Failure of tandem flow diversion for intracranial aneurysms: Literature review and illustrative case
- Department of Neurosurgery, University of Baghdad, College of Medicine, Al Risafa, Baghdad, Iraq,
- Department of Neurosurgery, University of Alameed, College of Medicine, Karbala, Iraq,
- Department of Neurosurgery, University of Misan, College of Medicine, Amarah, Iraq,
- Department of Neurosurgery, Tokyo General Hospital, Tokyo, Japan,
- Department of Neurosurgery, University of Wisconsin-Madison, Wisconsin, United States,
- Department of Neurosurgery, Imam Abdulrahman Alfaisal University, Dammam, Saudi Arabia,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
DOI:10.25259/SNI_944_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Teeba A. Al-Ageely1, Mustafa Ismail1, Sara A. Mohammed1, Ali H. Al-Delfi2, Muhammed S. Alshedidi2, Mohammed B. Al-Jaberi3, Muntadher H. Almufadhal1, Awfa Aktham Abdulateef4, Zaid Aljuboori5, Hosam Al-Jehani6, Samer S. Hoz7. Failure of tandem flow diversion for intracranial aneurysms: Literature review and illustrative case. 11-Nov-2022;13:518
How to cite this URL: Teeba A. Al-Ageely1, Mustafa Ismail1, Sara A. Mohammed1, Ali H. Al-Delfi2, Muhammed S. Alshedidi2, Mohammed B. Al-Jaberi3, Muntadher H. Almufadhal1, Awfa Aktham Abdulateef4, Zaid Aljuboori5, Hosam Al-Jehani6, Samer S. Hoz7. Failure of tandem flow diversion for intracranial aneurysms: Literature review and illustrative case. 11-Nov-2022;13:518. Available from: https://surgicalneurologyint.com/surgicalint-articles/11998/
Abstract
Background: Flow diverters are becoming one of the main endovascular procedures used to treat aneurysms. Flow diverter devices (FDDs) have multiple types approved for endovascular procedure use. Although their indications are not well described, they are usually used for large or giant, wide-necked, and recurrent aneurysms. Multiple FDDs can be deployed to treat giant aneurysms to ensure and accelerate aneurysm occlusion and mitigate complications. We report a case of endovascular treatment of an intracranial aneurysm using three silk FDDs complicated by a delayed migration of the stents along the parent artery, along with a literature review of the related cases.
Methods: We conducted a PubMed Medline database search by the following combined formula of subjects headings: ((((((intracranial aneurysm[MeSH Terms]) AND (endovascular procedure[MeSH Terms])) OR (endovascular technique[MeSH Terms])) AND (endovascular[Title/Abstract]) AND (Flow diverter[Title/ Abstract])) OR (flow diversion[Title/Abstract])) OR (Pipeline[Title/Abstract])) AND (Multiple[Title/Abstract]).
Results: The result was eight cases of endovascular treatment of intracranial aneurysms with multiple FDD. The male-to-female ratio in these cases was 5:3, and there is a wide age range from 22 months to 69 years old. The cases differed in the type and number of FDDs used, yet, they all had similar results with aneurysm occlusion and recovery of the patient with no observed complications.
Conclusion: Tandem flow diverter deployment has technical challenges and complications such as complete obstruction can occur. Planning and learning from experience with those new technologies are the typical way to overcome such complications in the future.
Keywords: Flow diverter devices, Intracranial aneurysms, Stent migration
INTRODUCTION
Flow diverter devices (FDDs) are relatively novel generation stents used in endovascular procedures to manage intracranial aneurysms.[
There are five types of flow diverters currently approved for the treatment of intracranial aneurysms. These include Pipeline Embolization Device (PED), Silk, Flow Redirection Endoluminal Device (FRED), p64 Flow Modulation Device, and the Surpass Flow Diverter.[
Here, we report a case of a delayed migration of three Silk flow diverter stents, leading to severe stenosis of the right cervical internal carotid artery (ICA). We explain the intricacies of FDDs and their complications, including delayed migration in the parent vessel. We have conducted a brief literature review of the published intracranial aneurysm cases managed with two or more FDDs, along with their outcomes.
