- Department of Surgery, Federal Medical Center, Abeokuta, Ogun, Nigeria
- Department of Surgery, College of Medicine, University of Lagos/Lagos University Teaching Hospital, Lagos, Nigeria.
Correspondence Address:
Bamidele Oludele Adebayo, Department of Surgery, Federal Medical Center, Abeokuta, Ogun, Nigeria.
DOI:10.25259/SNI_339_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Bamidele Oludele Adebayo1, Liadi Olanrewaju Tiamiyu1, Babatunde Adetunmbi1, Rilwan Omogbolahan Adegboyega1, Charles Oghenerukevwe Etagar1, Okezie Obasi Kanu2, Olufemi Bankole2. Female monozygotic twins with sacral myelomeningocele. 07-Jul-2023;14:234
How to cite this URL: Bamidele Oludele Adebayo1, Liadi Olanrewaju Tiamiyu1, Babatunde Adetunmbi1, Rilwan Omogbolahan Adegboyega1, Charles Oghenerukevwe Etagar1, Okezie Obasi Kanu2, Olufemi Bankole2. Female monozygotic twins with sacral myelomeningocele. 07-Jul-2023;14:234. Available from: https://surgicalneurologyint.com/surgicalint-articles/12396/
Abstract
Background: Concurrent myelomeningocele in twins is a rare clinical presentation, only reported twice in Nigeria.
Case Description: We present a set of identical female twins from Nigeria. Both twins were females that presented at 3 years with low back swelling since birth, associated with bisphincteric dysfunction but normal motor and sensory functions in the lower extremities. They had repair of myelomeningocele 2 months after presentation and there was no new deficit postoperatively.
Conclusion: This is the first reported case of identical twins with concurrent myelomeningocele and preserved motor functions in the lower limbs in Nigeria and West Africa.
Keywords: Monozygotic, Myelomeningocele, Twins
INTRODUCTION
Myelomeningocele is the most common congenital anomaly of the central nervous system and it is the most common type of spina bifida, with a worldwide incidence of 1/1000 live births. It is caused by failure of closure of the neural tube during embryonic development which results in a spinal cord that is open dorsally and forms a placode which lies on a meningeal sac at the back of the newborn.[
Myelomeningocele has a strong genetic component which is estimated at 60–70%. It has been reported that there is a higher concordance rate of neural tube defects (NTD) in same-sex twins compared to opposite-sex twins. The concordance rates for NTD from twin studies were 7.7% and 4.0% for monozygotic and dizygotic twins, respectively.[
We present the first set of identical twins with concurrent myelomeningocele from Nigeria that survived the perinatal period and have preserved motor functions in the lower extremities.
CASE REPORT
The patients were 3-year-old toddlers who presented with painless nonprogressive low back swelling since birth, associated with urinary and fecal incontinence but no gross motor deficit. The description of the mass at birth given by the mother was suggestive of a cystic mass with a placode which is typical of a myelomeningocele and it epithelialized over several weeks.
The twins were born at term through spontaneous vaginal delivery to a 35-year-old P5 + 0 uneducated food vendor in her second marriage. Mother had three children from a previous marriage and father had two children from a previous marriage, but there was no family history of NTD in first degree relatives. Mother did not take periconceptual folic acid and did not receive antenatal care. She was not diabetic nor did she have a history of use of antifolate drugs, exposure to radiation, and hyperthermia.
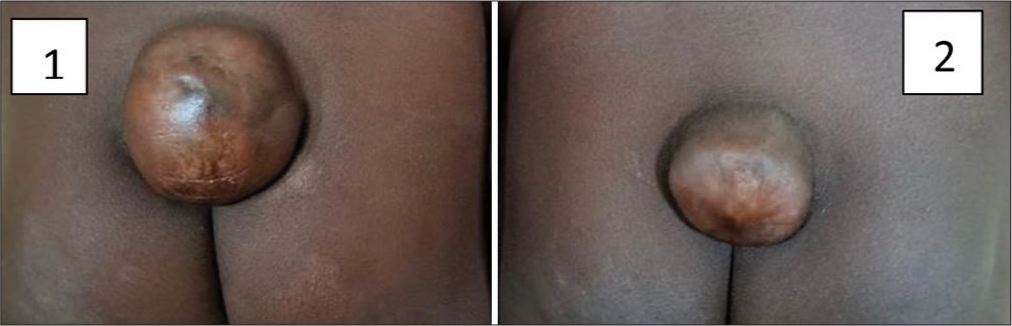
On examination, each twin had a sacral swelling covered with dysplastic skin at the center with normal skin at the periphery and there was no sinus or hairy patch on the swelling [
Both patients underwent repair of myelomeningocele under general anesthesia with endotracheal tube in prone position.
At surgery, the cord was directly attached to the epithelialized placode without any stalk.
