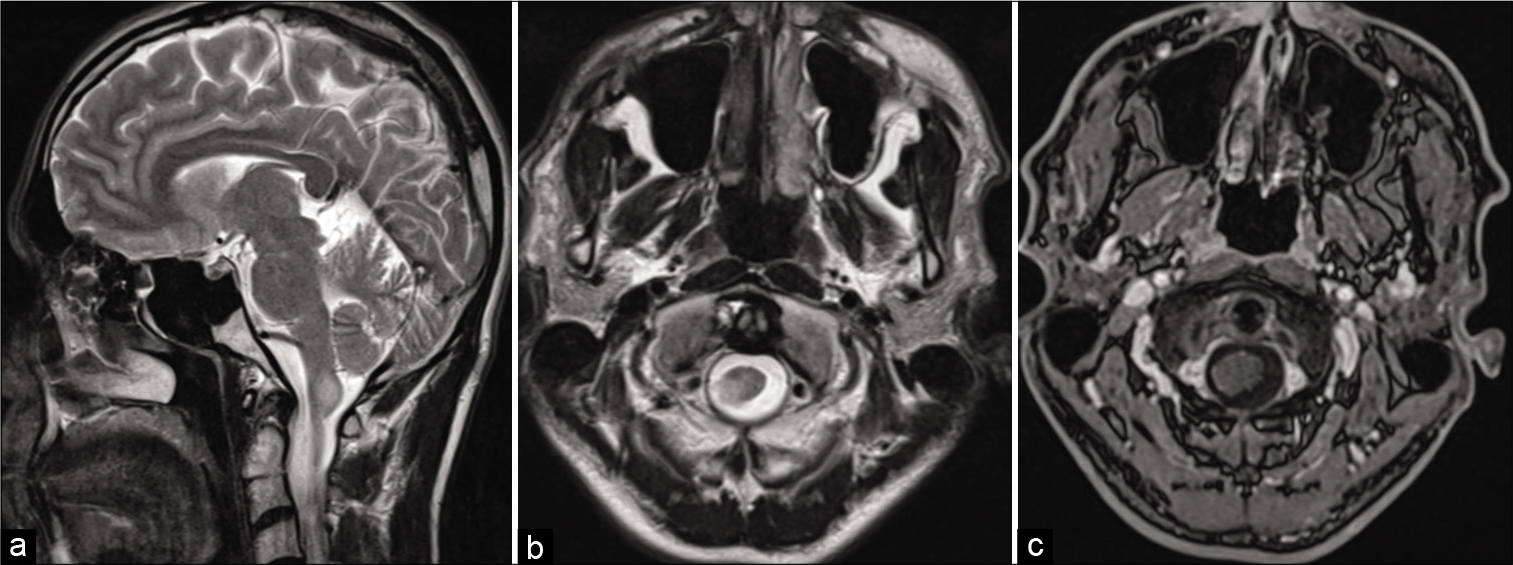
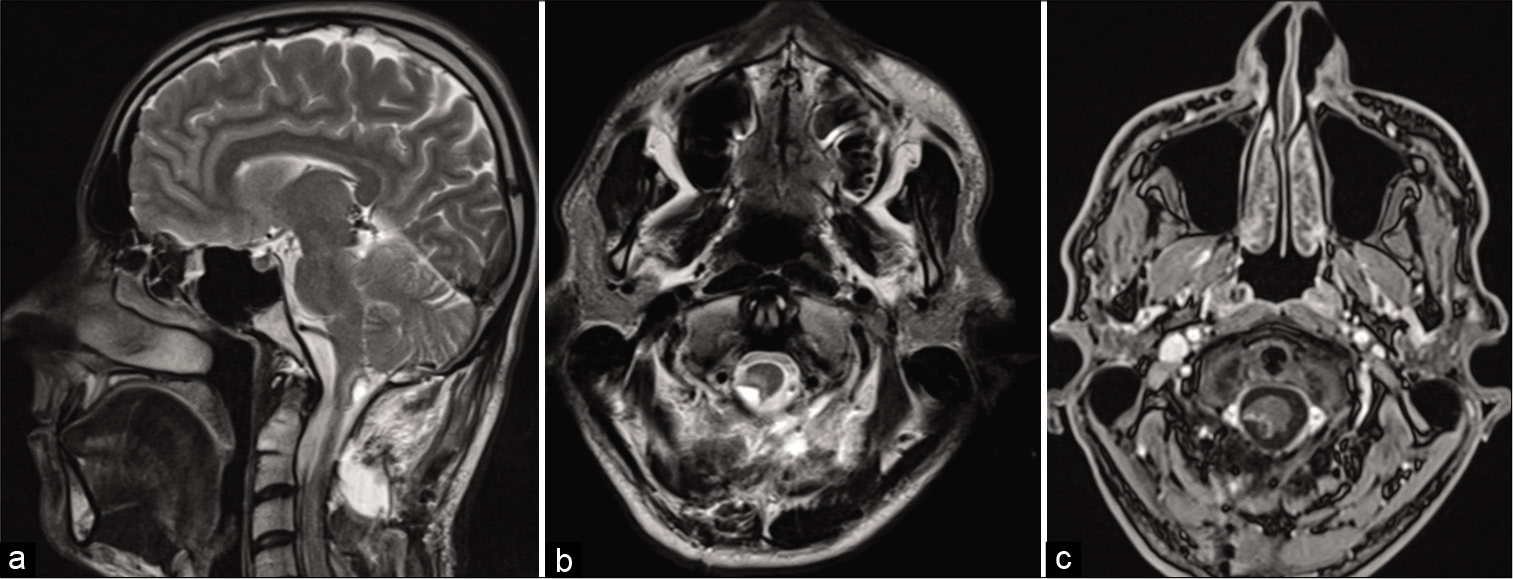
Figure 1:
Preoperative MRI. (a) T2-weighted image, sagittal plane. Tumor of 14 × 10 × 6 mm in size in the caudal dorsal medulla and upper cervical cord (hypertensive signal). (b) T2-weighted image, axial plane. The tumor on the right side of the medulla has similar characteristics. (c) Contrast enhancement axial T1. No contrast enhancement in this lesion.