CASE REPORT
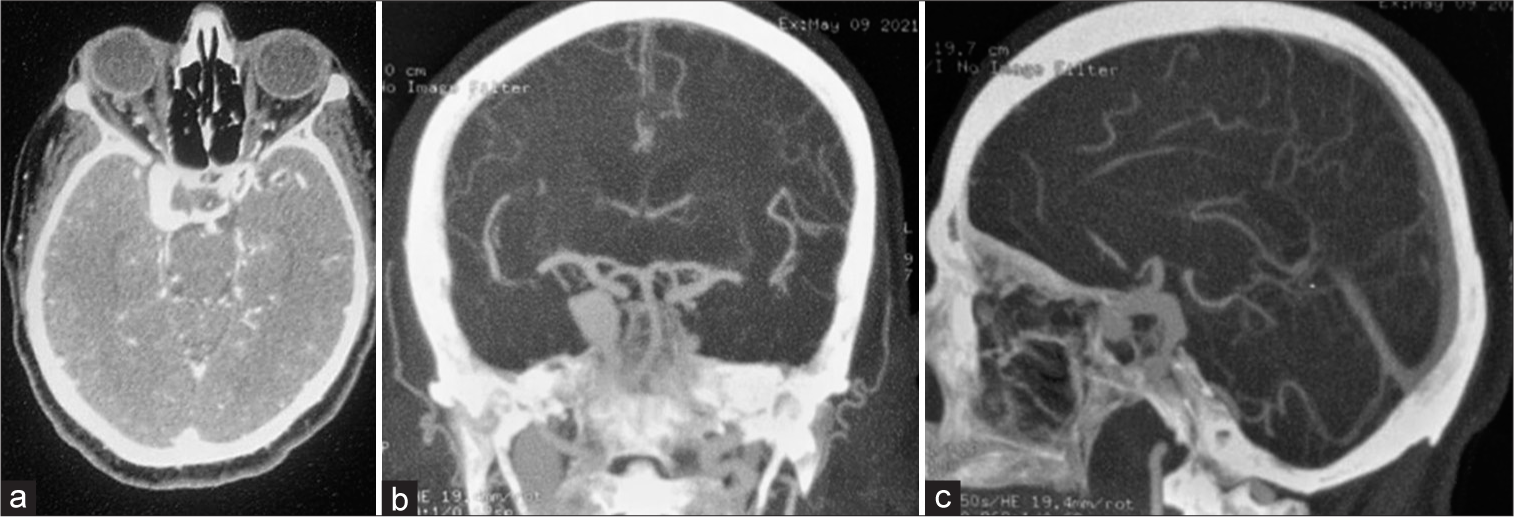
A 71-year-old female presented with the right eye ptosis and severe headache, with preserved vision. Computed tomography (CT) scan was done and it showed a subarachnoid hemorrhage in the basal cistern. In addition, CT angiography and magnetic resonance imaging were performed for the patient, and they revealed a giant aneurysm in the right ICA proximal to its bifurcation, with no evidence of the previous rupture [
Figure 1:
(a) Contrast-enhanced computed tomography scan axial section is revealing a large enhancing lesion in the right internal carotid artery (ICA). (b) Computed tomographic angiography (CTA) coronal section is showing a right-sided large vascular lesion in the right ICA in its proximal segment before its bifurcation. (c) CTA sagittal section is showing a right-sided large vascular lesion in the right ICA in its proximal segment before its bifurcation.
