- Department of Spinal Surgery, Petrovsky National Research Centre of Surgery, Moscow, Russian Federation
- Department of Neurosurgery, Russian People’s Friendship University, United Nations Educational, Scientific and Cultural Organization (UNESCO), Digital Anatomy, Moscow, Russian Federation,
- Department of Neurosurgery, Liaquat National Hospital and Medical College, Karachi, Pakistan,
- Department of Neurosurgery, Azienda Ospedaliero Universitaria Pisana, University of Pisa, Pisa, Italy.
Correspondence Address:
Nicola Montemurro, Department of Neurosurgery, Azienda Ospedaliero Universitaria Pisana, University of Pisa, Pisa, Italy.
DOI:10.25259/SNI_659_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Renat Nurmukhametov1, Abakirov Medetbek1, Manuel Encarnacion Ramirez2, Afifa Afsar3, Salman Sharif3, Nicola Montemurro4. Factors affecting return to work following endoscopic lumbar foraminal stenosis surgery: A single-center series. 24-Nov-2023;14:408
How to cite this URL: Renat Nurmukhametov1, Abakirov Medetbek1, Manuel Encarnacion Ramirez2, Afifa Afsar3, Salman Sharif3, Nicola Montemurro4. Factors affecting return to work following endoscopic lumbar foraminal stenosis surgery: A single-center series. 24-Nov-2023;14:408. Available from: https://surgicalneurologyint.com/surgicalint-articles/12643/
Abstract
Background: This study evaluates the factors affecting the return to work of endoscopic surgery for lumbar foraminal stenosis (LFS), including symptoms, functional status, complications, and reoperation rates.
Methods: The authors’ retrospective cohort study included 100 consecutive patients (50 males and 50 females) diagnosed with LFS who underwent endoscopic surgery at Trotsky National Research Center of Surgery between January 2018 and December 2021.
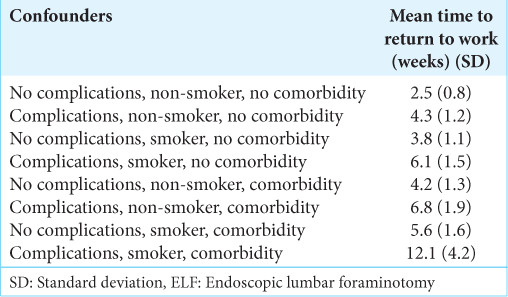
Results: There were no significant differences in age and preoperative visual analog scale and Oswestry disability index scores between the male and female groups, time to return to work for different patient groups after undergoing endoscopic lumbar foraminotomy (ELF). However, patients with more severe stenosis and comorbidities may take longer to recover. Confounding factors were patient age, preoperative physical function, and job requirements.
Conclusion: This study confirms that study ELF can effectively improve symptoms associated with lumbar radiculopathy, as well as back pain, and improve patients’ quality of life. Comorbidity, smoking status, and complications prolong the time to return to work following ELF surgery compared to healthy subjects.
Keywords: Clinical outcome, Endoscopic lumbar foraminotomy, Lumbar foraminal stenosis, Pain, Spine surgery
INTRODUCTION
Lumbar foraminal stenosis (LFS) is a common spinal disorder characterized by the narrowing of the neural foramen, causing compression of the exiting nerve root. LFS causes radicular and generalized back pain. Chronic low back pain, sciatica, and motor weakness may significantly affect patients’ quality of life. The traditional surgical approach for LFS is open decompression.
In recent years, endoscopic spine surgery has emerged as a minimally invasive alternative treatment for LFS. Endoscopic spine surgery involves using a small camera and specialized instruments inserted through a tiny incision, allowing the surgeon to visualize and access the affected area without extensive tissue disruption. This technique has been shown to have several advantages compared to open surgery, including reduced blood loss, shorter hospital stays, faster recovery, and lower morbidity rates.[
Endoscopic lumbar foraminotomy (ELF), as well as minimally invasive spinal surgery (MISS), led to the same endpoint of neural decompression when starting with more severe compression.[
Return to work is an essential indicator of the success of LFS surgery. Asher et al.[
MATERIALS AND METHODS
Study population
A retrospective analysis was performed on 100 consecutive patients consisting of 50 males and 50 females who underwent ELF for LFS at the Department of Spinal Surgery, Central Clinical Hospital of the Russian Academy of Sciences, between January 2018 and December 2021. The mean age was 48.2 years for males and 51.7 years for females.
