- Department of Neurosurgery, Kyorin University Hospital, Mitaka, Tokyo, Japan.
- Department of Pathology, Kyorin University Hospital, Mitaka, Tokyo, Japan.
Correspondence Address:
Sukwoo Hong
Department of Neurosurgery, Kyorin University Hospital, Mitaka, Tokyo, Japan.
DOI:10.25259/SNI_504_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sukwoo Hong1, Keisuke Maruyama1, Ryo Hatanaka1, Akio Noguchi1, Hiroaki Shimoyamada2, Motoo Nagane1, Yoshiaki Shiokawa1. Frontotemporal dermoid cyst with incomplete dermal sinus tract in an adult: A case report. 11-Dec-2020;11:429
How to cite this URL: Sukwoo Hong1, Keisuke Maruyama1, Ryo Hatanaka1, Akio Noguchi1, Hiroaki Shimoyamada2, Motoo Nagane1, Yoshiaki Shiokawa1. Frontotemporal dermoid cyst with incomplete dermal sinus tract in an adult: A case report. 11-Dec-2020;11:429. Available from: https://surgicalneurologyint.com/surgicalint-articles/10447/
Abstract
Background: Non-midline supratentorial dermoid cyst with dermal sinus tract has been rarely reported especially in adults. We recently experienced a noteworthy patient with frontotemporal dermoid cyst with incomplete dermal sinus tract.
Case Description: A 43-year-old female presented with recurrent subcutaneous mass in the left superolateral orbital region. She had a history of active bronchial asthma, which precluded her from contrast-enhanced imaging studies. Plain imaging studies showed a subcutaneous mass which was continuous with an intrasylvian fissure mass by a tract in the sphenoid ridge and the lesser wing of the sphenoid bone. Frontotemporal craniotomy was performed to reset the mass and the tract. Intraoperative finding showed no intradural tumor components. Extradural component was carefully removed focusing attention on the frontal branch of the facial nerve. The pathology was consistent with dermoid cyst and dermal sinus tract. Postoperatively, she had mild facial palsy of the corrugator supercilii (House and Brackmann Grade II). She was discharged home with modified Rankin scale 1.
Conclusion: Dermoid cyst needs to be included in the differential diagnosis of adult-onset subcutaneous mass in the frontotemporal regions. After thorough imaging studies for the presence and extent of the sinus tract, the symptomatic lesion should be excised completely once and for all.
Keywords: Adult, Dermal sinus tract, Dermoid cyst, Frontotemporal, Pterion
INTRODUCTION
Dermoid cyst is typically a congenital benign tumor considered to be derived from abnormal ectodermal fusion[
CASE REPORT
History and examination
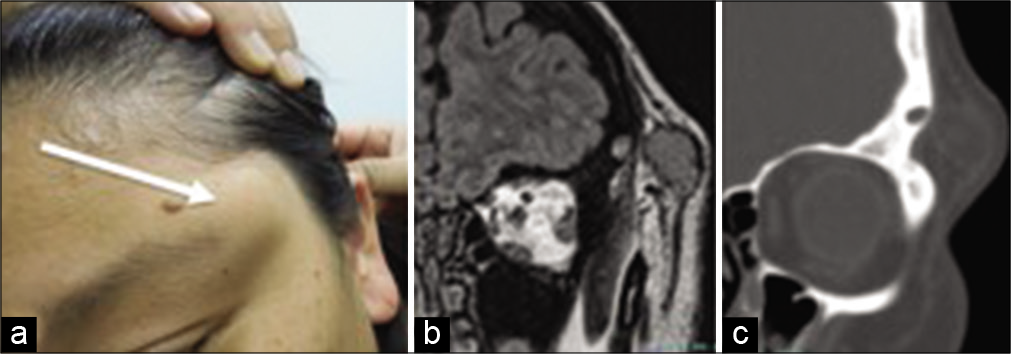
A 43-year-old female presented with recurrent subcutaneous mass in the left superolateral orbital region [
Figure 1:
Preoperative images of the recurrent dermoid cyst (a). Note the subcutaneous swelling in the superolateral orbital area (white arrow) Fluid attenuated inversion recovery MR imaging (coronal) showed a well-circumscribed extracranial tumor component of 22 mm in diameter (b). CT (coronal) showed a tract traversing through the sphenoid bone (c).
