- Department of Neurosurgery, Hospital Ernesto Dornelles, Porto Alegre, Rio Grande do Sul, Brazil.
Correspondence Address:
Carlos Eduardo da Silva, Department of Neurosurgery, Hospital Ernesto Dornelles, Porto Alegre, Rio Grande do Sul, Brazil.
DOI:10.25259/SNI_509_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tamara Brun Vidaletti, Ana Clara Thibes, Carlos Eduardo da Silva. Falcine meningioma: FEBAIR principles in a “Grade Zero” concept application – 2D operative video. 27-Oct-2023;14:380
How to cite this URL: Tamara Brun Vidaletti, Ana Clara Thibes, Carlos Eduardo da Silva. Falcine meningioma: FEBAIR principles in a “Grade Zero” concept application – 2D operative video. 27-Oct-2023;14:380. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12615
Abstract
Background: Falcine meningiomas account for 5% of intracranial meningiomas. They may involve the eloquent cortex as well as vascular structures. Gross-total resection with additional margins has been shown to be beneficial to patients and has been associated with a reduction in disease recurrence.
Case Description: A 57-year-old patient presented with recurrent frontal headaches that worsened when lying down. Magnetic resonance imaging showed a large lesion with homogeneous enhancement attached to the anterior third of the falx cerebri at the right frontal lobe, causing significant compression, and suggesting a meningioma.
Conclusion: This operative video highlights the application of 1st-time, exposure, bone removal, arachnoid, irrigation, and reconstruction principles for safely and effectively removing a large falcine meningioma using the “grade zero” concept for maximal resection.
Keywords: Falcine meningioma, Falx cerebri, Grade zero resection, Meningioma, Simpson
INTRODUCTION
Falcine meningiomas were described by Cushing and Eisenhardt as tumors that arise from the falx cerebri and are in contact with the adjacent cortex.[