Inclusion/exclusion criteria
Inclusion criteria are patients diagnosed with LFS confirmed by clinical and radiological examination, who underwent ELF, were over 18, and had a minimum follow-up of 12 months. Exclusion criteria were previous lumbar surgery, pregnancy, history of cancer or autoimmune disorders affecting the spine, concomitant central lumbar spinal stenosis, spondylolisthesis, and deformity. All surgeries were performed by the senior author (RN). The grade of LFS was graded and recorded according to Lee et al.[
Outcome measures
The primary outcome measures were the visual analog scale (VAS) score and the Oswestry disability index (ODI) score.[
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the Department of Spinal Surgery, Petrovsky National Research Center of Surgery, Moscow, Russia. Informed consent was obtained from all patients before surgery. Patient confidentiality was always maintained, and the data were anonymized during analysis and reporting.
Surgical technique
Under general or regional anesthesia, a small incision on the patient’s back to access the lumbar neuroforamen through the transforaminal approach. The endoscopic working cannula is inserted over sequential tubular dilators. A foraminal endoscope is used to visualize the compression pathology directly. The decompression is done with a motorized drill or Kerrison rongeurs. These endoscopic instruments are placed through the endoscope’s central working channel. The skin incision is closed with stitches or surgical glue. The patient is taken to a recovery area, where they are monitored until comfortable, able to ambulate, and void before being sent home from the recovery room.
Statistical analysis
Descriptive statistics were used to summarize the patient demographics, clinical presentation, and radiological findings. The pre-and postoperative VAS and ODI scores were analyzed with a paired T-test. Statistical analysis was performed using SPSS version 26.
RESULTS
Based on the sagittal MRI, Lee et al.[
The mean preoperative VAS score was 7.9 ± 1.5 for male and 8.1 ± 1.4 for female patients. The corresponding postoperative numbers were 2.4 ± 1.4 versus 2.6 ± 1.5, respectively. The mean preoperative ODI score for males was 58.3 ± 12.9 versus females 60.7 ± 14.6. The respective postoperative ODI scores were 19.5 ± 9.3 and 21.1 ± 10.1. There were no statistically significant differences between female and male patients between pre- and postoperative VAS and ODI numbers. However, the VAS and ODI score improvements were statistically significant (P = 0.021). Overall, surgical complications resulted in 6% of cases. There was one dural tear, postoperative hematoma, and nerve root injury. The reoperation rate in patients with LFS who underwent ELF was 4%. The mean time between first surgery and reoperation was 7.6 ± 3.4 months. The mean time to return to work following surgery was 2.5 weeks in patients without complications. In patients with complications, it was 4.3 weeks [
DISCUSSION
Surgical management of lumbar pathology has been proven to effectively improve patients’ function and allow them to return to work. However, around 25% of the surgically managed spine patients report minimal improvement in quality of life, and up to 10% experience a major complication or hospital readmission post-surgery.[
Our results corroborate findings reported by others, indicating that ELF is effective in treating LFS, with a low complication and reoperation rate. Lewandrowski[
However, patients with more severe stenosis and comorbidities may have longer recovery times. Further studies with larger sample sizes and longer follow-up periods are needed to confirm these findings. This is in line with previous research that has shown that the degree of stenosis is a key predictor of surgical outcomes in patients with LFS.[
A recent clinical study [
Findings showed relatively consistently that a lower level of education, a higher level of preoperative pain, less work satisfaction, a longer duration of sick leave, higher levels of psychological complaints, and more passive avoidance coping function as predictors of an unfavorable outcome in terms of pain, disability, work capacity, or a combination of these outcome measures.[
CONCLUSION
ELF is a surgical technique for the treatment of LFS. The author’s study suggests that ELF can effectively improve symptoms associated with lumbar radiculopathy, as well as back pain, and improve patients’ quality of life. Comorbidity, smoking status, and complications prolong the time to return to work following ELF surgery compared to healthy subjects. However, more prospective and randomized studies about patients treated with ELF for LFS are needed.
