- Department of Neurosurgery, Fukuoka University, Fukuoka, Japan.
Correspondence Address:
Takaaki Amamoto, Department of Neurosurgery, Fukuoka University, Fukuoka, Japan.
DOI:10.25259/SNI_105_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kazunori Oda, Takaaki Amamoto, Toshiyuki Enomoto, Hiromasa Kobayashi, Takashi Morishita, Mitsutoshi Iwaasa, Hiroshi Abe, Tooru Inoue. Favorable management of symptomatic cerebellar hemangioblastoma presenting with obstructive hydrocephalus during pregnancy: A case report and literature review. 29-Apr-2022;13:174
How to cite this URL: Kazunori Oda, Takaaki Amamoto, Toshiyuki Enomoto, Hiromasa Kobayashi, Takashi Morishita, Mitsutoshi Iwaasa, Hiroshi Abe, Tooru Inoue. Favorable management of symptomatic cerebellar hemangioblastoma presenting with obstructive hydrocephalus during pregnancy: A case report and literature review. 29-Apr-2022;13:174. Available from: https://surgicalneurologyint.com/surgicalint-articles/11569/
Abstract
Background: Cerebellar hemangioblastoma is a highly vascular benign tumor and the growth rate of hemangioblastomas is believed to often accelerate during pregnancy; however, the reason for this rapid increase in size remains poorly understood. There are several case reports of symptomatic hemangioblastoma during pregnancy; however, the favorable management strategy has not been well established.
Case Description: A 35-year-old woman, gravida 2 para 1, with no significant medical history presented with vertigo and difficulty walking at around 11 weeks of pregnancy and was referred to our institute at 30 weeks of gestation because of worsening symptoms. Brain magnetic resonance imaging revealed a 5.6 cm cystic lesion with a mural nodule in the right cerebellar hemisphere and the lesion blocked cerebrospinal fluid drainage from the fourth ventricle and brainstem, resulting in obstructive hydrocephalus. After obtaining the patient’s consent, a multidisciplinary team consisting of obstetricians and neurosurgeons decided to perform resection of the intracranial lesion following delivery of the fetus by emergency cesarean section in view of the symptoms of increased intracranial pressure. The patient’s general condition was confirmed to be stable postoperatively and she was discharged on the 16th day of her hospitalization without any neurological deficits or fetal complications.
Conclusion: Urgent tumor resection combined with cesarean section can be planned once fetal lung maturity is confirmed. Most cases of symptomatic hemangioblastoma during pregnancy have an uneventful gestational course and a favorable outcome for both mother and child.
Keywords: Hemangioblastoma, Neuro-oncology, Neurosurgery, Obstructive Hydrocephalus, Pregnancy
INTRODUCTION
Cerebellar hemangioblastoma is a highly vascular benign tumor, accounting for approximately 3% of all central nervous system tumors.[
In the present article, we report a case of symptomatic cerebellar hemangioblastoma in a 35-year-old woman at 30 weeks of gestation managed successfully with emergency surgical resection following cesarean section.
CASE PRESENTATION
A 35-year-old woman, gravida 2 para 1, with no significant medical history presented with vertigo at around 11 weeks of pregnancy and gradually became unable to walk. At 15 weeks of gestation, she was diagnosed with vestibular disorder by a local otolaryngologist. She was hospitalized and treated with steroids, but her symptoms did not improve. When she was 30 weeks and 4 days pregnant, her symptoms worsened and she could not walk. She was then referred to our institute for further evaluation and treatment.