F- First-time surgery – essential for total removal and disease control due to preserved anatomical structures.[ E- Exposure – consideration of all of the limits related to the origin and extent of the tumor to select the best approach.[ B- Bone removal – hyperostosis adjacent to the meningioma indicates tumor involvement in most cases.[ A- Arachnoid plane dissection – This is key to neurovascular preservation.[ I- Irrigation – Warm saline helps identify the arachnoid plane and hemostasis, avoiding bipolar coagulation.[ R- Reconstruction – the final step to prevent cerebrospinal fluid fistulas and esthetic disturbances.[
Since the seminal work of Simpson, the complete removal of the tumor, the dura, and any bone involvement by the meningioma has been defined as a grade I resection.[
The present article illustrates the application of FEBAIR principles for the 1st time, as shown in an operative video case report involving a “grade zero” gross-total resection of a falcine meningioma.
CASE DESCRIPTION
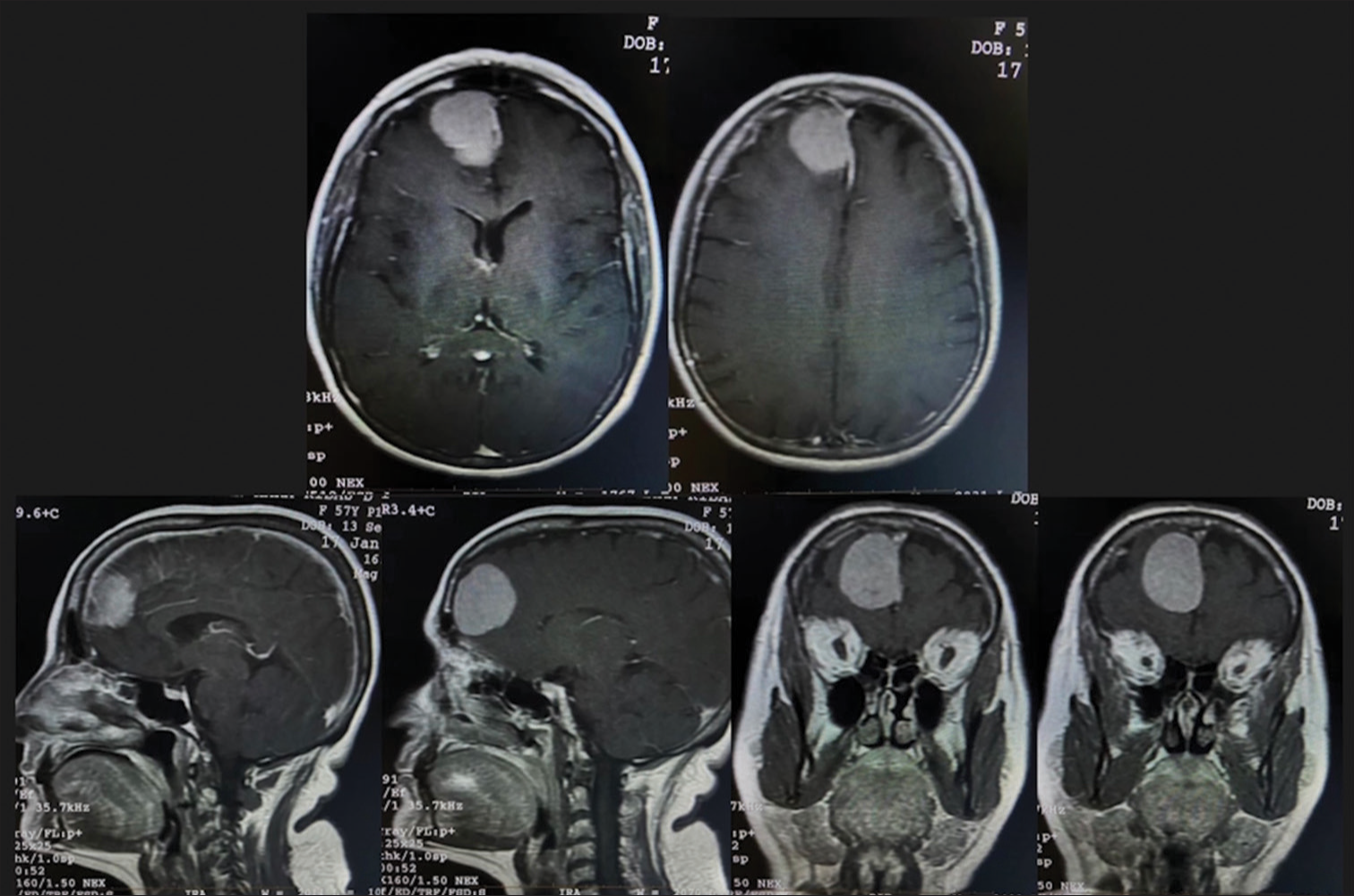
This paper presents the case of a 57-year-old woman with a history of intense frontal headaches which worsened in the decubitus position over the past 6 months. Her medical history included hypertriglyceridemia and prediabetes. There were no neurological deficits on physical examination. The preoperative magnetic resonance imaging (MRI) showed a large nodular lesion with homogeneous enhancement attached to the falx cerebri at the right frontal lobe region, strongly suggesting a diagnosis of meningioma [
Surgical technique
The objective of the surgery was a “grade zero” total tumor removal aiming to cure the disease. The senior author (CES) operated on the patient by applying the principles of meningioma surgery represented by the acronym FEBAIR.[
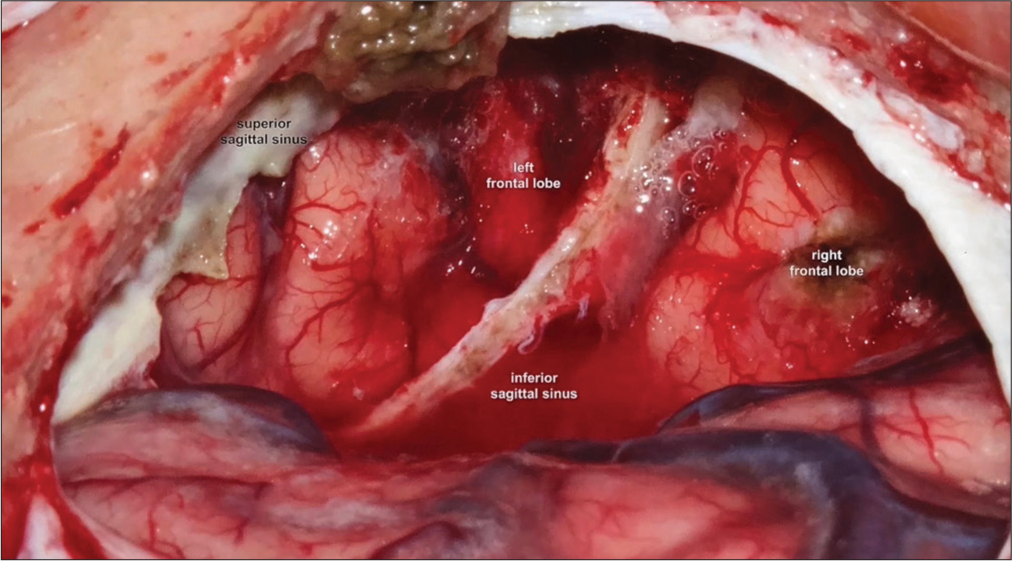
A frontal parasagittal approach with complete and direct exposure of the lesion was chosen for this case. The concept of grade zero resection includes not only the complete removal of the tumor and the coagulation of its dural attachment but also the removal of an additional 2–3 cm of the falx cerebri anterior and posteriorly from this attachment and inferiorly from the superior sagittal sinus.[
The frontal craniotomy was performed superiorly from the superior temporal line to avoid the dissection of the temporal muscle, superior to the frontal sinus, and laterally from the superior sagittal sinus to reduce the risk of injury.