Ethical approval
The author(s) declare that they have taken the ethical approval from IRB of Department of Spinal Surgery, Petrovsky National Research Centre of Surgery, Moscow, Russia (10/21). Approval number is 10/2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
We thank Prof Jesus Lafuente Barza, Prof Matias Baldoncini, Dr. Ismael Peralta Baez, Dr. Medet Dosanov, and Dr Kai-Uwe Lewandrowski for their scientific support.
References
1. Ahn Y, Lee SH, Park WM, Lee HY. Posterolateral percutaneous endoscopic lumbar foraminotomy for L5-S1 foraminal or lateral exit zone stenosis. Technical note. J Neurosurg. 2003. 99: 320-3
2. Ahn Y, Oh HK, Kim H, Lee SH, Lee HN. Percutaneous endoscopic lumbar foraminotomy: An advanced surgical technique and clinical outcomes. Neurosurgery. 2014. 75: 124-33
3. Ahsan K, Khan SI, Zaman N, Ahmed N, Montemurro N, Chaurasia B. Fusion versus nonfusion treatment for recurrent lumbar disc herniation. J Craniovertebr Junction Spine. 2021. 12: 44-53
4. Ahsan MK, Hossain MR, Khan MS, Zaman N, Ahmed N, Montemurro N. Lumbar revision microdiscectomy in patients with recurrent lumbar disc herniation: A single-center prospective series. Surg Neurol Int. 2020. 11: 404
5. Anderson JT, Tye EY, Haas AR, Percy R, Woods ST, Ahn UM. Multilevel lumbar fusion is a risk factor for lower return to work rates among workers’ compensation subjects with degenerative disc disease. J Surg Orthop Adv. 2018. 27: 209-18
6. Asher AL, Devin CJ, Archer KR, Chotai S, Parker SL, Bydon M. An analysis from the Quality Outcomes Database, Part 2. Predictive model for return to work after elective surgery for lumbar degenerative disease. J Neurosurg Spine. 2017. 27: 370-81
7. Burman MS. Myeloscopy or the direct visualization of the spinal canal and its contents. J Bone Joint Surg. 1931. 13: 695-6
8. Chang SB, Lee SH, Ahn Y, Kim JM. Risk factor for unsatisfactory outcome after lumbar foraminal and far lateral microdecompression. Spine. 2006. 31: 1163-7
9. Chen T, Zhou G, Chen Z, Yao X, Liu D. Biportal endoscopic decompression vs. microscopic decompression for lumbar canal stenosis: A systematic review and meta-analysis. Exp Ther Med. 2020. 20: 2743-51
10. Choi WS, Kim JS, Hur JW, Song JH, Kim KT. Endoscopic spinal surgery for lumbar spinal stenosis: A systematic review and meta-analysis. Eur Spine J. 2019. 28: 2522-32
11. Chou R, Shekelle P. Will this patient develop persistent disabling low back pain?. JAMA. 2010. 303: 1295-302
12. den Boer JJ, Oostendorp RA, Beems T, Munneke M, Oerlemans M, Evers AW. A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J. 2006. 15: 527-36
13. Encarnacion Ramirez MJ, Barrientos Castillo RE, Nurmukhametov R, Dosanov M, Tolokonnikov N, Bernard E. Microsurgical wiltse paraspinal approach using a low-budget exoscope. Cureus. 2022. 14: e25858
14. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980. 66: 271-3
15. Giordan E, Billeci D, Del Verme J, Varrassi G, Coluzzi F. Endoscopic transforaminal lumbar foraminotomy: A systematic review and meta-analysis. Pain Ther. 2021. 10: 1481-95
16. Haufe SM, Mork AR, Pyne MA, Baker RA. Endoscopic laminoforaminoplasty success rates for treatment of foraminal spinal stenosis: Report on sixty-four cases. Int J Med Sci. 2009. 6: 102-5