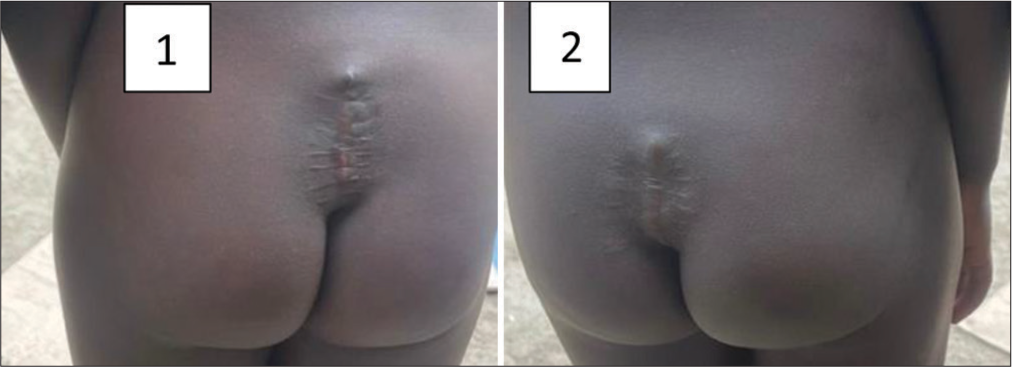
The cord was untethered from adhesion bands [
The toddlers had an uncomplicated postoperative period and were discharged 10 days after the operation, with no new neurologic deficit postoperatively.
Patients are 4-month postoperatively with healed wounds [
DISCUSSION
Myelomeningocele is characterized by protrusion of the meninges and spinal cord through an open vertebral arch and it is often associated with hydrocephalus, orthopedic disabilities, bowel, and bladder dysfunction.[
The specific cause of myelomeningocele is unknown, but pathogenesis is thought to be multifactorial and involve interplay of genetic and environmental factors. It has been reported that twinning predisposes to NTD and a higher rate of myelomeningocele has been observed in monozygotic twins compared with dizygotic twins.[
Folate deficiency in pregnancy is a major risk factor for NTD but other factors such as maternal use of drugs (valproic acid, carbamazepine, warfarin, and thalidomide), radiation exposure, maternal diabetes mellitus, maternal hyperthermia, mercury and lead exposures, as well as infections (rubella, cytomegalovirus, and toxoplasmosis) may impact the formation of NTD.[
In this report, we present the first set of identical twins with myelomeningocele in Nigeria. The first two reports in medical literature of myelomeningocele in monozygotic twins were by Wright in 1899 and Eskelund and Bartels in 1941, while the first report in dizygotic twins was by Fry in 1943.[
Rydnert et al. reported the first case of conjoined twins with myelomeningocele in 1985 from a hospital in Sweden.[
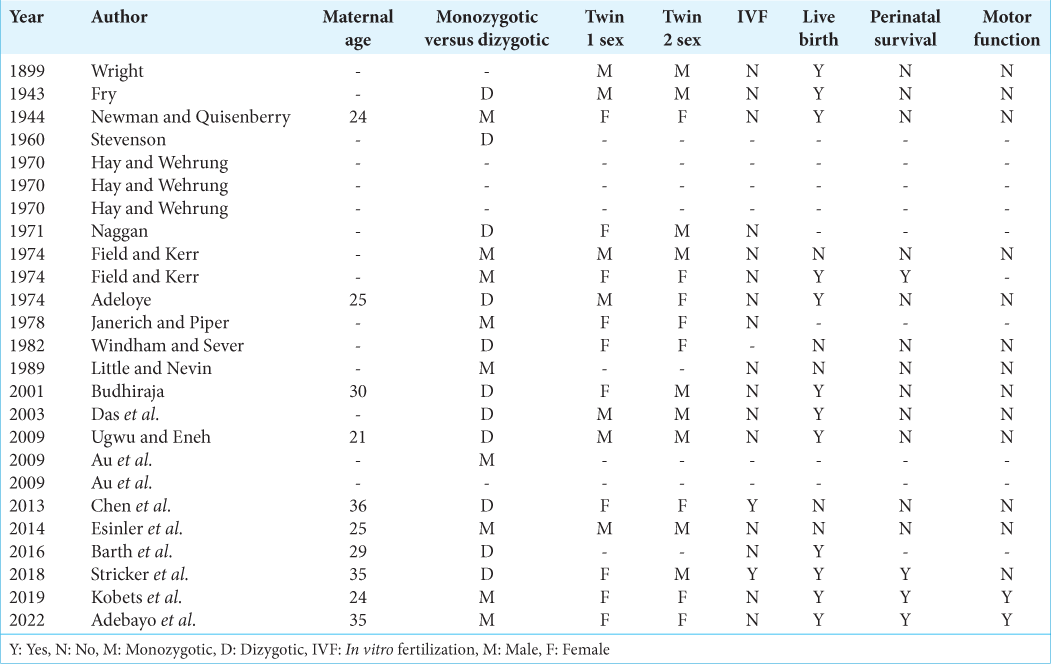
Table 1:
Review of all reported cases of concurrent twin myelomeningocele.[
The diagnosis of myelomeningocele can be made in utero or postnatally. Studies have shown that the best time to repair myelomeningocele is within the first 48 h of life, to prevent infection or neurological deterioration resulting from dehydration or stretching of the neural placode.[
Furthermore, repair within the first 72 h of life has been reported to improve the prognosis of neurogenic bladder compared with repair at a later time.[
However, intrauterine repair is possible in specialized centers and results suggest that fetal surgery leads to a reversal of hindbrain herniation (the Chiari II malformation), a decrease in shunt-dependent hydrocephalus, and possibly improvement in leg function.[
The main aim of the surgical treatment of myelomeningocele is to dissect the malformed area from the surrounding tissues and to create an adequate barrier above the spine to prevent infections and to preserve the residual motor and sensory functions.[
The most effective strategy worldwide for the prevention of NTD is folic acid supplementation at a dose of 0.36–0.8 mg daily for women who are planning or capable of pregnancy in the periconceptual period (atleast 1 month before conception and continues through the first 2–3 months of pregnancy).[
CONCLUSION
