- Department of Neurosurgery, Mayo Clinic Alix School of Medicine, Arizona, United States.
- Department of Neurosurgery, Mayo Clinic AZ, Phoenix, Arizona, United States.
Correspondence Address:
Sarah A. Merrill
Department of Neurosurgery, Mayo Clinic AZ, Phoenix, Arizona, United States.
DOI:10.25259/SNI_689_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sarah A. Merrill1, Daniel Khan1, Alexandra E. Richards2, Maziyar A. Kalani2, Naresh P. Patel2, Matthew T. Neal2. Functional recovery following surgery for chronic subdural hematoma. 22-Dec-2020;11:450
How to cite this URL: Sarah A. Merrill1, Daniel Khan1, Alexandra E. Richards2, Maziyar A. Kalani2, Naresh P. Patel2, Matthew T. Neal2. Functional recovery following surgery for chronic subdural hematoma. 22-Dec-2020;11:450. Available from: https://surgicalneurologyint.com/surgicalint-articles/10474/
Abstract
Background: Among the elderly, chronic subdural hematoma is a relatively common neurosurgical condition. Presenting symptoms range from headache and focal neurological deficits to seizure and coma depending on location and extent of brain compression. Functional recovery following surgery for chronic subdural hematoma is central to quality of life and ongoing health for elderly patients; however, there is a paucity of data regarding functional recovery in this population.
Methods: In this study, the physical activity of patients who underwent surgical evacuation of chronic subdural hematoma was surveyed, as well as participation in physical therapy following surgery. In total, 38 patients completed the survey.
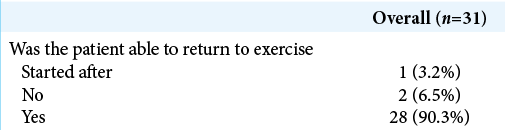
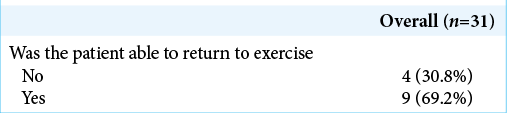
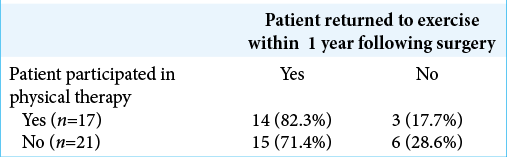
Results: Of the 30 patients who exercised regularly before surgery, 28 (90.3%) returned to exercise within 1 year after surgery. Of 13 patients who reported playing hobby sports before surgery, 9 (69.2%) returned to those sports. 17/38 (44.7%) patients participated in physical therapy after surgery. 35/38 (92.1%) of patients reported that the surgery improved their quality of life.
Conclusion: The majority of patients who underwent surgery for chronic subdural hematoma were able to return to exercise within 1 year. Participation in physical therapy was associated with return to exercise and sports. Further study is needed to determine which factors contribute to a return to baseline levels of physical activity following surgery for chronic subdural hematoma.
Keywords: Chronic, Exercise, Neurosurgery, Neurovascular, Physical therapy, Subdural hematoma
INTRODUCTION
Chronic subdural hematoma (cSDH) is a common disease process encountered in neurosurgery. Reported incidence of cSDH is between 1.72 and 20.6/100,000 persons per year across the study populations, with an increased incidence in patients over 60 years of age.[
Surgical evacuation of cSDH is generally performed through craniotomy or burr holes, with or without external drain placement. Following surgical evacuation, clinical status improvement rates are high, although oftentimes patients do not return to baseline before discharge.[
MATERIALS AND METHODS
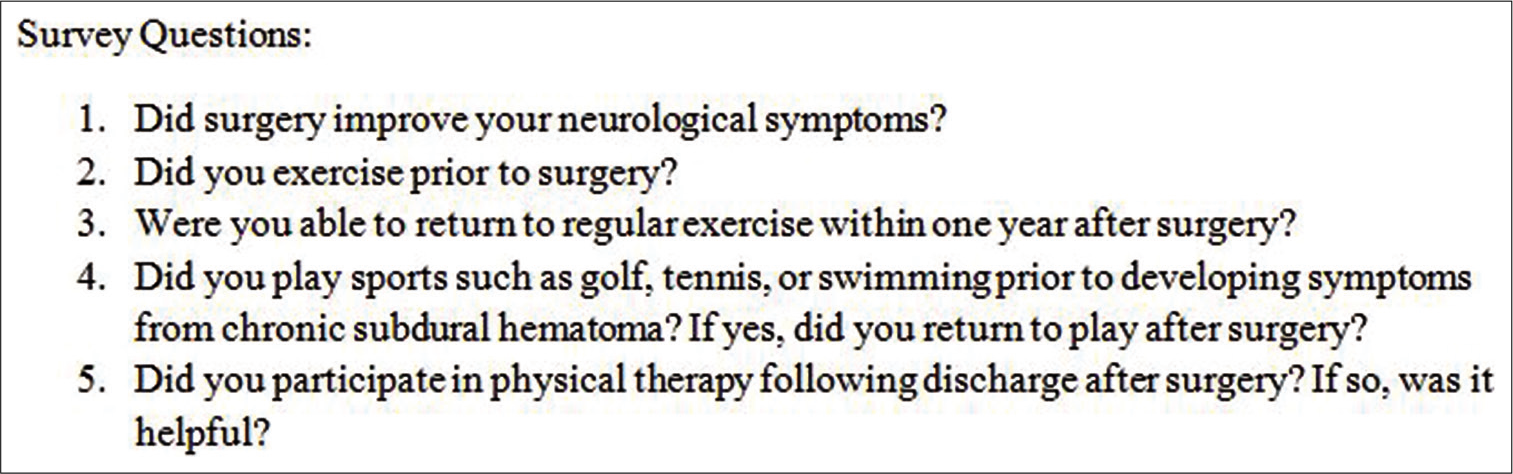
We identified all patients treated surgically for cSDH at our institution between January 1, 2014, and December 31, 2018, through CPT codes. Eligible participants received a phone call to participate in a five-question survey regarding their recovery following surgery for cSDH. The survey included questions regarding symptom improvement after surgery, participation in exercise or hobby sports before surgery, and return to exercise or hobby sports following surgery. We also inquired if the patients participated in physical therapy after surgery, and if they found that participation helpful [