17. Hennemann S, de Abreu MR. Degenerative lumbar spinal stenosis. Rev Bras Ortop (Sao Paulo). 2021. 56: 9-17
18. Hersht M, Massicotte EM, Bernstein M. Patient satisfaction with outpatient lumbar microsurgical discectomy: A qualitative study. Can J Surg. 2007. 50: 445-9
19. Hijikata S. Percutaneous nucleotomy: A new treatment method for lumbar disc herniation. J Toden Hosp. 1975. 1: 713-5
20. Houra K, Saftic R, Klaric E, Knight M. Long-term clinical outcomes following endoscopic foraminoplasty for patients with single-level foraminal stenosis of the lumbar spine. Int J Spine Surg. 2022. 16: 139-50
21. Hsu HT, Chang SJ, Yang SS, Chai CL. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J. 2013. 22: 727-33
22. Huysmans E, Goudman L, Van Belleghem G, De Jaeger M, Moens M, Nijs J. Return to work following surgery for lumbar radiculopathy: A systematic review. Spine J. 2018. 18: 1694-714
23. Iyer S, Bovonratwet P, Samartzis D, Schoenfeld AJ, An HS, Awwad W. Appropriate telemedicine utilization in spine surgery: Results from a Delphi study. Spine (Phila Pa 1976). 2022. 47: 583-90
24. Kambin P, editors. Posterolateral percutaneous lumbar discectomy and decompression. Arthroscopic micro-discectomy: Minimal intervention in spinal surgery. United States: Williams & Wilkins; 1991. 8: 287-95
25. Khan I, Bydon M, Archer KR, Sivaganesan A, Asher AM, Alvi MA. Impact of occupational characteristics on return to work for employed patients after elective lumbar spine surgery. Spine J. 2019. 19: 1969-76
26. Kim JE, Choi DJ. Biportal endoscopic transforaminal lumbar interbody fusion with arthroscopy. Clin Orthop Surg. 2018. 10: 248-52
27. Kim JM, Lee SH, Ahn Y, Yoon DH, Lee CD, Lim ST. Recurrence after successful percutaneous endoscopic lumbar discectomy. Minim Invasive Neurosurg. 2007. 50: 82-5
28. Kim JY, Kim HS, Jeon JB, Lee JH, Park JH, Jang IT. The novel technique of uniportal endoscopic interlaminar contralateral approach for coexisting L5-S1 lateral recess, foraminal, and extraforaminal stenosis and its clinical outcomes. J Clin Med. 2021. 10: 1364
29. Kim M, Lee S, Kim HS, Park S, Shim SY, Lim DJ. A comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for lumbar disc herniation in the Korean: A meta-analysis. Biomed Res Int. 2018. 2018: 9073460
30. Laasik R, Lankinen P, Kivimäki M, Neva MH, Aalto V, Oksanen T. Return to work after lumbar disc herniation surgery: An occupational cohort study. Acta Ortho. 2021. 92: 638-43
31. Lee DY, Shim CS, Ahn Y, Choi YG, Kim HJ, Lee SH. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for recurrent disc herniation. J Korean Neurosurg Soc. 2009. 46: 515-21
32. Lee S, Lee JW, Yeom JS, Kim KJ, Kim HJ, Chung SK. A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol. 2010. 194: 1095-8
33. Lewandrowski KU. “Outside-in” technique, clinical results, and indications with transforaminal lumbar endoscopic surgery: A retrospective study on 220 patients on applied radiographic classification of foraminal spinal stenosis. Int J Spine Surg. 2014. 8: 26
34. Lewandrowski KU. Readmissions after outpatient transforaminal decompression for lumbar foraminal and lateral recess stenosis. Int J Spine Surg. 2018. 12: 342-51
35. Lewandrowski KU, Ransom NA, Yeung A. Return to work and recovery time analysis after outpatient endoscopic lumbar transforaminal decompression surgery. J Spine Surg. 2020. 6: S100-15