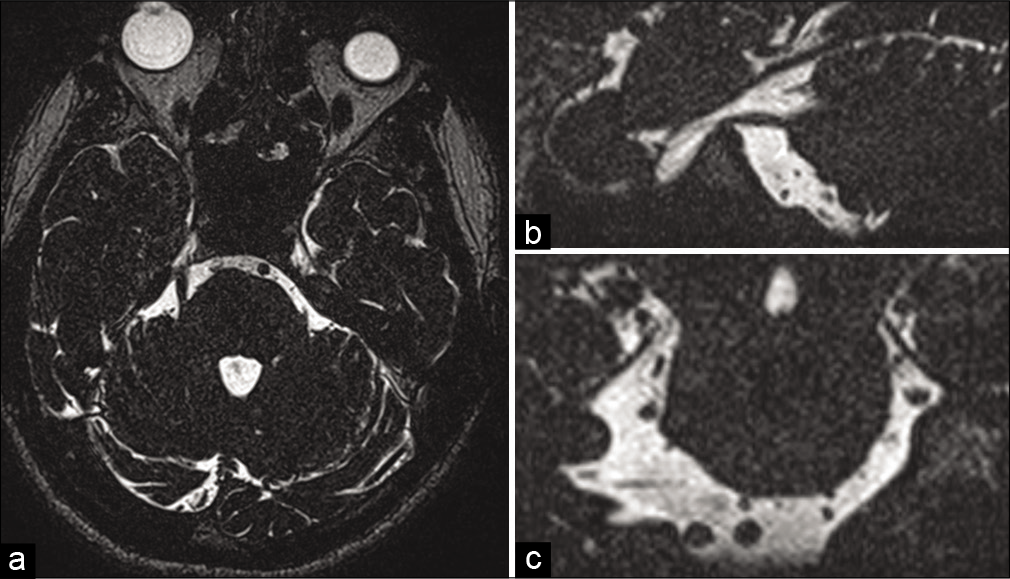
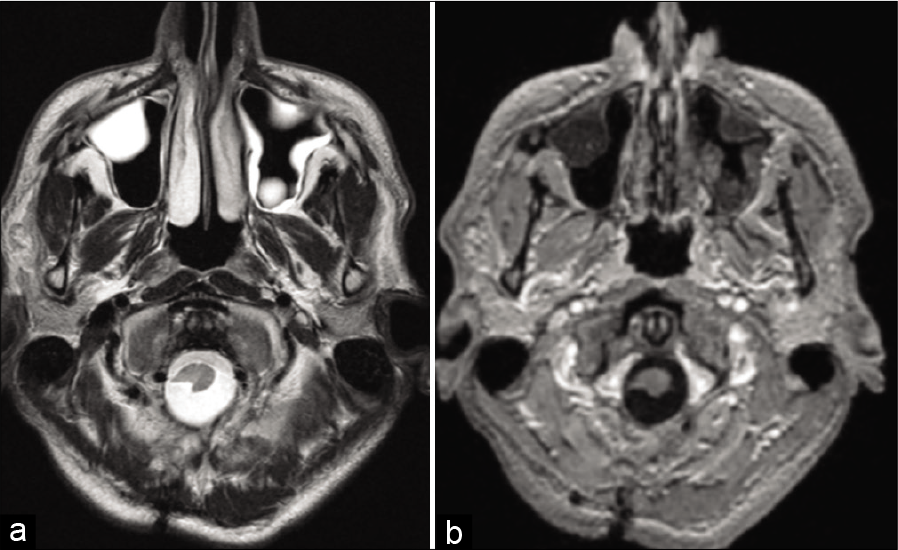
Figure 3:
Preoperative MRI at the level of the cisternal part of the trigeminal nerves. (a) T1 with contrast enhancement, axial plane. The focus of homogeneous enhancement is in the cisternal part of the root that related to the stereotaxic surgery procedure that affected that area. (b) DTI sequence. Anisotropy fraction is 463 at the TREZ level.