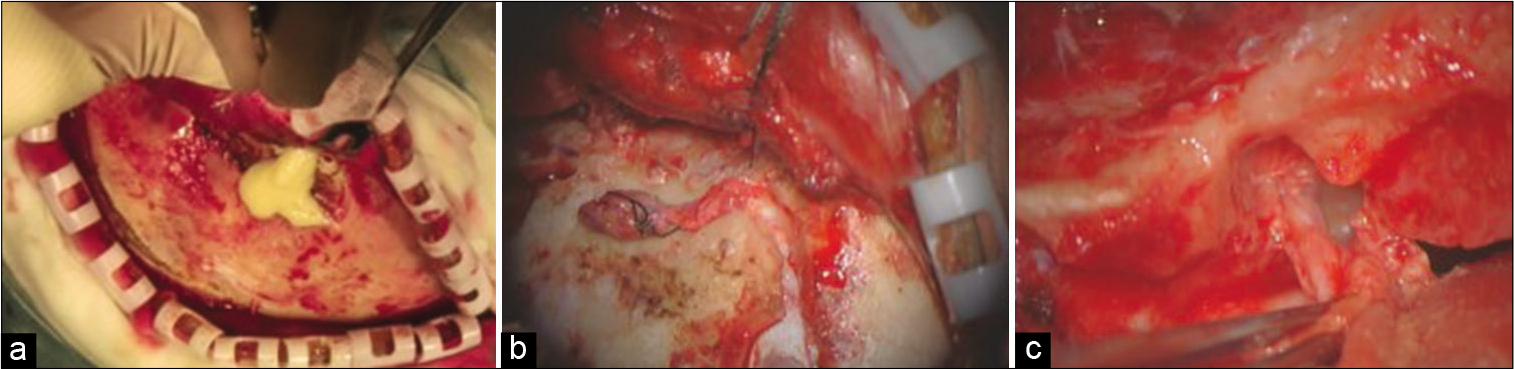
Surgical intervention
She underwent frontotemporal craniotomy. When musculocutaneous flap was retracted, the cyst duct was inadvertently damaged, resulting in spill out of greasy and whitish yellow cyst content [
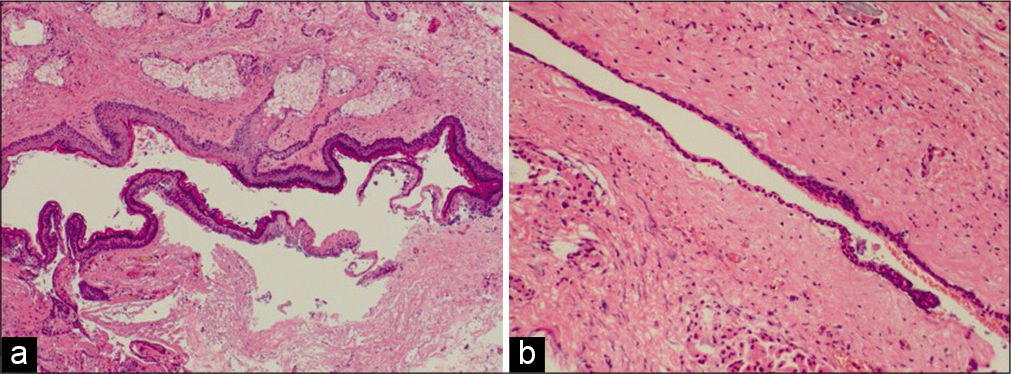
Histopathological findings
The resected specimens showed a cystic lesion filled with keratinized debris and a ductal structure which was connected to the cyst. The cyst wall was lined by a stratified squamous epithelium similar to epidermis. It contained adnexa of skin, such as sebaceous glands and sweat glands [
Figure 3:
A cystic lesion lined by an epidermal-like squamous epithelium contained several sebaceous glands, some of which continuous to the epithelium (a). A ductal structure, traversing through the sphenoid bone, was lined by a thin squamous epithelium with seldom keratinization (b). H&E: Hematoxylin and eosin; Original magnification ×40.
