- Department of Neurosurgery, Lenox Hill Hospital, New York, United States.
DOI:10.25259/SNI_556_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yafell Serulle, Deepak Khatri, Jada Fletcher, Anna Pappas, Audrey Heidbreder, David Langer, Rafael A. Ortiz. Fusiform superior cerebellar artery aneurysm treated with flow diversion: A case report. 08-Oct-2020;11:330
How to cite this URL: Yafell Serulle, Deepak Khatri, Jada Fletcher, Anna Pappas, Audrey Heidbreder, David Langer, Rafael A. Ortiz. Fusiform superior cerebellar artery aneurysm treated with flow diversion: A case report. 08-Oct-2020;11:330. Available from: https://surgicalneurologyint.com/surgicalint-articles/10317/
Abstract
Background: Fusiform aneurysms of the distal superior cerebellar artery are rare and challenging to treat. Due to the rarity of these lesions, there is little consensus regarding their management. Treatment options have traditionally included parent artery sacrifice with either an endovascular approach or microsurgical clipping. Given the small diameter of the superior cerebellar artery, flow diversion has not been typically considered as a viable treatment option for these aneurysms.
Case Description: A 67-year-old female presented complaining of severe sudden onset headache. Noncontrast head CT demonstrated no intracranial hemorrhage. Head CT angiogram demonstrated a 4.2 mm fusiform aneurysm in the distal right superior cerebellar artery. The patient underwent treatment with the Pipeline embolization device which was deployed in the right superior cerebellar artery covering the aneurysm. Six-month posttreatment follow-up angiogram demonstrated resolution of the aneurysm with patency of the parent vessel.
Conclusion: To the best of our knowledge, this is the first report of a distal superior cerebellar artery aneurysm treated with the Pipeline embolization device. The use of a Pipeline stent to create flow diversion should be considered in a case of a fusiform aneurysm of the right superior cerebellar artery. Treatment with flow diversion may allow for the treatment of the aneurysm while preserving patency of the parent vessel.
Keywords: Aneurysm, Endovascular, Flow diversion, Fusiform, Pipeline
INTRODUCTION
Aneurysms of the vertebrobasilar system comprise fewer than 10% of all intracranial aneurysms. Among the posterior circulation aneurysms, superior cerebellar aneurysms (SCAs) are rare and account for 1.7% of all treated intracranial aneurysms, with the most typical location being the junction of the basilar artery and SCA.[
Fusiform aneurysms of the distal SCA are particularly challenging to treat. Treatment options for these aneurysms have typically consisted of parent artery sacrifice with either endovascular means or microsurgical clipping with or without bypass.[
CASE DESCRIPTION
A 67-year-old female with a medical history of hypertension and active smoking presented to the emergency department after experiencing a severe headache of sudden onset in the right side of her head. The patient had undergone elective screening colonoscopy the day prior. The morning following the colonoscopy procedure she woke up experiencing a right-sided headache associated with nausea, right-arm pain, right eye blurry vision, and slight fingertip numbness on her right side after which she decided to come to the hospital. She denied any recent trauma, fever, chills, or neck stiffness. On physical examination, she was neurologically intact.