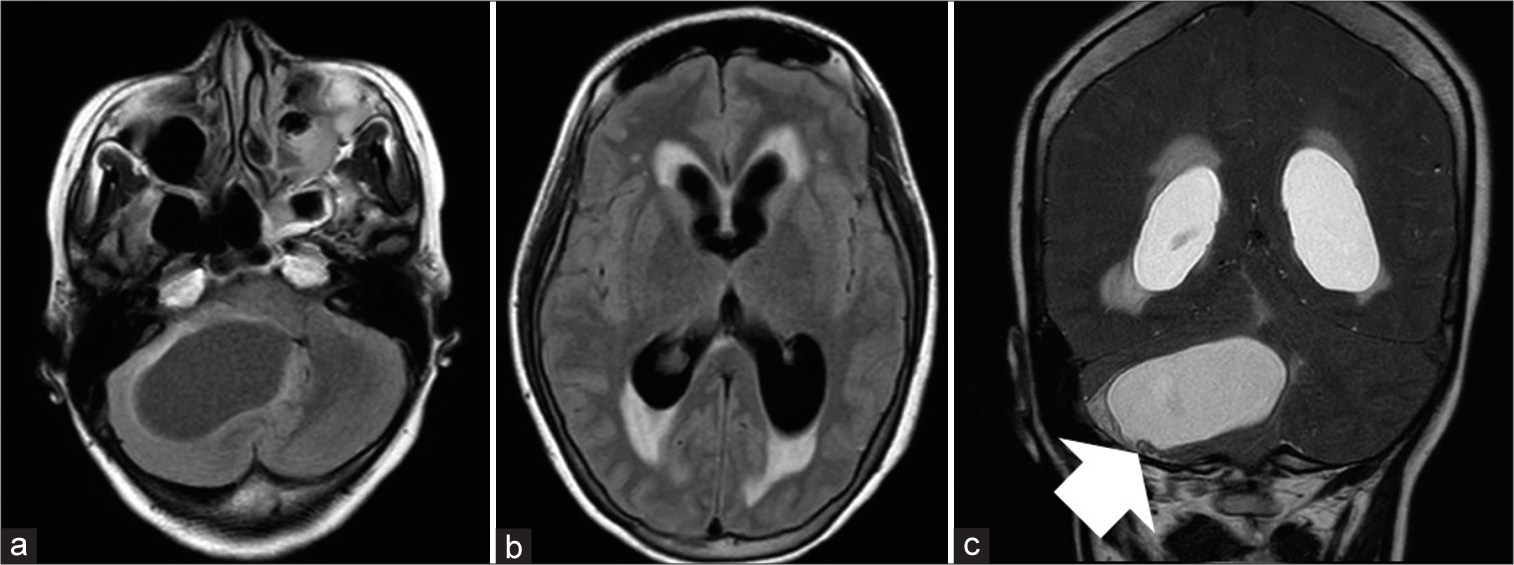
Brain magnetic resonance imaging (MRI) revealed a 5.6 cm cystic lesion with a mural nodule in the right cerebellar hemisphere and the lesion blocked cerebrospinal fluid drainage from the fourth ventricle and brainstem, resulting in obstructive hydrocephalus [
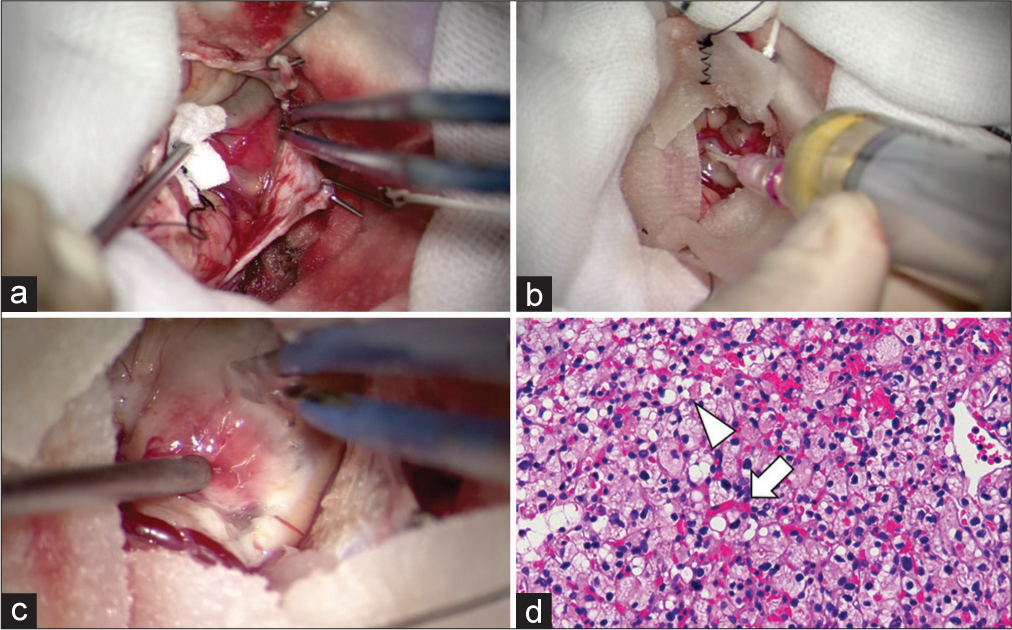
After obtaining the patient’s consent, a multidisciplinary team consisting of obstetricians and neurosurgeons decided to perform resection of the intracranial lesion following delivery of the fetus by emergency cesarean section in view of the symptoms of increased intracranial pressure. The patient underwent tumor resection through a suboccipital small craniotomy in the three-quarter position following external ventricular drainage. Indocyanine green video angiography showed the location of a vascular nodule thorough the dura and the mural nodule was identified directly underneath. Following cyst decompression and tumor resection without resecting cystic capsule, it was confirmed that the cerebellum had become slack and pulsation was observed [
Figure 2:
Intraoperative view showed that the dura was incised and a mural nodule was identified directly underneath (a). The tumor was punctured and the pale yellow contents were aspirated; internal decompression was performed (b). The mural nodule was removed as a mass without resecting the cystic capsule and it was confirmed that the cerebellum had become slack and pulsation was observed (c). Histopathological examination of the specimen revealed a rich vascular network (white arrow) and bubbly vacuolated cells with mild nuclear enlargement and clear cytoplasm (arrowhead) (d).