Postoperative course
The patient developed mild facial palsy of the corrugator supercilii. House and Brackmann grade was 2. She was discharged home 8 days after operation with modified Rankin scale of 1. At 6 months after the second surgery, she was free of recurrence clinically and radiologically.
DISCUSSION
A noteworthy case of subcutaneous dermoid cyst in the left superolateral orbital region accompanied by incomplete dermal sinus tract was described. Even though quite a few case reports have been made despite its rarity,[
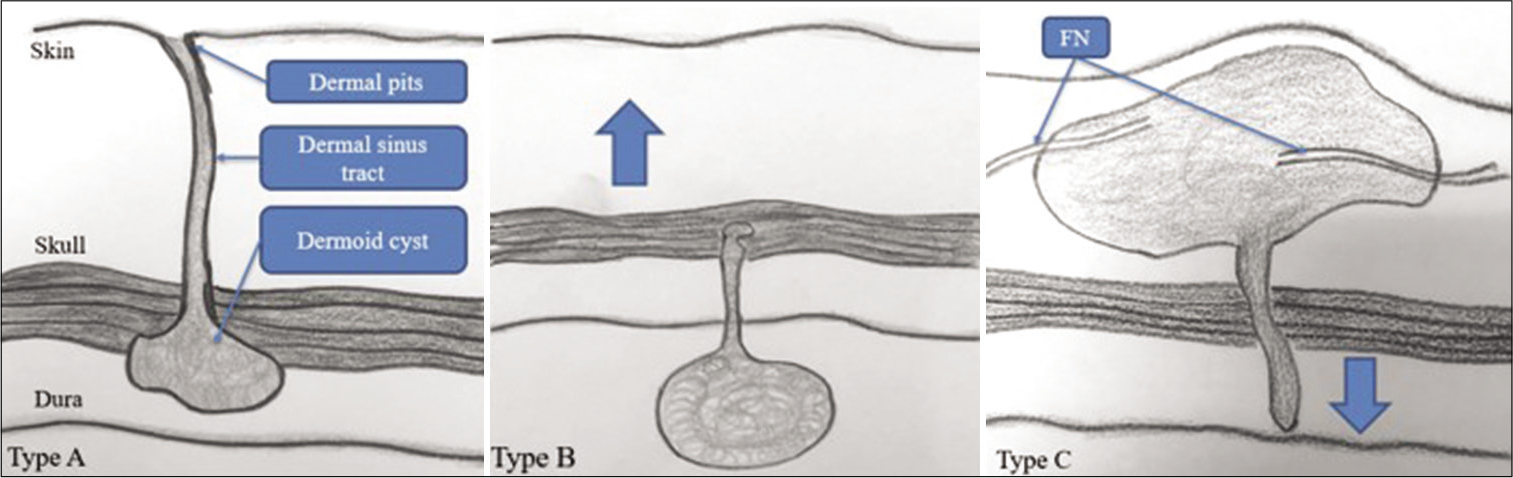
Based on these previous reports, we classified the dermoid cyst sinus tract complex into three types (types A, B, and C) [
Figure 4:
Dermoid cyst sinus tract complex is classified into three types based on the positional relationship of cyst and tract. In type A, the complete tract begins from the skin surface and the cyst is along the tract. Please note the relationship of the dermal pits, sinus tract and the cyst to the skin, skull, and the dura. Type B is the intradural dermoid cyst and the incomplete tract extending outward to the skin (arrow). Type C is the dermoid cyst and the incomplete sinus tract extending inward to the dura (arrow). In this type, the facial nerve (FN) branches may be around the cyst mass.