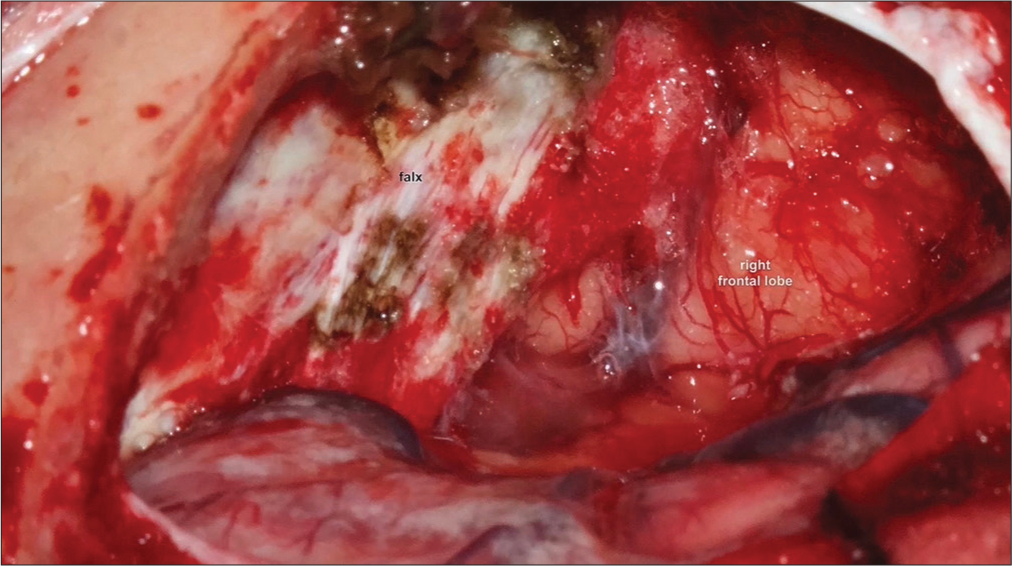
After the craniotomy, the dura-mater was opened in a flap manner, with its base turned to the midline, lateral to the superior sagittal sinus. The dissection was, then, performed using the arachnoid plane, separating the lesion from the right frontal lobe, and preserving the adjacent frontal drainage veins. Then, debulking of the medial portion of the lesion was performed close to its attachment at the falx cerebri, using biopsy forceps and a bipolar cautery device. This initial maneuver permitted access to the tumoral implantation on the right side of the falx cerebri.
Next, a coagulation of the tumoral implants was performed and the tumor attached to the right side of the falx was removed, devascularizing the lesion. The dissection was then resumed through the arachnoid plane, completely liberating the tumor from the right frontal lobe and allowing its en bloc removal, thus achieving a Simpson grade II resection [
The reconstruction was performed through a primary suture of the dural flap, maintaining external protection with Gelfoam. Then, the bone flap from the frontal craniotomy was repositioned and fixed with mini titanium plaques – enabling an excellent esthetic result for the cranioplasty.