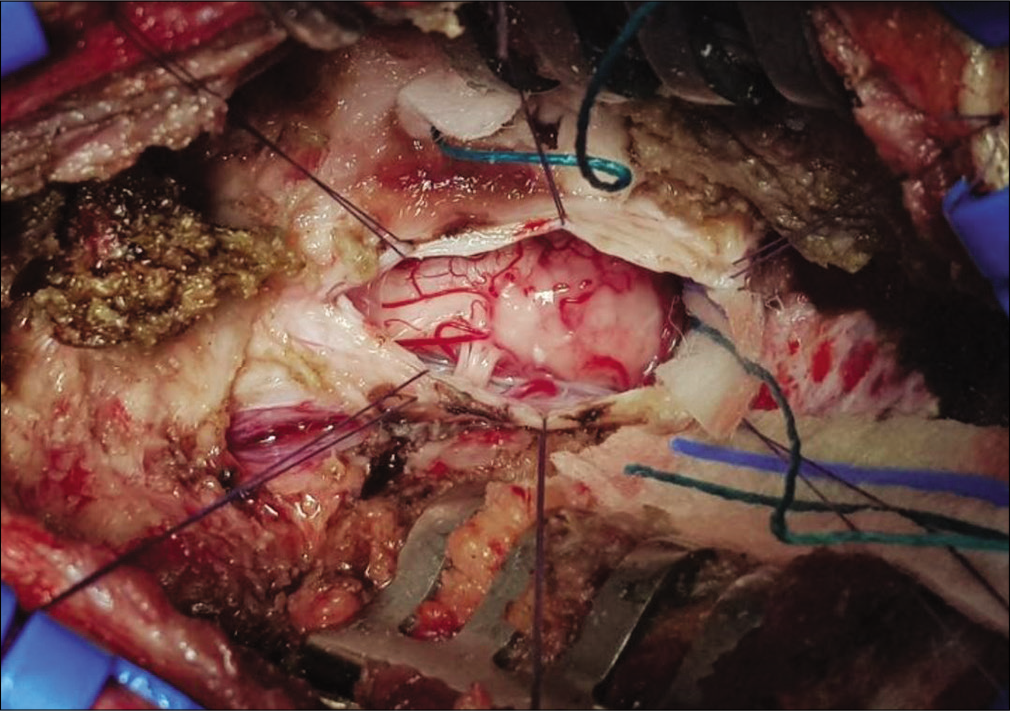
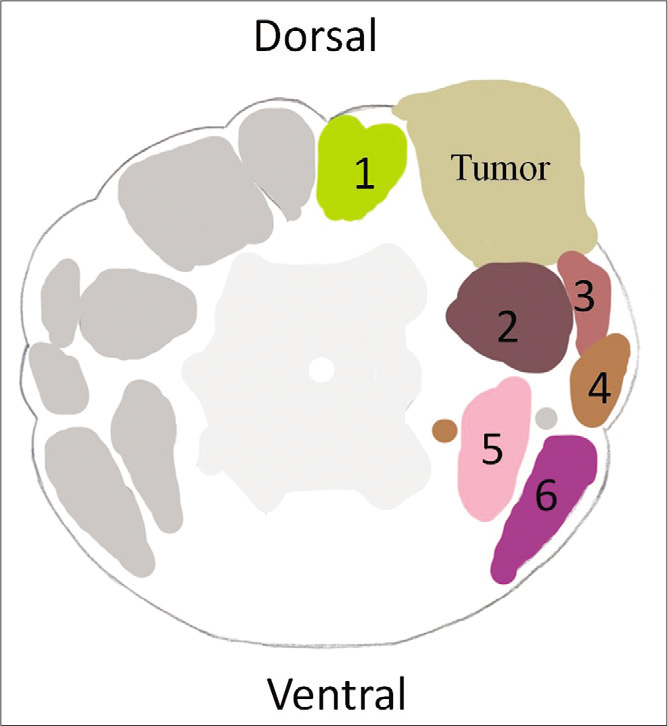
After ruling out other possible reasons for trigeminal pain, a decision was made to resect the lesion. In the operating room, C1 posterior arch resection in prone position under general anesthesia with neurophysiologic monitoring was performed by the senior author (JR). Intraoperatively, the tumor was tan in color without clear borders of separation it from the normal tissue [