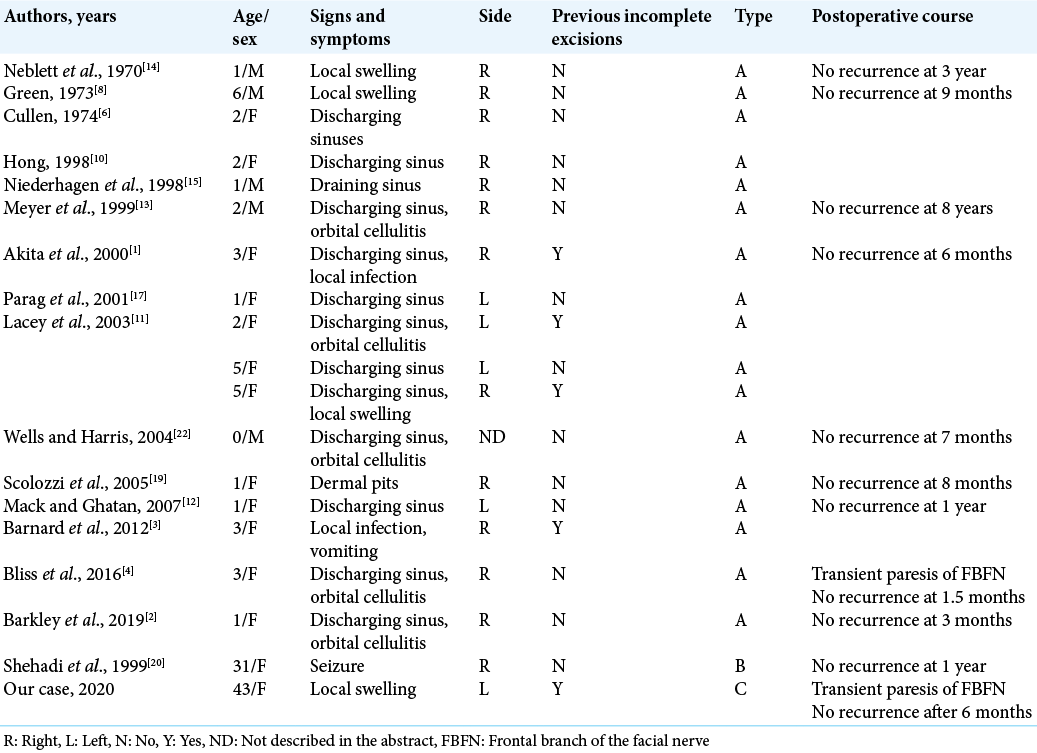
Table 1:
Past intracranial surgical reports on the frontotemporal dermoid cyst- sinus tract complex. All underwent complete excisions in the end and none recurred thereafter. Most of the cases were diagnosed in children and shared the same positional relationship of the cyst and the tract. The two unique adult cases were put in the lowest two rows for comparison.
