- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita City, Japan
- Department of Neurosurgery Kouhoukai Takagi Hospital, Okawa, Japan
- Department of Pathology, Kouhoukai Takagi Hospital, Okawa, Japan
- Department of Neurosurgery, Faculty of Medicine, Saga University, Saga, Japan.
Correspondence Address:
Tatsuya Tanaka, Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita City, Japan.
DOI:10.25259/SNI_54_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tatsuya Tanaka1, May Pyae Kyaw2, Satoshi Anai2, Yukinori Takase2, Yukari Takase3, Tatsuya Abe4, Akira Matsuno1. Fatal convexity and interhemispheric acute subdural hematoma from a falx meningioma: A case report. 05-Apr-2024;15:115
How to cite this URL: Tatsuya Tanaka1, May Pyae Kyaw2, Satoshi Anai2, Yukinori Takase2, Yukari Takase3, Tatsuya Abe4, Akira Matsuno1. Fatal convexity and interhemispheric acute subdural hematoma from a falx meningioma: A case report. 05-Apr-2024;15:115. Available from: https://surgicalneurologyint.com/surgicalint-articles/12848/
Abstract
Background: Hemorrhagic meningiomas are rare. We report a rare case of nontraumatic convexity and interhemispheric acute subdural hematoma (ASDH) caused by a falx meningioma.
Case Description: An 84-year-old woman with a history of atrial fibrillation and hypertension who was taking warfarin presented to our emergency department with a sudden disorder of consciousness. The patient had no traumatic events associated with her symptoms. Computed tomography (CT) revealed right convexity and interhemispheric ASDH, mass lesions in the left frontal lobes, and brain herniation. Contrast-enhanced CT revealed vascular structures within the mass lesion. CT angiography (CTA) revealed no aneurysm or arteriovenous malformation, and the venous phase revealed occlusion in the anterior portion of the superior sagittal sinus. The patient had her right convexity and interhemispheric ASDH removed endoscopically. A mass lesion located on the falx, which was easily bleeding, soft, and suctionable, was immediately detected. Histopathological examination revealed fibrous meningioma, a benign meningioma of the World Health Organization grade 1. Despite undergoing aggressive treatment, the patient’s general condition deteriorated.
Conclusion: Hemorrhagic meningiomas can easily be missed with plain CT, and the enhancement effect of CTA and tumor shadow on digital subtraction angiography may not be observed during the acute phase. Surgery for nontraumatic ASDH should be performed considering the possibility that a meningioma causes it.
Keywords: Falx meningioma, Grade 1 meningioma, Interhemispheric acute subdural hematoma, Intratumoral hemorrhage, Nontraumatic acute subdural hematoma
INTRODUCTION
Meningiomas are benign tumors that frequently occur in the central nervous system of adults. The World Health Organization (WHO) classifies roughly 80–90% of meningioma cases as grade 1, implying that these lesions are histologically benign.[
Even though these tumors are benign, they might bleed due to radiation therapy, embolization before surgery, or spontaneous events, although the incidence rate of bleeding (1.3–2.4%) is lower than that in malignant tumors.[
The most prevalent types of bleeding related to meningiomas are subarachnoid hemorrhage and intracerebral hemorrhage.[
In this report, we present a case of falx meningioma that manifested with acute subdural hemorrhage on the convexity and interhemispheric region in a comatose patient with a review of the literature.