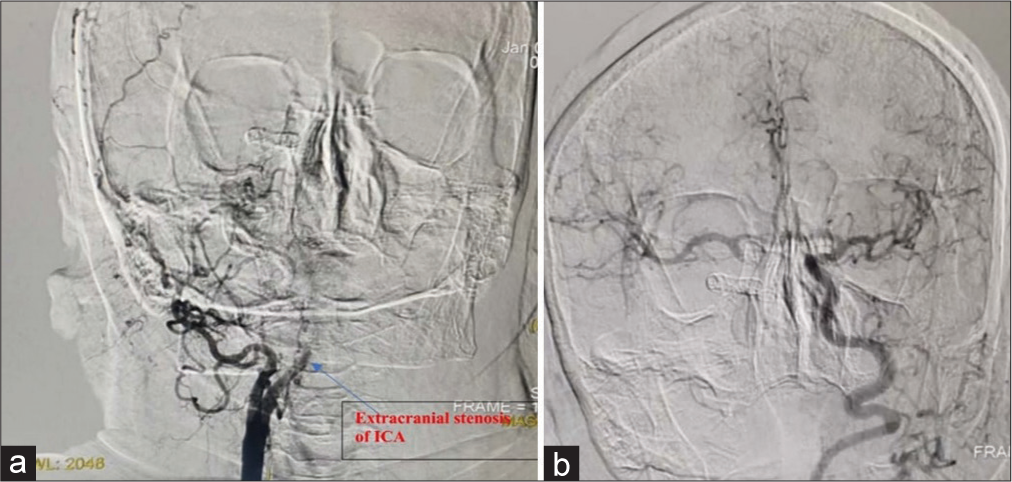
The patient underwent diagnostic catheter angiography, which revealed a fusiform, thrombosed, and dissecting aneurysm in the cavernous segment of the right ICA, the dome width of 10.3 mm, and the dome height was 19.8 mm. The width of the proximal segment of the aneurysm was 4.7 mm [
Due to the aneurysm’s size and location, the decision for an endovascular approach using three sequential tandem SILK flow diverting stents was the most appropriate treatment for the case. The result of the stenting showed a significant reduction in blood flow within the aneurysm and an improvement in the patient’s symptoms [
Six months later, the patient developed recurrent attacks of severe headache. She underwent diagnostic catheter angiography, which revealed severe stenosis of the cervical right ICA with intracranial obstruction, which was then known to be due to proximal migration of the stents inside the ICA with no recurrence of the aneurysm. The collateral blood flow showed sufficient compensation for the stenosed segment of the right ICA; therefore, the patient was started on conservative treatment along with monitoring and follow-up [
LITERATURE REVIEW
Methods
We conducted a PubMed Medline database search by the following combined formula of subjects headings: ((((((intracranial aneurysm[MeSH Terms]) AND (endovascular procedure[MeSH Terms])) OR (endovascular technique[MeSH Terms])) AND (endovascular[Title/ Abstract]) AND (Flow diverter[Title/Abstract])) OR (flow diversion[Title/Abstract])) OR (Pipeline[Title/Abstract])) AND (Multiple[Title/Abstract]). The reference list of the included papers was screened for additional sources.