36. Liu Y, Van Isseldyk F, Kotheeranurak V, Quillo-Olvera J, Bae J, Choi KC. Transforaminal endoscopic decompression for foraminal stenosis: Single-arm meta-analysis and systematic review. World Neurosurg. 2022. 168: 381-91
37. Montemurro N. Telemedicine: Could it represent a new problem for spine surgeons to solve?. Global Spine J. 2022. 12: 1306-7
38. Nurmukhametov R, Dosanov M, Encarnacion MJ, Barriento R, Matos Y, Alyokhin AI. Transforaminal fusion using physiologically integrated titanium cages with a novel design in patients with degenerative spinal disorders: A pilot study. Surgeries. 2022. 3: 175-84
39. Parker SL, Lerner J, McGirt MJ. Effect of minimally invasive technique on return to work and narcotic use following transforaminal lumbar inter-body fusion: A review. Prof Case Manag. 2012. 17: 229-35
40. Patel K, Harikar MM, Venkataram T, Chavda V, Montemurro N, Assefi M. Is minimally invasive spinal surgery (MISS) superior to endoscopic spine surgery in postoperative radiological outcome for lumbar spine degenerative disease? A systematic review. J Neurol Surg A Cent Eur Neurosurg. 2023. 1: 1
41. Ramirez ME, Peralta I, Nurmukhametov R, Castillo RE, Castrox JS, Volovich A. Expanding access to microneurosurgery in low-resource settings: Feasibility of a low-cost exoscope in transforaminal lumbar interbody fusion. J Neurosci Rural Pract. 2023. 14: 156-60
42. Ramirez MJ, Nurmukhametov R, Bernard E, Peralta I, Efe IE. A low-cost three-dimensional printed retractor for transforaminal lumbar interbody fusion. Cureus. 2022. 14: e24185
43. Rosen DS, O’Toole JE, Eichholz KM, Hrubes M, Huo D, Sandhu FA. Minimally invasive lumbar spinal decompression in the elderly: Outcomes of 50 patients aged 75 years and older. Neurosurgery. 2007. 60: 503-9
44. Ruetten S, Komp M, Merk H, Godolias G. Recurrent lumbar disc herniation after conventional discectomy: A prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech. 2009. 22: 122-9
45. Siepe CJ, Sauer D, Michael Mayer H. Full endoscopic, bilateral over-the-top decompression for lumbar spinal stenosis. Eur Spine J. 2018. 27: 563-5
46. Srinivas S, Paquet J, Bailey C, Nataraj A, Stratton A, Johnson M. Effect of spinal decompression on back pain in lumbar spinal stenosis: A Canadian Spine Outcomes Research Network (CSORN) study. Spine J. 2019. 19: 1001-8
47. Tang K, Goldman S, Avrumova F, Lebl DR. Background, techniques, applications, current trends, and future directions of minimally invasive endoscopic spine surgery: A review of literature. World J Orthop. 2023. 14: 197-206
48. Vanegas Cerna G, Barrientos Castillo RE, Nurmukhametov R, Baldoncini M, López Lara CE, Rosario A. Giant invasive intradural extramedullary lumbar schwannoma: A case report and literature review. Cureus. 2023. 15: e40708
49. Yang Y, Liu ZY, Zhang LM, Pang M, Chhantyal K, Wu WB. Microendoscopy-assisted minimally invasive versus open transforaminal lumbar interbody fusion for lumbar degenerative diseases: 5-year outcomes. World Neurosurg. 2018. 116: e602-10
50. Youn MS, Shin JK, Goh TS, Lee JS. Predictors of clinical outcome after endoscopic partial facetectomy for degenerative lumbar foraminal stenosis. World Neurosurg. 2019. 126: e1482-8