RESULTS
Inclusion criteria included adults aged 18–89 that had surgical treatment for chronic subdural hematoma from January 1, 2014, to December 31, 2019. Patients were identified in a neurosurgery quality database. Exclusion criteria included patients who were discharged to hospice, died in hospital, required multiple surgical interventions for the cSDH, had greater than 50% acute SDH, or had concurrent intracranial hemorrhage other than SDH. Patients without phone contact information were also excluded. One patient was excluded due to having acute-on-chronic presentation. Of 90 total identified cSDH patients, 31 were deceased during the follow-up period, which is consistent with mortality rates in other published series,[
Of the 50 eligible patients, 38 consented to participate in the survey. Ten patients were female (26.3%); 28 were male (73.7%). Average age at time of surgery was 75 years old; range: 56–87. Average time between surgery and survey was 1362 days. The surgical approach used for 31 patients was burr hole drainage, while 7 patients were evacuated through craniotomy. No patients had external drains placed following burr hole craniotomies; however, drains are routinely placed following craniotomy procedures. Thirty-two of 38 patients had a GCS score of 15 before surgery. The remaining six patients had GCS 14 with point reduction due to confused speech.
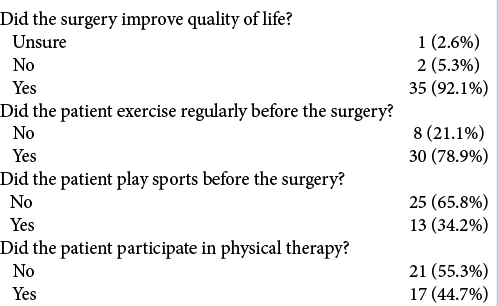
Of the participating patients, 35/38 (92.1%) reported that the surgery improved their neurologic symptoms and quality of life [
Before surgery, 13/38 (34.2%) participated in hobby sports such as golf, tennis, and swimming. Of those 13 patients, 9 (69.2%) returned to playing sports within 1 year following surgery [
DISCUSSION
Chronic subdural hematoma is a condition found most commonly in elderly patients, with incidence increasing with every decade past 60 years of age.[
Many studies on recovery following cSDH have focused on the acute hospitalization phase or the first 30 days after surgery. A systematic review by Chari et al. of 102 studies examining cSDH from 1990 to 2016 found only one study which examined outcome data at 18 months.[
While much has been written regarding survival, complications, and rates of recurrence following cSDH, little has been published regarding functional recovery and return to activity. A systematic review by Cunningham et al. found that a regular, moderate level of physical activity is associated with lower all-cause mortality and lower rates of falls, cognitive decline, dementia, and depression in patients aged 60 years and older.[
Physical therapy has been found to improve functional outcomes in elderly patients recovering from various neurosurgical procedures.[
Limitations and further study
As with all surveys, this study is subject to the limitations of recall bias. In addition, the rate of regular exercise before cSDH among older adults treated at our facility (78.9%) may be higher than rates in the general population; this generally higher baseline level of activity may influence rates of return to exercise following surgery. It is also possible that some or all of the 13 patients who did not participate in the survey may have suffered poor outcomes. In this case, the percentage of patients who returned to sport or regular exercise would be falsely elevated.