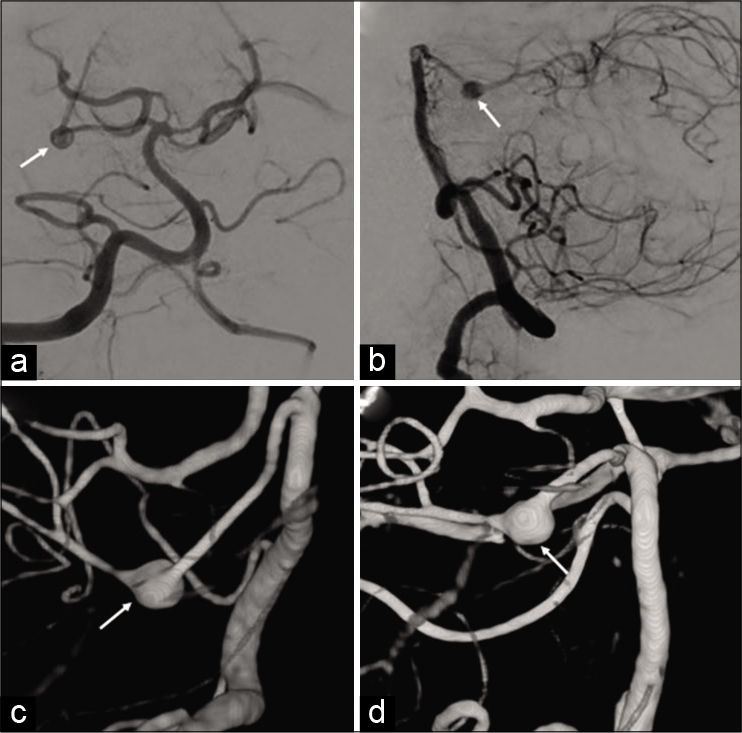
Noncontrast head CT demonstrated no acute intracranial pathology, specifically no evidence of subarachnoid hemorrhage. CT angiogram (CTA) demonstrated a 4.2 × 4.2 × 4.2 mm fusiform aneurysm arising off the superior cerebellar artery, approximately 1.5 cm distal to its origin off the basilar artery. The headache subsided the following day. Diagnostic cerebral angiogram was performed and redemonstrated the fusiform aneurysm, essentially unchanged in appearance when compared to the CTA [
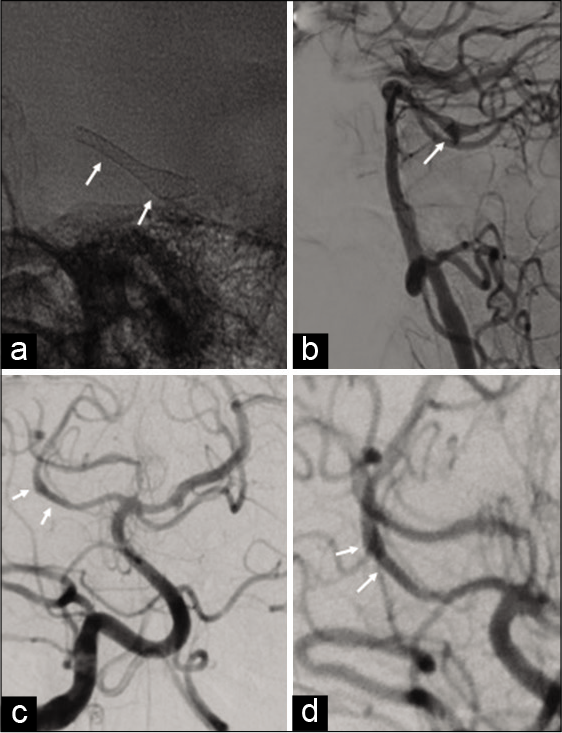
Figure 2:
Native image (a) during the deployment of the Pipeline embolization device (PED) demonstrating the device already deployed (arrows). (b) Lateral digital subtraction angiography performed immediately following the deployment of the PED demonstrates contrast stagnation within the aneurysm and patency of the parent vessel. Six-month angiographic follow-up (c and d) demonstrates resolution of the aneurysm with patency of the superior cerebellar artery (arrows).
The patient was neurologically intact postoperatively and was discharged home on postoperative day 2. A cerebral angiogram performed 6 months later demonstrated resolution of the aneurysm with patency of the superior cerebellar artery [
DISCUSSION
Fusiform or dissecting aneurysms affecting the distal segments of the superior cerebellar artery are a rare entity. Review of the previous cases suggests that subarachnoid hemorrhage is the most common mode of presentation, however, a myriad of clinical symptoms including cerebellar infarction or brainstem ischemia, hemifacial paralysis with hemiplegia, diplopia with ocular dysmotility due to trochlear nerve dysfunction, and sudden onset torticollis has also been reported previously.[
We explored both open and endovascular approaches for the treatment of this aneurysm. Open microsurgical techniques to treat distal SCA aneurysms include clipping of the aneurysm, wrapping the aneurysm to induce wall fibrosis, parent vessel occlusion, and trapping the aneurysms with or without vascular bypass to restore the distal circulation. A deep anatomical location in the brain and proximity to the brainstem renders these aneurysms difficult to access surgically. In addition, the morbidity related to the craniotomy and skull base microsurgical approaches is relatively high.[
In contrast to the surgical approaches, an endovascular technique offers a more direct access to these aneurysms for treatment. Occlusion of the parent vessel through endovascular coil embolization has been a commonly utilized technique for fusiform aneurysms involving very small diameter arteries, such as the superior cerebellar artery.[
Perforator infarction is a well-known complication of flow diverter treatment and can potentially lead to devastating consequences.[
Vessel diameter plays a critical role while making the decision for flow diversion. A small vessel diameter poses a unique set of challenges to PED placement including difficulty in access as well as device placement, higher risk of kinking, vessel dissection, vasospasm, thrombosis, in-stent occlusion, and delayed ischemia due to intimal hyperplasia. Schob et al. successfully utilized Silk Vista Baby, a novel flow diverter, not yet available in the USA, with 2.25 mm and 2.75 mm diameter variants to treat 25 patients with small and distal vessel aneurysms arising from anterior communicating artery, pericallosal artery, and distal middle cerebral artery.[
The smallest PED available right now is 2.5 mm in diameter, which was the one used in this report.