This is the first report of myelomeningocele in same-sex (female) identical twins in Nigeria and also the first to survive the perinatal period with full motor functions in the lower extremities in the world.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Adeloye A. Identical myelomeningoceles in a set of non-identical Nigerian twins. Ghana Med J. 1974. 1: 289
2. Adzick NS. Fetal myelomeningocele: Natural history, pathophysiology, and in-utero intervention. Semin Fetal Neonatal Med. 2010. 15: 9-14
3. Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM. Spina bifida. Nat Rev Dis Primers. 2015. 1: 15007
4. Deak KL, Siegel DG, George TM, Gregory S, Ashley-Koch A, Speer MC. Further evidence for a maternal genetic effect and a sex-influenced effect contributing to risk for human neural tube defects. Birth Defects Res A Clin Mol Teratol. 2008. 82: 662-9
5. De-Regil LM, Peña-Rosas JP, Fernández-Gaxiola AC, Rayco-Solon P. Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst Rev. 2015. 12: CD007950
6. Farmer DL, Thom EA, Brock JW, Burrows PK, Johnson MP, Howell LJ. Management of myelomeningocele study investigators. The management of myelomeningocele study: Full cohort 30-month pediatric outcomes. Am J Obstet Gynecol. 2018. 218: 256.e1-13
7. Fry A. Spina bifida in binovular twins. Br Med J. 1943. 1: 131-2
8. Kobets A, Lee RP, Oriko D, Jackson E, Robinson S, Cohen A. Dual myelomeningoceles in twins: Case report, review, and insights for etiology. Pediatr Neurosurg. 2020. 55: 363-73
9. Lee S, Gleeson JG. Closing in on mechanisms of open neural tube defects. Trends Neurosci. 2020. 43: 519-32
10. Mattogno PP, Massimi L, Tamburrini G, Frassanito P, Di Rocco C, Caldarelli M. Myelomeningocele repair: Surgical management based on a 30-year experience. Acta Neurochir Suppl. 2017. 124: 143-8
11. Meuli M, Moehrlen U. Fetal surgery for myelomeningocele is effective: A critical look at the whys. Pediatr Surg Int. 2014. 30: 689-97
12. Moldenhauer JS, Adzick NS. Fetal surgery for myelomeningocele: After the management of myelomeningocele study (MOMS). Semin Fetal Neonatal Med. 2017. 22: 360-6
13. Radcliff E, Cassell CH, Laditka SB, Thibadeau JK, Correia J, Grosse SD. Factors associated with the timeliness of postnatal surgical repair of spina bifida. Childs Nerv Syst. 2016. 32: 1479-87
14. Rydnert J, Holmgren G, Nielsen K, Bergman F, Joelsson I. Prenatal diagnosis of conjoined twins (diprosopus) with myelomeningocele. Acta Obstet Gynecol Scand. 1985. 64: 687-8
15. Tarcan T, Onol FF, Ilker Y, Alpay H, Simşek F, Ozek M. The timing of primary neurosurgical repair significantly affects neurogenic bladder prognosis in children with myelomeningocele. J Urol. 2006. 176: 1161-5
16. Ugwu RO, Eneh AU. Myelomeningocoele in dizygotic twins. Niger J Clin Pract. 2009. 12: 196-9
17. Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW. Folic acid supplementation for the prevention of neural tube defects: US preventive services task force recommendation statement. JAMA. 2017. 317: 183-9