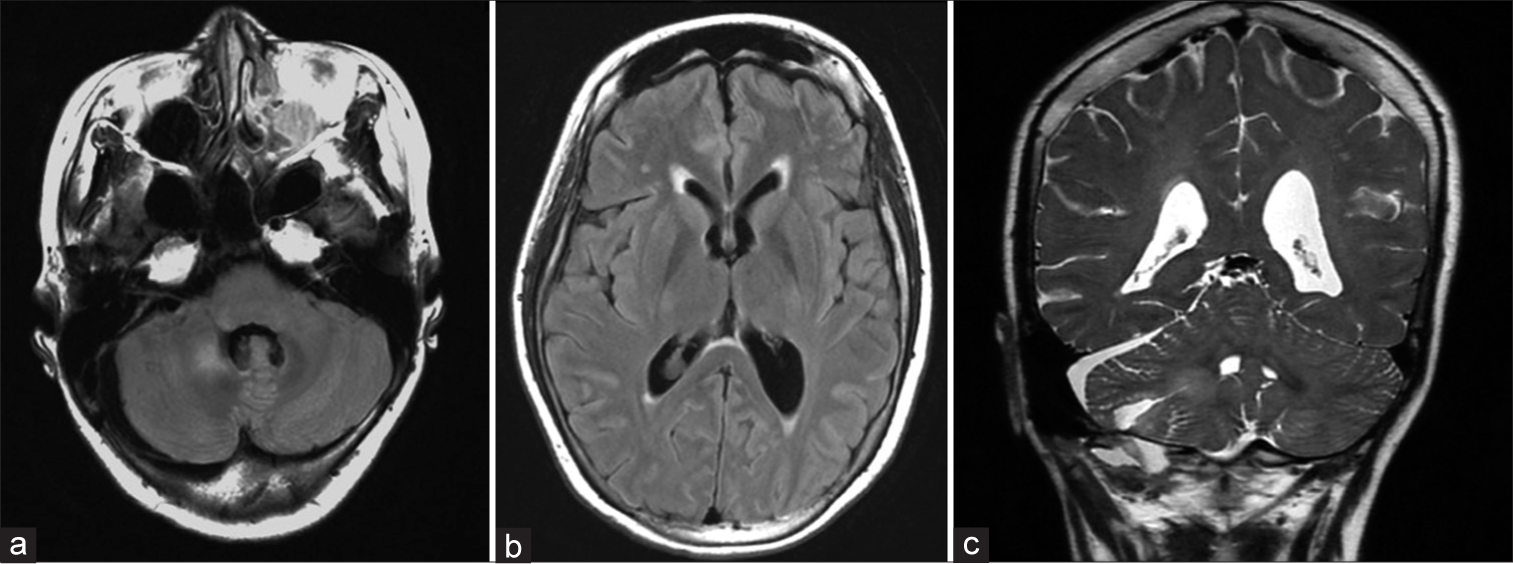
The patient recovered from general anesthesia and was extubated the next day. Postoperatively, the patient continued to experience dizziness and general malaise, but her symptoms resolved spontaneously with continued symptomatic treatment with oral medication. Postoperative brain MRI revealed that the tumor had been removed with no obvious residual tumor and the hydrocephalus had improved [
DISCUSSION
Mechanism of increase in the size of hemangioblastoma during pregnancy
Cerebellar hemangioblastoma is a benign vascular tumor and accounts for approximately 3% of all central nervous system tumors.[
Favorable management for hemangioblastoma during pregnancy
A variety of management options for hemangioblastoma occurring during pregnancy has been reported in the relevant literature, including conservative management with close observation, spinal fluid detour, and direct surgery. Conservative management with close observation is not a viable option for symptomatic patients because these conditions can deteriorate during pregnancy.[
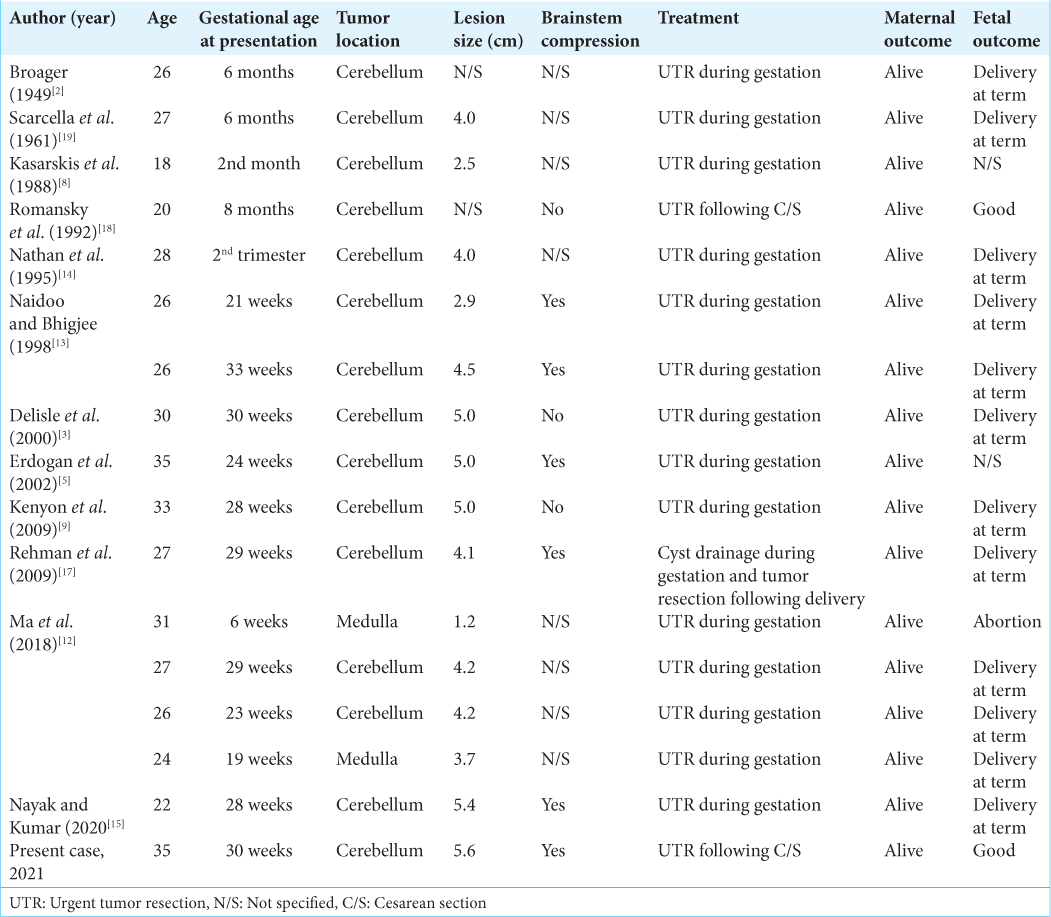
To date, there are a total of 12 English reports regarding direct surgical treatment of symptomatic hemangioblastomas during pregnancy in 16 cases, primarily in case reports or case series [
Based on the previous literature, six cases were reported with brainstem compression and three cases were reported without brainstem compression [
Overall, these reports suggest that direct surgery is a better option, especially in early pregnancy. Repeated general anesthesia and shunt-related complications during pregnancy can both be avoided. Moreover, in patients who present after 30–32 weeks of gestation, as in this case, combined of cesarean section and surgical resection of the tumor can be planned if fetal lung maturity is confirmed.[
Prognosis
The previous publications reported that most pregnant patients with hemangioblastoma during pregnancy experienced an uneventful gestational course [
CONCLUSION