This study highlights the need for additional research on this topic, including better prognostication about recovery after cSDH so that we can better educate patients and families. Further study is required to illuminate the factors contributing to high functional activity levels following surgical evacuation and to elucidate the optimal role, duration, and timing for physical therapy during recovery from cSDH.
CONCLUSION
In our small cohort, we found that surgery improved symptoms and allowed the majority of our patients to return to exercise within one year after surgery. Participation in a physical therapy program was positively associated with return to exercise. Further study is needed to determine which factors contribute to a return to baseline levels of physical activity following surgery for chronic subdural hematoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Baechli H, Nordmann A, Bucher HC, Gratzl O. Demographics and prevalent risk factors of chronic subdural haematoma: Results of a large single-center cohort study. Neurosurg Rev. 2004. 27: 263-6
2. Bartek J, Sjavik K, Dhawan S, Sagberg LM, Kristiansson H, Ståhl F. Clinical course in chronic subdural hematoma patients aged 18-49 compared to patients 50 years and above: A multicenter study and meta-analysis. Front Neurol. 2019. 10: 311
3. Bergmann M, Puskas Z, Kuchelmeister K. Subdural hematoma due to dural metastasis: Case report and review of the literature. Clin Neurol Neurosurg. 1992. 94: 235-40
4. Chari A, Hocking KC, Edlmann E, Turner C, Santarius T, Hutchinson PJ. Core outcomes and common data elements in chronic subdural hematoma: A systematic review of the literature focusing on baseline and peri-operative care data elements. J Neurotrauma. 2016. 33: 1569-75
5. Chen JC, Levy ML. Causes, epidemiology, and risk factors of chronic subdural hematoma. Neurosurg Clin N Am. 2000. 11: 399-406
6. Cunningham C, R OS, Caserotti P, Tully MA. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand J Med Sci Sports. 2020. 30: 816-27
7. DeJong G, Hsieh CH, Putman K, Smout RJ, Horn SD, Tian W. Physical therapy activities in stroke, knee arthroplasty, and traumatic brain injury rehabilitation: Their variation, similarities, and association with functional outcomes. Phys Ther. 2011. 91: 1826-37
8. Fomchenko EI, Gilmore EJ, Matouk CC, Gerrard JL, Sheth KN. Management of subdural hematomas: Part I. Medical management of subdural hematomas. Curr Treat Options Neurol. 2018. 20: 28
9. Gazzeri R, Laszlo A, Faiola A, Colangeli M, Comberiati A, Bolognini A. Clinical investigation of chronic subdural hematoma: Relationship between surgical approach, drainage location, use of antithrombotic drugs and postoperative recurrence. Clin Neurol Neurosurg. 2020. 191: 105705
10. Gillett G. Subdural hematoma. Camb Q Healthc Ethics. 2017. 26: 527-9
11. Kuan-Yin T, Dueng-Yuan H, Hsin IM. Subdural hematoma associated with skull and dural metastasis of gastric carcinoma: A case report. Turk Neurosurg. 2013. 23: 796-9
12. Miranda LB, Braxton E, Hobbs J, Quigley MR. Chronic subdural hematoma in the elderly: Not a benign disease. J Neurosurg. 2011. 114: 72-6
13. Rauhala M, Helen P, Seppa K, Huhtala H, Iverson GL, Niskakangas T. Long-term excess mortality after chronic subdural hematoma. Acta Neurochir (Wien). 2020. 162: 1467-78
14. René O, Martin H, Pavol S, Kristián V, Tomáš F, Branislav K. Factors influencing the results of surgical therapy of non-acute subdural haematomas. Eur J Trauma Emerg Surg. 2019. p.
15. Sottile PD, Nordon-Craft A, Malone D, Luby DM, Schenkman M, Moss M. Physical therapist treatment of patients in the neurological intensive care unit: Description of practice. Phys Ther. 2015. 95: 1006-14
16. Stippler M, Ramirez P, Berti A, Macindoe C, Villalobos N, Murray-Krezan C. Chronic subdural hematoma patients aged 90 years and older. Neurol Res. 2013. 35: 243-6
17. Yang W, Huang J. Chronic subdural hematoma: Epidemiology and natural history. Neurosurg Clin N Am. 2017. 28: 205-10






Demao Cao
Posted January 21, 2021, 6:14 pm
Thank you for your work first. CSDH is really an interesting disease,the functional recovery after operation is important for the patients.But we still don’t know which reason facilitate it, and are there some differences between the patients with TBI and without TBI?