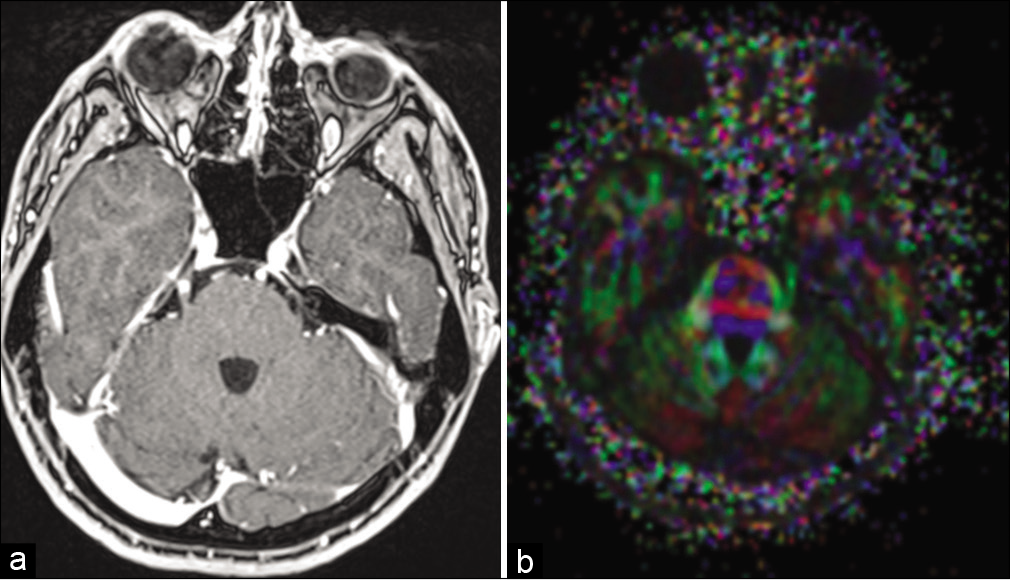
Figure 5:
Postoperative MRI. (a) T2-weighted image, sagittal plane. Postoperative cavity and perifocal edema of the medulla and spinal cord. Subcutaneous postoperative edema of the soft tissues. (b) T2-weighted image, axial plane. The mass was resected, the same postsurgical changes. (c) Contrast enhancement axial T1. A small amount of contrast enhancement presents in the surgical field.