RESULTS
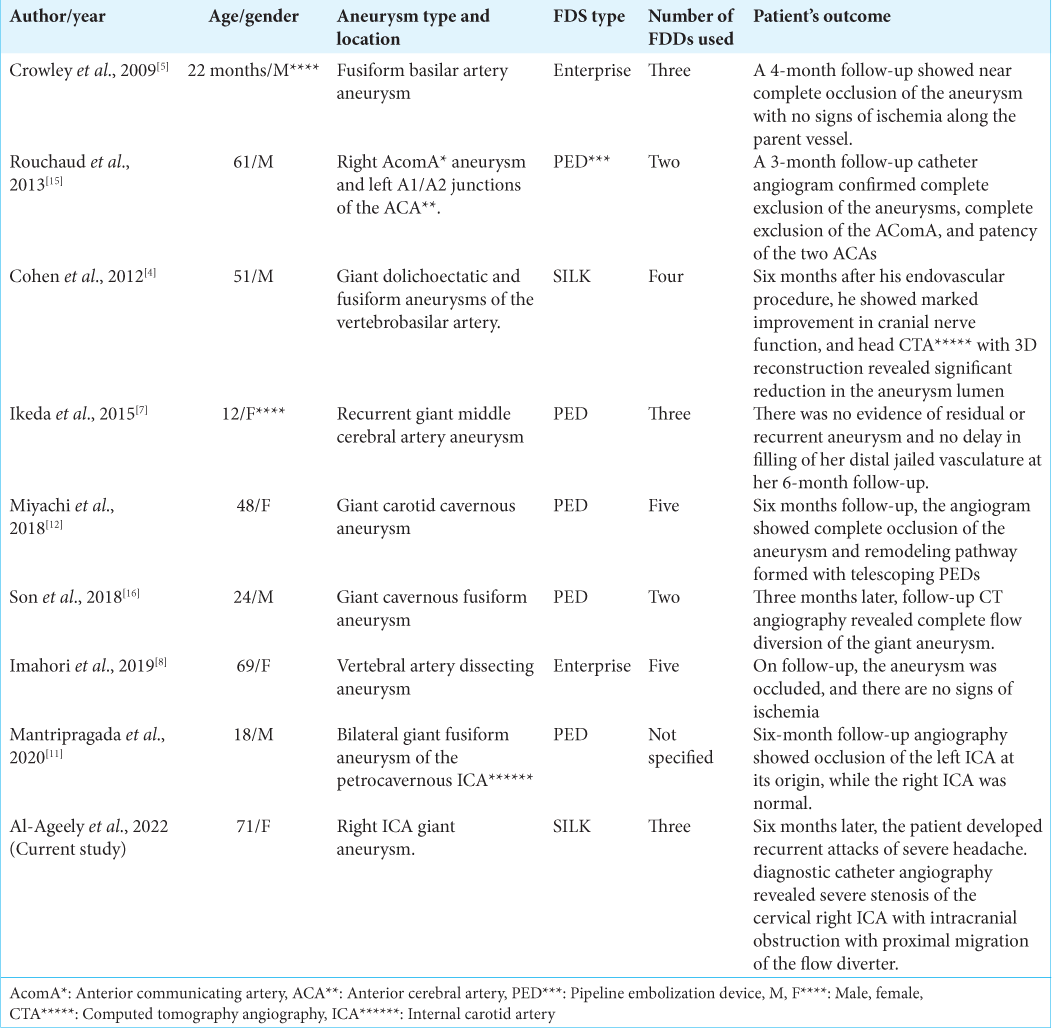
A total of 66 case reports were found. By excluding cases in which only a single FDD was deployed, only eight cases remained in which an intracranial aneurysm was treated by an endovascular approach using two or more FDDs. The male-to-female ratio in these cases was 5:3, and there is a wide age range from 22 months to 69 years old [
The most reported aneurysmal site was the cavernous segment of the ICA, with a total of three cases; two of the reported cases consisted of vertebral artery aneurysms, and the remaining cases were of middle cerebral artery aneurysms, basilar artery aneurysm, and two anterior communicating artery aneurysms.
The type of FDD used was PED in five reported cases; enterprise was used in two cases, while silk FDD was deployed in only one of the mentioned cases. The number of FDDs deployed to occlude the aneurysm differed between the reported cases. A total of two PEDs were deployed in two of these cases; two cases showed the use of three FDDs, two other cases described the use of five FDDs, while the two remaining cases either used four FDDs or did not specify the exact number.
The outcome was similar in all the reported cases, with complete occlusion of the aneurysm on follow-up with no signs of ischemia and no complications associated with the stents’ placement.