Management strategy
Reviewing the literature, in Type A, where recurrent skin infections leads to the diagnosis in childhood, surgical excision of the lesion is the treatment of choice.[
CONCLUSION
Dermoid cyst needs to be included in the differential diagnosis of adult-onset subcutaneous mass in the frontotemporal regions. After thorough imaging studies for the presence and extent of the sinus tract, the symptomatic lesion should be excised completely once and for all.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akita S, Hirano A, Fujii T. Recurrent, discharging congenital frontotemporal dermoid cyst. Ann Plast Surg. 2000. 44: 465-6
2. Barkley AS, Susarla SM, Lee A. Frontotemporal dermal sinus tract with 2 connected intradiploic dermoid cysts: A rare case and review of the literature. World Neurosurg. 2019. 127: 350-3
3. Barnard AR, Jones AP, Hodgkinson PD, Jenkins AJ. Beware frontotemporal dermoids-they may have intracranial extension: A case of a middle cranial fossa cyst. J Plast Reconstr Aesthet Surg. 2012. 65: e185-8
4. Bliss M, Grant G, Tittler E, Loven T, Yeom KW, Sidell D. Diagnosis and treatment of pediatric frontotemporal pits: Report of 2 cases. J Neurosurg Pediatr. 2016. 18: 471-4
5. Chang JW, Yoon JS, Lee JH. The appropriate surgical approach to frontotemporal dermoid cysts in adult patients. Ann Plast Surg. 2017. 78: 54-8
6. Cullen JF. Orbital diploic dermoids. Br J Ophthalmol. 1974. 58: 105-6
7. Elton S, Oakes WJ. Dermal sinus tracts of the spine. Neurosurg Focus. 2001. 10: e4
8. Green MF. A lateral dermal sinus associated with an intradiploic cyst. Br J Plast Surg. 1973. 26: 298-300
9. Greenberg MS.editors. Handbook of Neurosurgery. Germany: Thieme; 2016. p.
10. Hong SW. Deep frontotemporal dermoid cyst presenting as a discharging sinus: A case report and review of literature. Br J Plast Surg. 1998. 51: 255-7
11. Lacey M, Gear AJ, Lee A. Temporal dermoids: Three cases and a modified treatment algorithm. Ann Plast Surg. 2003. 51: 103-9
12. Mack WJ, Ghatan S. Congenital pterional dermal sinus in an 18-month-old child: Case report. Neurosurgery. 2007. 61: E661
13. Meyer DR, Lessner AM, Yeatts RP, Linberg JV. Primary temporal fossa dermoid cysts. Characterization and surgical management. Ophthalmology. 1999. 106: 342-9
14. Neblett CR, Caram PC, Morris R. Lateral congenital dermal sinus tract associated with an intradiploic dermoid tumor. Case report. J Neurosurg. 1970. 33: 103-5
15. Niederhagen B, Reich RH, Zentner J. Temporal dermoid with intracranial extension: Report of a case. J Oral Maxillofac Surg. 1998. 56: 1352-4
16. Noguchi A, Shiokawa Y, Delahaw JB. Surgical anatomy for orbitozygomatic approach. No Shinkei Geka. 2010. 38: 703-13
17. Parag P, Prakash PJ, Zachariah N. Temporal dermoid-an unusual presentation. Pediatr Surg Int. 2001. 17: 77-9
18. Prior A, Anania P, Pacetti M, Secci F, Ravegnani M, Pavanello M. Dermoid and epidermoid cysts of scalp: Case series of 234 consecutive patients. World Neurosurg. 2018. 120: 119-24
19. Scolozzi P, Lombardi T, Jaques B. Congenital intracranial frontotemporal dermoid cyst presenting as a cutaneous fistula. Head Neck. 2005. 27: 429-32
20. Shehadi JA, Alorainy IA, Johnston KM. Temporal dermoid cyst with a partial dermal sinus tract. Can J Neurol Sci. 1999. 26: 321-4
21. Vega RA, Hidlay DT, Tye GW, Fuller CE, Rhodes JL. Intradiploic dermoid cyst of the lateral frontotemporal skull: Case report and review of the literature. Pediatr Neurosurg. 2013. 49: 232-5
22. Wells TS, Harris GJ. Orbital dermoid cyst and sinus tract presenting with acute infection. Ophthalmic Plast Reconstr Surg. 2004. 20: 465-7






Maruyama K
Posted December 11, 2020, 11:10 pm
Congratulations for online publication!
I am looking forward to your continuous academic activities!