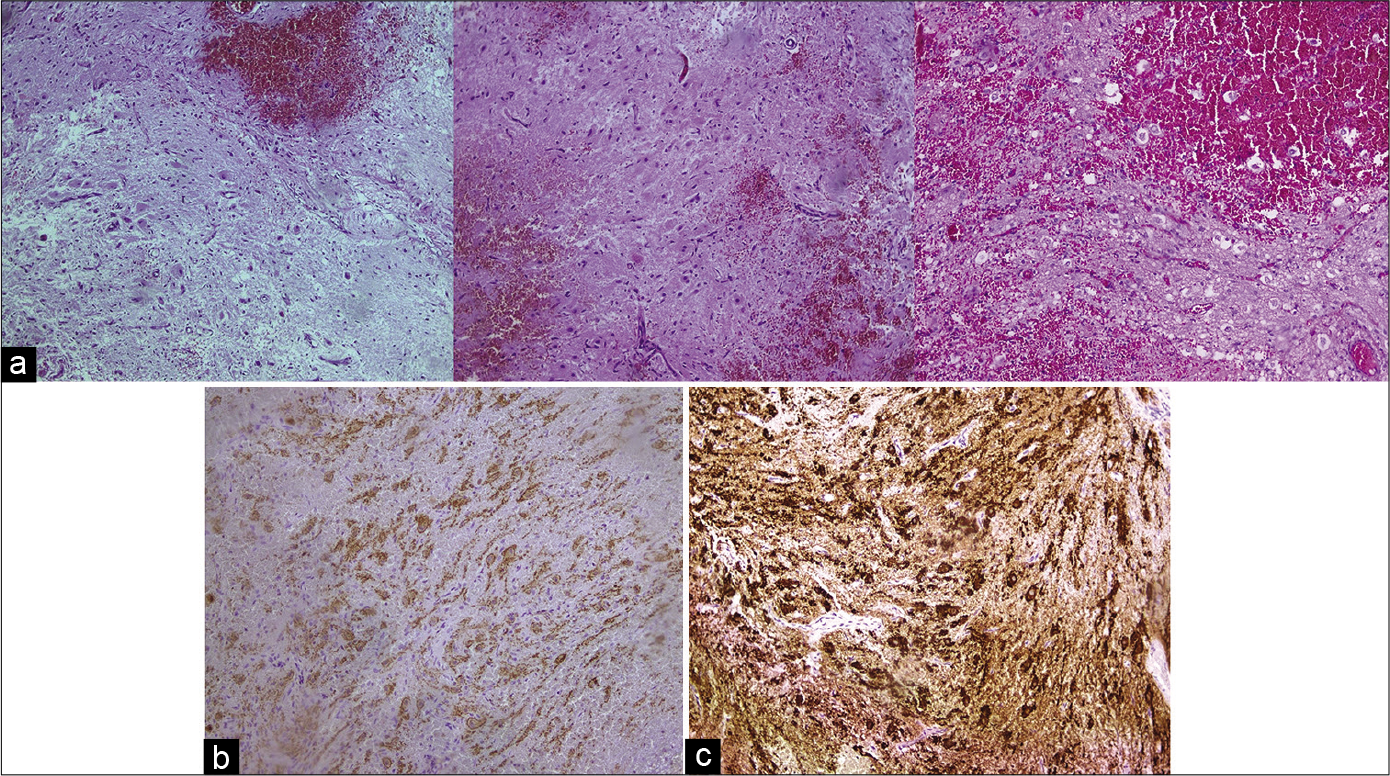
Figure 6:
Histological examination. (a) H&E staining of the tumor, ×100. The sample contains rare ovoid cells with well-shaped processes as well as the sings of edema single fibers and glia cells. The neurons are often separated in a diffuse way. (b) NeuN staining, ×100. Positive staining. (c) Synaptophysin staining, ×100. Positive staining.