DISCUSSION
Management of intracranial aneurysms includes open surgical approaches by clipping the aneurysm or endovascular treatment, which consists of direct embolization, stenting alone, and flow diversion. FDDs are becoming more important in aneurysmal treatment due to the significant intraoperative complications associated with open surgical approaches, the shallow nature, the shape of the aneurysms, and the natural tortuosity in some vessels such as the ICA, which renders stent-assisted coiling ineffective.[
FDDs are new-generation stents used primarily in large and giant aneurysms, wide-necked, and recurrent aneurysms.[
When deployed, FDDs produce vessel reconstruction by two main hemodynamic and biological effects, which consist of redirection of blood flow by bridging the neck of the aneurysm, leading to thrombosis inside the aneurysm. Therefore, excluding the sac from circulation, without the need to catheterize it, decreases the risk of aneurysmal rupture and tissue overgrowth by providing scaffolding for the production of endothelium and neointimal tissue across the neck of the aneurysm.[
The decision of the best endovascular approach and indications for the use of FDDs are still a subject of debate. Flow diversion has five main types that have been approved for the management of intracranial aneurysm: the PED, which is a self-expanding, flexible, and cylindrical mesh-like device consisting of platinum tungsten and cobalt chromium, made from 48 strands interwoven in a standard pattern, the Silk is a self-expanding stent made of 48 braided nitinol strands that have a wider range of diameters than in PED, the FRED, the p64 Flow Modulation, and the Surpass Flow Diverter.[
Significant disadvantages of using FDDs include their higher cost value, high reoperation rate, and increased risk of pressure effect on an aneurysm after the placement of a stent, which is still a subject of discussion and remains one of the critical issues associated with FDDs.[
The delayed migration of a flow diverter stent is a severe but rare complication that could be associated with a high mortality rate. The migration of the device can be seen proximally or distally in the parent artery and can result in aneurysm rupture or thromboembolic incidents. The risk factors for FDD proximal or distal migration include a substantial mismatch in diameter between the inflow and outflow vessels; giant aneurysms with a long neck; tortuous parent vessels; and the patient’s underlying vascular risk factors, such as smoking and hypertension, which can lead to the delay of the endothelialization of the FDD. Management of delayed FDD migration includes endovascular procedures such as stent-assisted coiling, balloon anchoring, and flow diverter placement, in addition to sacrificing the parent vessel. Prevention of the delayed flow diverter stents migration can be done through the accurate measurements of the diameters within the inflow and outflow vessels, vigilance is needed in choosing the correct size, length, and the number of stents to be placed.[
The utilization of multiple telescoped FDDs might be well tolerated in cases where neurosurgeons believe that multiple stents would improve the aneurysm occlusion rates compared with single devices.[
We conducted a brief review of the literature for using two or more FDDs in treating patients with intracranial aneurysms. We have found eight similar cases in the literature in which multiple FDDs were deployed to manage an intracranial aneurysm. Similar to our case, all the reported cases improved the patients’ symptoms with successful occlusion of the aneurysm observed during follow-up. However, none of the cases mentioned showed delayed complications, including the migration of the FDDs deployed in the parent vessel, like in our case.