CASE DESCRIPTION
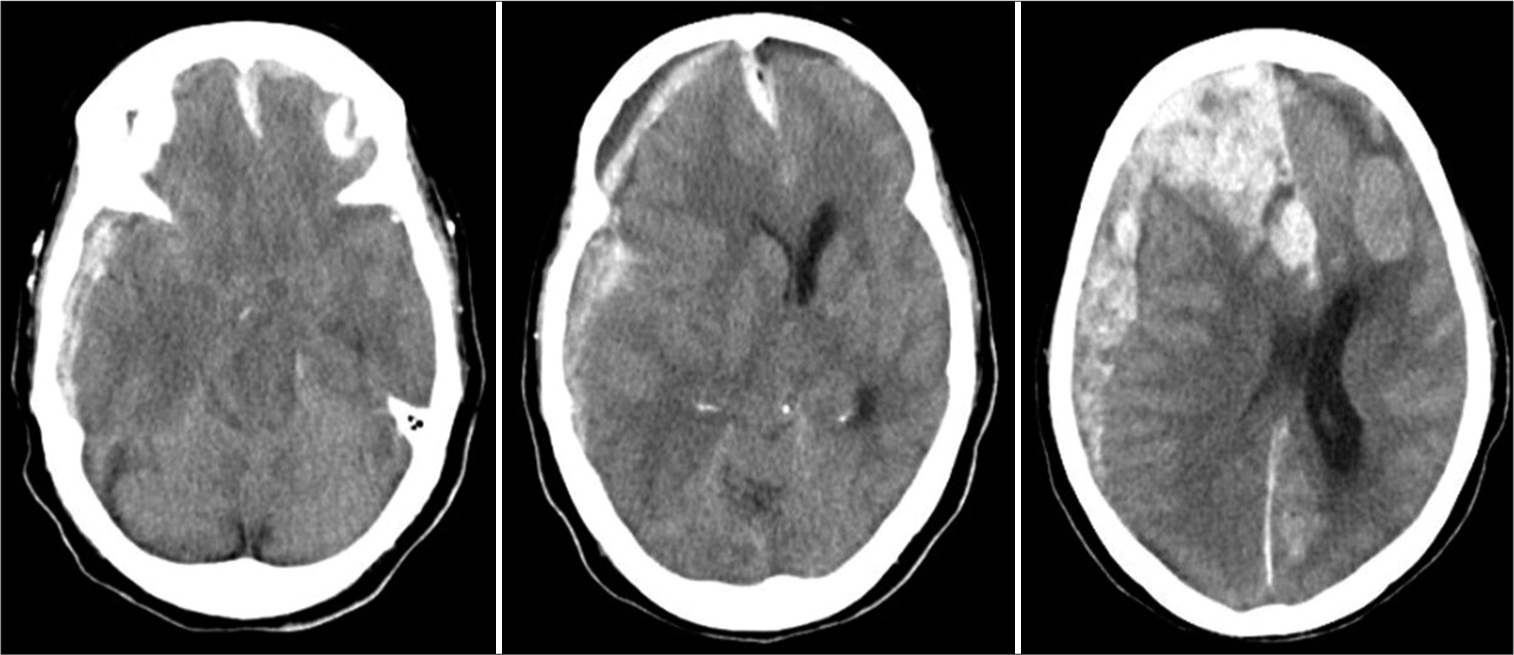
An 84-year-old woman with a history of atrial fibrillation and hypertension who was taking warfarin and antihypertensive medications presented to our emergency department with a sudden disorder of consciousness. The patient had no traumatic events associated with her symptoms. On initial assessment, the patient had a Glasgow Coma Scale (GCS) score of 3, with bilateral pupil diameters of 4 mm and a dull light reflex. Computed tomography (CT) revealed right convexity and interhemispheric acute subdural hematoma (ASDH), mass lesions in the left frontal lobes, and brain herniation [
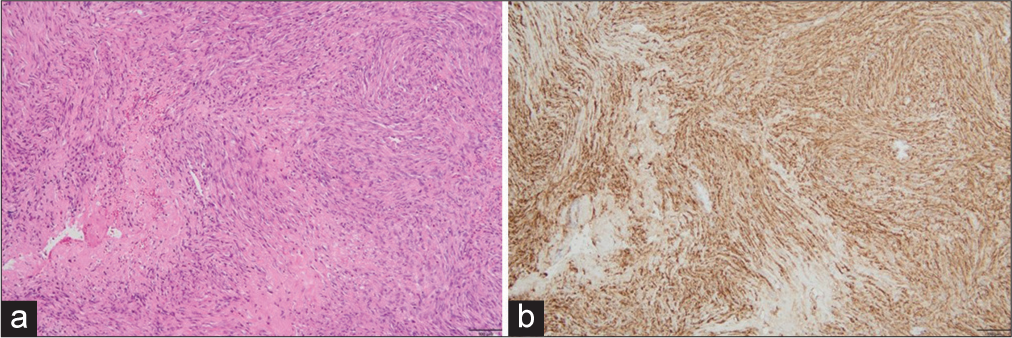
The patient was intubated for airway protection. Tranexamic acid, menatetrenone, and 4-factor prothrombin complex concentrate were intravenously administered. During emergency surgery, a right frontal minicraniotomy and dural incision were performed. The patient had her right convexity and interhemispheric ASDH removed endoscopically. A mass lesion located on the falx, which was easily bleeding, soft, and suctionable, was immediately detected. After the removal of the lesion, bleeding from the falx was stopped through cauterization and packing with gelatin sponge and BioGlue. No other active bleeding points, such as cortical arteries or bridging veins, were observed in the subdural space. Brain swelling was insignificant. Histopathological examination revealed that spindle-shaped tumor cells proliferated in fascicular or storiform patterns with collagenous stroma. The tumor tissue revealed no mitosis, nuclear atypia, and tumor necrosis [
DISCUSSION
The overall intratumoral hemorrhage rate for brain tumors is 14.6%, with a significant difference in the hemorrhage rate among different histological tumor types.[
Several hypotheses have been proposed to explain the mechanism of meningioma growth accompanied by massive ASDH. They include the following: (1) disruption of tumor vessels due to tumor growth; (2) disruption of bridging veins due to tumor growth; (3) direct invasion of tumor cells into blood vessels; (4) release of vasoactive substances by tumor cells; (5) disruption of bridging veins due to local venous hypertension caused by a secondary condition, such as Valsalva maneuver or cough; and (6) anticoagulant or antiplatelet medications, blood dyscrasias, or hypertension.[
In our case, the tumor was not identified as a pathologically malignant meningioma and lacked an obvious traumatic mechanism. Furthermore, in this case, the occlusion of the venous sinuses and deep veins due to the meningioma may have increased intratumoral venous pressure. Furthermore, the use of anticoagulant drugs and hypertension may have led to significant bleeding due to the delicate nature of the tumor vessels. Diagnosing meningiomas is typically straightforward based on clinical presentation and conventional radiological findings.[