Postoperative
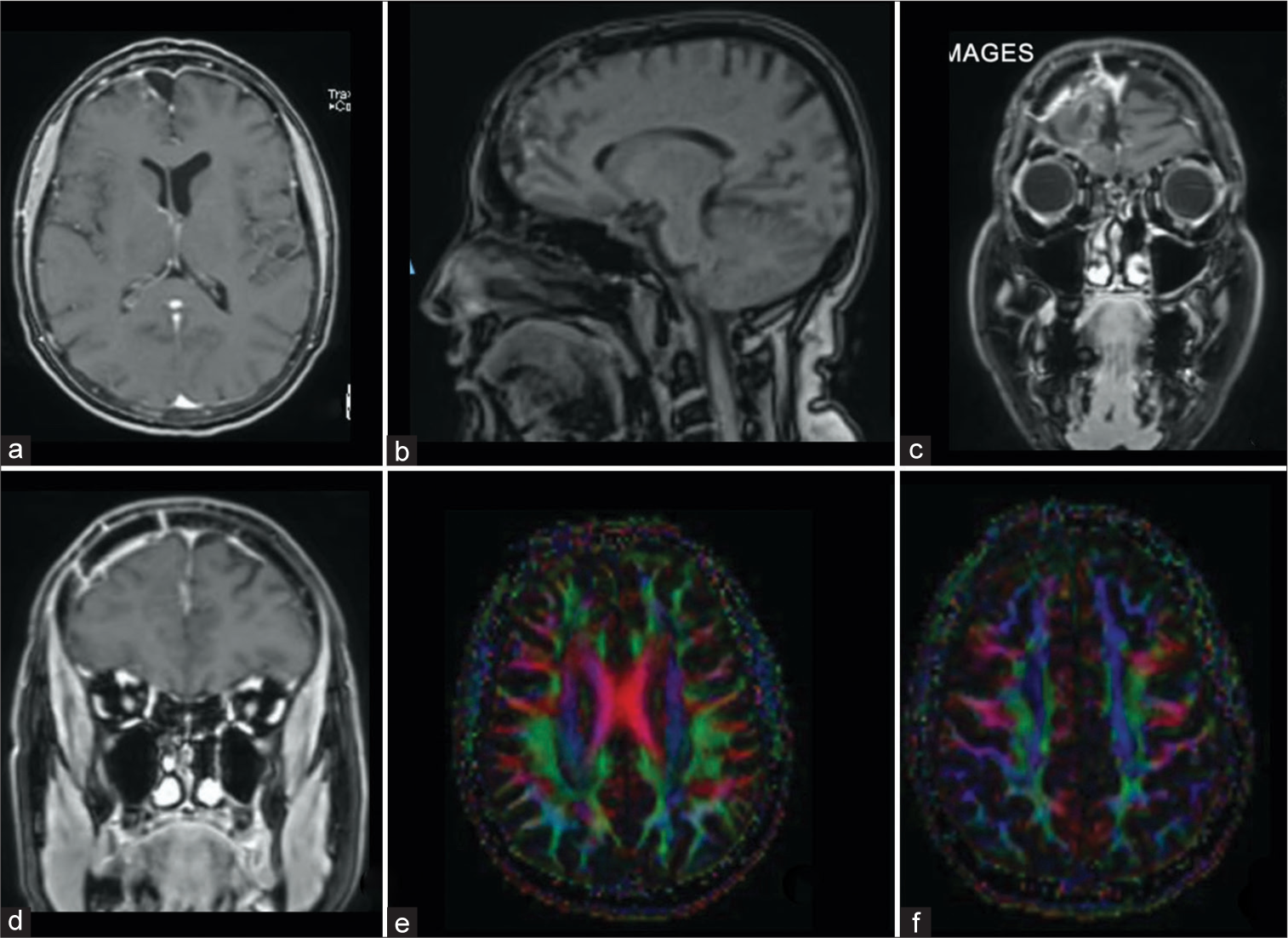
A postoperative MRI conducted 30 days after the procedure showed total resection of the tumor with vascular preservation and preservation of the right frontal association fascicules in the tractography sequence [
Video 1
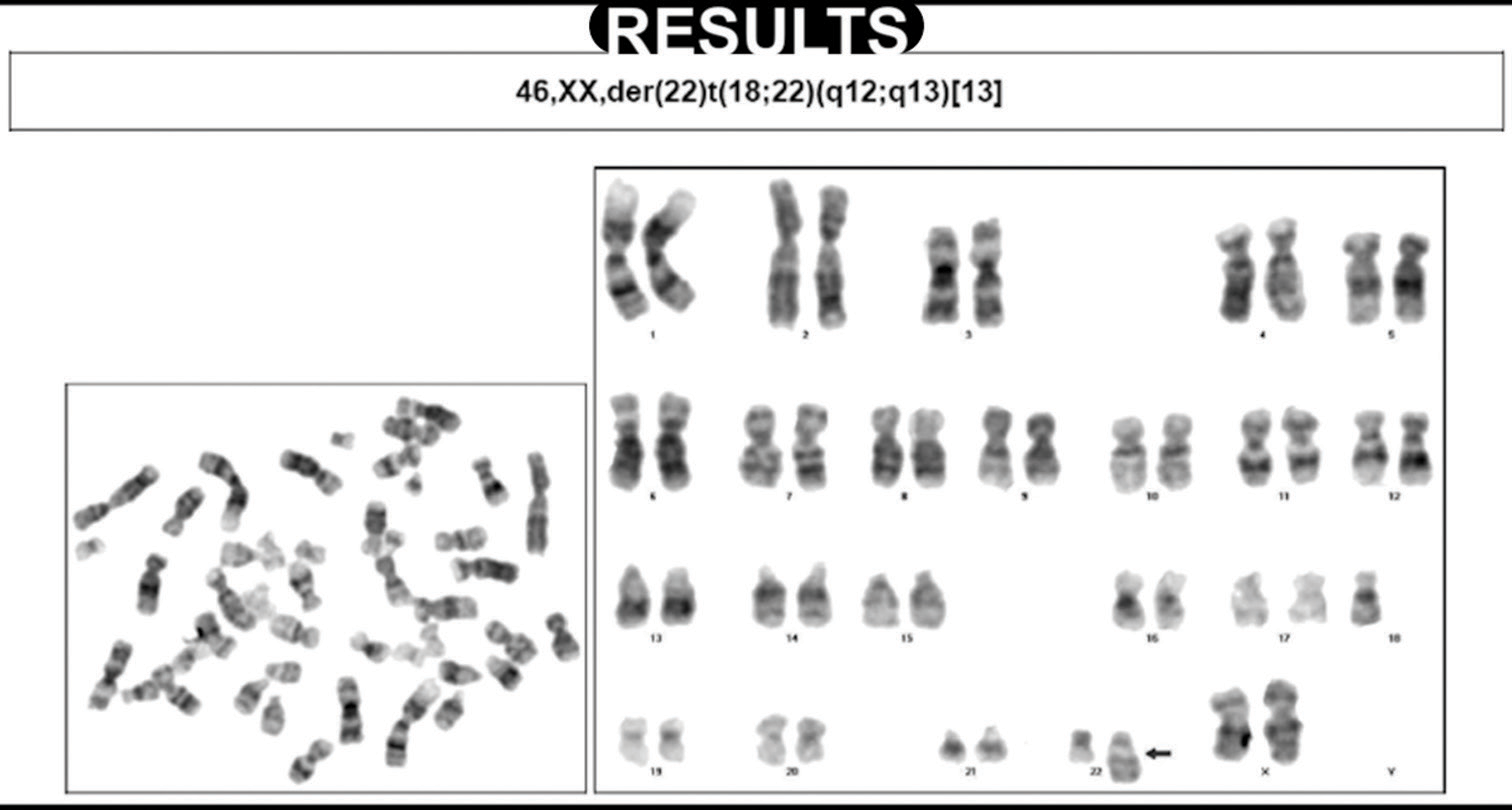
The anatomopathological study examined the meningothelial meningioma; confirming that the tumor resection was performed with a safe margin as evidenced by the absence of a tumoral implant in the dura mater sample. The cytogenetic study reviewed abnormal cellular lineage, presenting the depletion of the short arm of chromosome 18 and the depletion of the long arm of chromosome 22 [
CONCLUSION
Adherence to the principles of meningioma surgery represented by the acronym FEBAIR is helpful in achieving the best surgical results. Furthermore, the extension of the falx resection proposed for falcine meningiomas benefits patients by reducing the risk of recurrence.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available on