Considering all the above-mentioned technical nuances and potential risk of procedure-related complications, the use of flow diverting stents for fusiform aneurysms of the distal SCA remains limited. On our literature review, we found only one case of a ruptured distal SCA dissecting aneurysm which was successfully treated using flow-diverting device placement. Authors successfully utilized a low-profile visualized intraluminal support (LVIS Jr.) device (MicroVention, Tustin, CA) to cover a left distal fusiform aneurysm measuring 3 mm × 18 mm in size.[
On our 6-month angiographic follow-up, there was resolution of the aneurysm. We did notice some vessel irregularity in the vessel, which was otherwise patent. The patient will be followed up with angiogram in another 6 months and then 1 year later to confirm the obliteration of the aneurysm and stent and vessel patency.
CONCLUSION
An effective obliteration of the aneurysm with preservation of the distal circulation is the ideal desirable goal for fusiform aneurysms. Flow diversion, though technically challenging in distal vessels with smaller diameter, can be considered for treatment in patients with distal SCA aneurysms. However, a detailed knowledge of the vascular anatomy and technical expertise in the procedure is warranted.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adeeb N, Griessenauer CJ, Dmytriw AA, Shallwani H, Gupta R, Foreman PM. Risk of branch occlusion and ischemic complications with the pipeline embolization device in the treatment of posterior circulation aneurysms. AJNR Am J Neuroradiol. 2018. 39: 1303-9
2. Alurkar A, Karanam LS, Nayak S, Oak S. Endovascular management of fusiform superior cerebellar artery aneurysms: A series of three cases with review of literature. J Clin Imaging Sci. 2012. 2: 47
3. Bender MT, Colby GP, Jiang B, Lin LM, Campos JK, Xu R. Flow diversion of posterior circulation cerebral aneurysms: A single-institution series of 59 cases. Neurosurgery. 2019. 84: 206-16
4. Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: A meta-analysis. Stroke. 2013. 44: 442-7
5. Hardy DG, Peace DA, Rhoton AL Jr. Microsurgical anatomy of the superior cerebellar artery. Neurosurgery. 1980. 6: 10-28
6. Irie Y, Takemoto K, Katsuta T, Fukuda K, Abe H, Iwaasa M. Distal superior cerebellar artery aneurysm located at the newly formed anastomotic site with the long circumferential artery of the posterior cerebral artery: A case report. Interv Neuroradiol. 2019. 25: 648-52
7. Jeon JB, Oh SY, Hyun DK, Shim YS. Fusiform superior cerebellar artery aneurysm treated with endovascular treatment. J Cerebrovasc Endovasc Neurosurg. 2016. 18: 276-80
8. Peluso JP, Van Rooij WJ, Sluzewski M, Beute GN. Superior cerebellar artery aneurysms: Incidence, clinical presentation and midterm outcome of endovascular treatment. Neuroradiology. 2007. 49: 747-51
9. Ros de San Pedro J. Retrosigmoid approach for trapping and removal of a distal dissecting superior cerebellar artery aneurysm in a child. J Neurol Surg B Skull Base. 2019. 80: S335-8
10. Schob S, Hoffmann KT, Richter C, Bhogal P, Köhlert K, Planitzer U. Flow diversion beyond the circle of Willis: Endovascular aneurysm treatment in peripheral cerebral arteries employing a novel low-profile flow diverting stent. J Neurointerv Surg. 2019. 11: 1227-34
11. Tahir R, Asmaro KP, Haider S, Kole M. Ruptured distal superior cerebellar artery dissecting aneurysm treated with a flow-diverting device: Case report and review of literature. Cureus. 2018. 10: e2918