DISCUSSION
In this paper, we describe an unusual manifestation of a spinal cord tumor. In our patient, the facial pain was the only clinical sign of the ganglioglioma located in the uppermost segment of the spinal cord presenting as combination of paroxysmal flash-like and burning constant pain in the entire distribution of the trigeminal nerve. In patients with trigeminal neuralgia and coexisting neurological signs or history of neurological deficit, the entire trigeminal pathway can be considered for proper detection of a pain generator. Searching for lesion along the entire trigeminal pathway enabled us to detect a possible pain generator and select a proper treatment.[
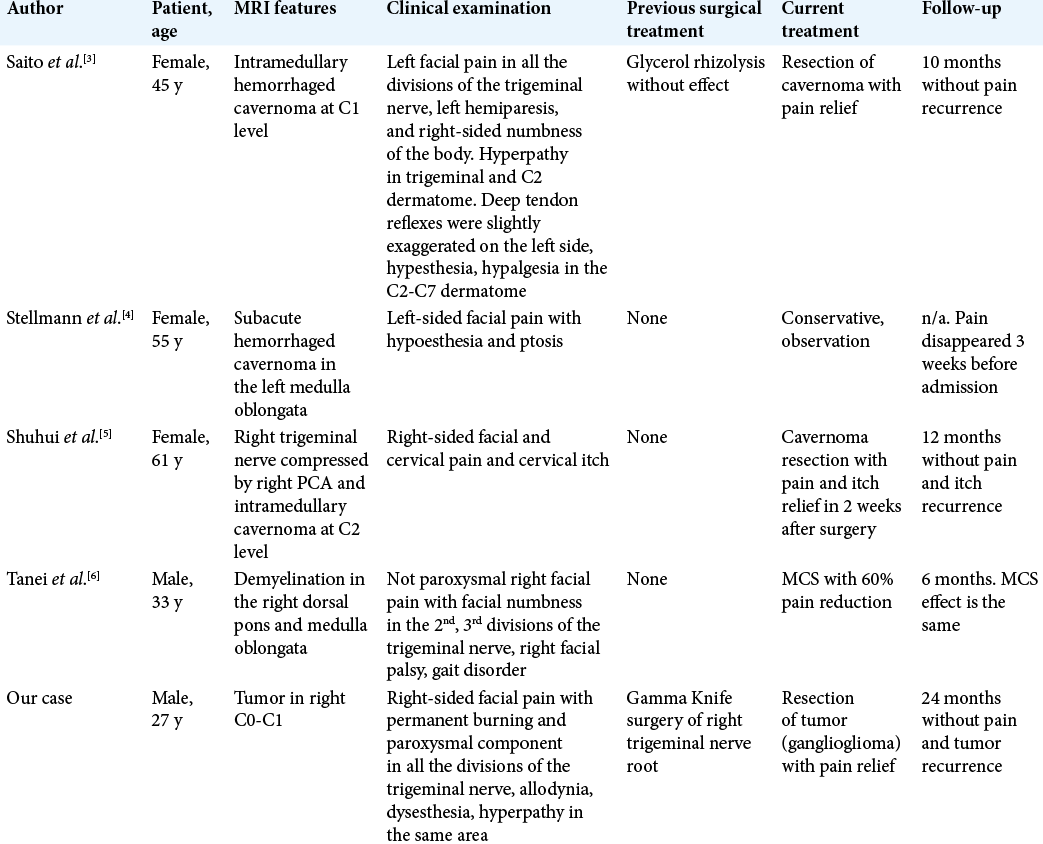
There have been several similar cases described in the literature [
Based on our experience, the management of the secondary trigeminal neuralgia associated with (or caused by) an upper cervical cord tumor should include resection of the tumor if possible. As an alternative treatment, one may consider stereotactic radiosurgery, but focusing radiation on trigeminal nerve root is unlikely to produce symptomatic improvement. Our patient underwent Gamma Knife radiosurgery of the trigeminal nerve root without any benefit, and the patient in another case[
CONCLUSION
Tumors of the upper cervical cord can manifest by ipsilateral facial pain. Resection of an intramedullary lesion in the upper cervical spinal cord can result in complete and permanent relief of the facial pain.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Graff-Radford S, Gordon R, Ganal J, Tetradis S. Trigeminal neuralgia and facial pain imaging. Curr Pain Headache Rep. 2015. 19: 19-
2. Saito N, Yamakawa K, Sasaki T, Saito I, Takakura K. Intramedullary cavernous angioma with trigeminal neuralgia: A case report and review of the literature. Neurosurgery. 1989. 25: 97-101
3. Shuhui G, Jiagang L, Siqing H, Haifeng C, Qingrong T, Bohao Z. Rare cervical intramedullary cavernous angioma with trigeminal neuralgia and cervical itch: Case report and review of the literature. Iran Red Crescent Med J. 2016. 18: e25151-
4. Slavin K, Nersesyan H, Colpan M, Munawar N. Current algorithm for the surgical treatment of facial pain. Head Face Med. 2007. 3: 30-
5. Stellmann J, Kuhn M, Töpper R. Therapieresistenter gesichtsschmerz durch ein hirnstammkavernom. Aktuelle Neurol. 2007. 75: 552-4
6. Tanei T, Kajita Y, Wakabayashi T. Motor cortex stimulation for intractable neuropathic facial pain related to multiple sclerosis. Neurol Med Chir (Tokyo). 2010. 50: 604-7