Our case started with clinical findings and was systematically approached with CT and then CTA; however, magnetic resonance imaging (MRI) was not possible due to emergency surgery. Due to the possibility of the presence of nontraumatic intracranial hemorrhage, the surgical field was carefully observed, and ASDH due to meningioma was diagnosed during surgery. Imaging findings that are not typical of a simple traumatic hematoma may indicate meningioma hemorrhage, and neurosurgeons should be alert to these signs, particularly in patients requiring emergency surgery where preoperative MRI is not possible. For patients with intracranial hemorrhage who do not require urgent workup or treatment, contrast-enhanced MRI should be performed for further investigation.
CONCLUSION
We report a rare case of falx meningioma caused by nontraumatic convexity and interhemispheric ASDH. Hemorrhagic meningiomas can be easily missed with plain CT, and the enhancement effect of CTA and tumor shadow on DSA may not be observed during the acute phase. Surgery for nontraumatic ASDH should be performed considering the possibility that a meningioma causes it.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alghabban FA, Alhamss YJ, Farag AA, Alfahmi JA, AlSaiari SA, Alghamdi F. Incidental intraoperative finding of meningioma in spontaneous acute subdural hematoma: A case report from Saudi Arabia and review of literature. Int J Surg Case Rep. 2020. 77: 314-7
2. Basil G, Urakov T, Knudsen MG, Morcos J. Jugular tubercle meningioma with hemorrhagic conversion mimicking a ruptured thrombosed giant vertebrobasilar aneurysm. World Neurosurg. 2018. 119: 108-12
3. Dallocchio C, Borutti G, Frascaroli G, Camana C, Magrotti E. A sudden bleeding meningioma. Neurol Sci. 2003. 23: 327-8
4. Di Rocco F, Mannino S, Puca A, Lauriola L, Pompucci A. Intracranial meningiomas associated with non-traumatic chronic subdural hematoma. Acta Neurochir (Wien). 2006. 148: 1097-102
5. Donato J, Campigotto F, Uhlmann EJ, Coletti E, Neuberg D, Weber GM. Intracranial hemorrhage in patients with brain metastases treated with therapeutic enoxaparin: A matched cohort study. Blood. 2015. 126: 494-9
6. Goyal A, Singh AK, Kumar S, Gupta V, Singh D. Subdural hemorrhage associated with falcine meningioma. Neurol India. 2003. 51: 419-21
7. Huang RB, Chen LJ, Su SY, Wu X, Zheng YG, Wang HP. Misdiagnosis and delay of diagnosis in hemorrhagic meningioma: A case series and review of the literature. World Neurosurg. 2021. 155: e836-46
8. Kondziolka D, Bernstein M, Resch L, Tator CH, Fleming JF, Vanderlinden RG. Significance of hemorrhage into brain tumors: Clinicopathological study. J Neurosurg. 1987. 67: 852-7
9. Krishnan P, Jena M, Kartikueyan R. Occult falcine meningioma unmasked following nearly complete hemorrhagic transformation with resultant spontaneous acute interhemispheric subdural hematoma. J Neurosci Rural Pract. 2015. 6: 91-3