We reported a case of symptomatic cerebellar hemangioblastoma during pregnancy and reviewed the literature. UTR combined with cesarean section can be planned once fetal lung maturity can be confirmed. A multidisciplinary discussion among neurosurgeons, anesthetists, and obstetricians is necessary to determine a treatment plan. Most cases of symptomatic hemangioblastoma during pregnancy have shown an uneventful gestational course and a favorable outcome for both mother and child.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Binderup ML, Budtz JE, Bisgaard ML. New von Hippel-Lindau manifestations develop at the same or decreased rates in pregnancy. Neurology. 2015. 85: 1500-3
2. Broager B. Multiple cerebellar angioreticulomas; discussion of high protein contents of the cysts and of enclosed parts of the subarachnoid space. Acta Psychiatr Neurol. 1949. 24: 317-32
3. Delisle MF, Valimohamed F, Money D, Douglas MJ. Central nervous system complications of Von Hippel-Lindau disease and pregnancy; perinatal considerations: Case report and literature review. J Matern Fetal Med. 2000. 9: 242-7
4. Drapkin AJ, Rose WS. Cerebellar hemangioblastoma during pregnancy. Neurosurgery. 1989. 24: 298-9
5. Erdogan B, Sen O, Aydin MV, Bagis T, Bavbek M. Cerebellar hemangioblastoma in pregnancy. A case report. J Reprod Med. 2002. 47: 864-6
6. Frantzen C, Kruizinga RC, van Asselt SJ, Zonnenberg BA, Lenders JW, de Herder WW. Pregnancy-related hemangioblastoma progression and complications in von Hippel-Lindau disease. Neurology. 2012. 79: 793-6
7. Glaäsker S, van Velthoven V. Risk of hemorrhage in hemangioblastomas of the central nervous system. Neurosurgery. 2005. 57: 71-6
8. Kasarskis EJ, Tibbs PA, Lee C. Cerebellar hemangioblastoma symptomatic during pregnancy. Neurosurgery. 1988. 22: 770-2
9. Kenyon AP, Haider S, Ashkan K, Nelson-Piercy C. Cerebellar haemangioblastoma presenting with dizziness in pregnancy: Case report and review of the literature. Obstet Med. 2009. 2: 164-7