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cushing H, Eisenhardt L, editors. Primary meningiomas of the falx cerebri. Meningiomas: Their classification, regional behaviour, life history and surgical end results. Baltimore, MD: Charles C Thomas; 1938. p. 538-55
2. da Silva CE, Zanatta C, Thibes AC, Vidaletti T. Sphenoid wing meningiomas with secondary cavernous sinus invasion: Surgical results and algorithm for treatment at a single brazilin center. World Neurosurg. 2022. 163: e635-46
3. Jaaskelainen J. Seemingly complete removal of histologically benign intracranial meningioma: Late recurrence rate and factors predicting recurrence in 657 patients. A multivariate analysis. Surg Neurol. 1986. 26: 461-9
4. Kinjo T, Al-Mefty O, Kanaan I. Grade zero removal of supratentorial convexity meningiomas. Neurosurgery. 1993. 33: 394-9 discusion 399
5. Mooney MA, Abolfotoh M, Bi WL, Tavanaiepour D, Almefty RO, Bassiouni H. Is falcine meningioma a diffuse disease of the falx? Case series and analysis of a “grade zero” resection. Neurosurgery. 2020. 87: 900-9
6. Mooney MA, Aboud E, Essayed WI, Al-Mefty O. Grade zero” removal of a falcine meningioma: 2-dimensional operative video. Oper Neurosurg (Hagerstown). 2022. 22: e158
7. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957. 20: 22-39