10. Krishnan V, Mittal MK, Sinha M, Thukral BB. Imaging spectrum of meningiomas: A review of uncommon imaging appearances and their histopathological and prognostic significance. Pol J Radiol. 2019. 84: e630-53
11. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007. 114: 97-109
12. Mantia C, Uhlmann EJ, Puligandla M, Weber GM, Neuberg D, Zwicker JI. Predicting the higher rate of intracranial hemorrhage in glioma patients receiving therapeutic enoxaparin. Blood. 2017. 129: 3379-85
13. Martinez-Lage JF, Poza M, Martinez M, Esteban JA, Antunez MC, Sola J. Meningiomas with haemorrhagic onset. Acta Neurochir (Wien). 1991. 110: 129-32
14. Matsuoka G, Eguchi S, Ryu B, Tominaga T, Ishikawa T, Yamaguchi K. Treatment strategy for recurrent hemorrhage from meningioma: Case report and literature review. World Neurosurg. 2019. 124: 75-80
15. Miki K, Kai Y, Hiraki Y, Kamano H, Oka K, Natori Y. Malignant meningioma mimicking chronic subdural hematoma. World Neurosurg. 2019. 124: 71-4
16. Okuno S, Touho H, Ohnishi H, Karasawa J. Falx meningioma presenting as acute subdural hematoma: Case report. Surg Neurol. 1999. 52: 180-4
17. Ostrom QT, Cioffi G, Gittleman H, Patil N, Waite K, Kruchko C. CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro Oncol. 2019. 21: v1-100
18. Omar AT, Starreveld YP. Meningiomas associated with subdural hematoma: A systematic review of clinical features and outcomes. World Neurosurg. 2022. 158: e465-75
19. Oyamada K, Ohbuchi H, Nishiyama K, Imazato D, Inazuka M, Hagiwara S. Acute subdural hematoma associated with disruption of tumor vessels due to rapid growth of falx meningioma: A case report and literature review. Surg Neurol Int. 2022. 13: 495
20. Pressman E, Penn D, Patel NJ. Intracranial hemorrhage from meningioma: 2 novel risk factors. World Neurosurg. 2020. 135: 217-21
21. Pelz D, Levine AB, MacDougall KW. Subdural hematoma: A rare presentation of a convexity meningioma. Can J Neurol Sci. 2014. 41: 506-7
22. Sato K, Matsuo A, Hiu T, Kurohama H, Miura S, Ito K. Falx meningioma presenting with intratumoral hemorrhage and interhemispheric acute subdural hematoma: A case of report. No Shinkei Geka. 2020. 48: 413-22
23. Suzuki Y, Fujimoto M, Kawakita F, Asakura F, Murata H,Morooka Y. Tiny falx meningioma causing massive interhemishelic subdural hematoma: A case report. NMC Case Rep J. 2018. 5: 51-5
24. Sunada I, Nakabayashi H, Matsusaka Y, Yamamoto S. Meningioma associated with acute subdural hematoma--case report. Radiat Med. 1998. 16: 483-6
25. Wakai S, Yamakawa K, Manaka S, Takakura K. Spontaneous intracranial hemorrhage caused by brain tumor: Its incidence and clinical significance. Neurosurgery. 1982. 10: 437-44
26. Whittle IR, Smith C, Navoo P, Collie D. Meningiomas. Lancet. 2004. 363: 1535-43