10. Laviv Y, Wang JL, Anderson MP, Kasper EM. Accelerated growth of hemangioblastoma in pregnancy: The role of proangiogenic factors and upregulation of hypoxia-inducible factor (HIF) in a non-oxygen-dependent pathway. Neurosurg Rev. 2019. 42: 209-26
11. Lynch JC, Gouvea F, Emmerich JC, Kokinovrachos G, Pereira C, Welling L. Management strategy for brain tumour diagnosed during pregnancy. Br J Neurosurg. 2011. 25: 225-30
12. Ma XJ, Zhang GB, Guo TX, Li CB, Chen YJ, Zhang LW. Management and outcomes of pregnant patients with central nervous system hemangioblastoma. J Clin Neurosci. 2018. 57: 126-30
13. Naidoo K, Bhigjee AI. Multiple cerebellar haemangioblastomas symptomatic during pregnancy. Br J Neurosurg. 1998. 12: 281-4
14. Nathan L, Satin AJ, Twickler DM. Cerebellar hemangioblastoma complicating pregnancy. A case report. J Reprod Med. 1995. 40: 662-4
15. Nayak N, Kumar A. Cerebellar hemangioblastoma during pregnancy: Management options and review of literature. Surg Neurol Int. 2020. 11: 123
16. Ogasawara KK, Ogasawara EM, Hirata G. Pregnancy complicated by von Hippel-Lindau disease. Obstet Gynecol. 1995. 85: 829-31
17. Rehman T, Ali R, Yonas H. Cerebellar haemangioblastoma: Temporising treatment in a high risk pregnancy. BMJ Case Rep. 2009. 2009: bcr0120091413
18. Romansky K, Arnaudova V, Nachev S. Hemangioblastoma during pregnancy. Case report. Zentralbl Neurochir. 1992. 53: 37-9
19. Scarcella G, Allen MB, Andy OJ. Vascular lesions of the posterior fossa during pregnancy. Am J Obstet Gynecol. 1961. 82: 836-40
20. Signorelli F, Piscopo G, Giraud S, Guerriero S, Laborante A, Latronico ME. Von Hippel-Lindau disease: When neurosurgery meets nephrology, ophthalmology and genetics. J Neurosurg Sci. 2017. p. 63548-65
21. Wanebo JE, Lonser RR, Glenn GM, Oldfield EH. The natural history of hemangioblastomas of the central nervous system in patients with von Hippel-Lindau disease. J Neurosurg. 2003. 98: 82-94
22. Ye DY, Bakhtian KD, Asthagiri AR, Lonser RR. Effect of pregnancy on hemangioblastoma development and progression in von Hippel-Lindau disease. J Neurosurg. 2012. 117: 818-24