CONCLUSION
Tandem flow diverter deployment has technical challenges and complications, which include complete obstruction. Planning and learning from experience with the continuous advancement in such technologies are the typical way to overcome such complications in the future.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abouelleil M, Chehab A, Nabulsi O, Singer J, Mazaris P. Use of pipeline flex flow diverter in the treatment of an internal carotid artery dissection: A case report. Interdiscip Neurosurg. 2022. 29: 101577
2. Bender MT, Jiang B, Campos JK, Lin LM, Beaty N, Vo CD. Single-stage flow diversion with adjunctive coiling for cerebral aneurysm: Outcomes and technical considerations in 72 cases. J Neurointerv Surg. 2018. 10: 843-50
3. Briganti F, Leone G, Marseglia M, Mariniello G, Caranci F, Brunetti A. Endovascular treatment of cerebral aneurysms using flow-diverter devices: A systematic review. Neuroradiol J. 2015. 28: 365-75
4. Cohen JE, Gomori JM, Moscovici S, Itshayek E. Successful endovascular treatment of a growing megadolichoectasic vertebrobasilar artery aneurysm by flow diversion using the “diverter-in-stent” technique. J Clin Neurosci. 2012. 19: 166-70
5. Crowley RW, Evans AJ, Kassell NF, Jensen ME, Dumont AS. Endovascular treatment of a fusiform basilar artery aneurysm using multiple “in-stent stents” Technical note. J Neurosurg Pediatr. 2009. 3: 496-500
6. Dai D, Ding YH, Kadirvel R, Rad AE, Lewis DA, Kallmes DF. Patency of branches after coverage with multiple telescoping flow-diverter devices: An in vivo study in rabbits. AJNR Am J Neuroradiol. 2012. 33: 171-4
7. Ikeda DS, Marlin ES, Shaw A, Powers CJ. Successful endovascular reconstruction of a recurrent giant middle cerebral artery aneurysm with multiple telescoping flow diverters in a pediatric patient. Pediatr Neurosurg. 2015. 50: 88-93
8. Imahori T, Shose H, Okamura Y, Kohmura E. Deploying 5 overlapping enterprise stents and coiling for treating hemorrhagic vertebral artery dissecting aneurysm. World Neurosurg. 2019. 132: 177-81
9. Kojima M, Irie K, Fukuda T, Arai F, Hirose Y, Negoro M. The study of flow diversion effects on aneurysm using multiple enterprise stents and two flow diverters. Asian J Neurosurg. 2012. 7: 159-65
10. Manning NW, Cheung A, Phillips TJ, Wenderoth JD. Pipeline shield with single antiplatelet therapy in aneurysmal subarachnoid haemorrhage: Multicentre experience. J Neurointerv Surg. 2019. 11: 694-8
11. Mantripragada K, Echeverry N, Mansour S, Peterson EC, Snelling B. Treatment of bilateral giant fusiform petrocavernous aneurysms. Cureus. 2020. 12: e8662
12. Miyachi S, Ohnishi H, Hiramatsu R, Yagi R, Kuroiwa T. Tied pipeline: A case of rare complication. Neurol Med Chir (Tokyo). 2018. 58: 219-24
13. Piano M, Valvassori L, Quilici L, Pero G, Boccardi E. Midterm and long-term follow-up of cerebral aneurysms treated with flow diverter devices: A single-center experience: Special topic. J Neurosurg. 2013. 118: 408-16
14. Pierot L. Flow diverter stents in the treatment of intracranial aneurysms: Where are we?. J Neuroradiol. 2011. 38: 40-6
15. Rouchaud A, Saleme S, Gory B, Ayoub D, Mounayer C. Endovascular exclusion of the anterior communicating artery with flow-diverter stents as an emergency treatment for blister-like intracranial aneurysms. A case report. Interv Neuroradiol. 2013. 19: 471-8
16. Son W, Kang DH, Kim BM, Park J, Kim YS. Retrograde snare-assisted rescue via anterior communicating artery for lost access during multiple overlapping pipeline embolization device placement. World Neurosurg. 2018. 114: 4-7
17. Stamatopoulos T, Anagnostou E, Plakas S, Papachristou K, Lagos P, Samelis A. Treatment of carotid cavernous sinus fistulas with flow diverters. A case report and systematic review. Interv Neuroradiol. 2022. 28: 70-83
18. Tsai YH, Wong HF, Hsu SW. Endovascular management of spontaneous delayed migration of the flow-diverter stent. J Neuroradiol. 2020. 47: 38-45
19. Wang CB, Shi WW, Zhang GX, Lu HC, Ma J. Flow diverter treatment of posterior circulation aneurysms. A meta-analysis. Neuroradiology. 2016. 58: 391-400
20. Ye G, Zhang M, Deng L, Chen X, Wang Y. Meta-analysis of the efficiency and prognosis of intracranial aneurysm treated with flow diverter devices. J Mol Neurosci. 2016. 59: 158-67