- Department of Neurosurgery, Hospital Celso Pierro PUC-Campinas, Campinas, Brazil
- Department of Neurosurgery, Hospital Santa Paula, São Paulo, Brazil
Correspondence Address:
Maick Willen Fernandes Neves
Department of Neurosurgery, Hospital Celso Pierro PUC-Campinas, Campinas, Brazil
DOI:10.4103/sni.sni_18_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Maick Willen Fernandes Neves, Luis Otavio Carneiro Pontelli, Luiz Gustavo de Abreu Mattos, Mariana Mazzuia Guimarães, Telmo Augusto Barba Belsuzarri, Tiago Fernandes Gonçales, Wolnei Marques Zeviani, Paulo Henrique Pires de Aguiar, João Flavio Mattos Araújo. Giant mucopyocele associated with intracranial hypertension: Case report and literature review. 10-Oct-2017;8:242
How to cite this URL: Maick Willen Fernandes Neves, Luis Otavio Carneiro Pontelli, Luiz Gustavo de Abreu Mattos, Mariana Mazzuia Guimarães, Telmo Augusto Barba Belsuzarri, Tiago Fernandes Gonçales, Wolnei Marques Zeviani, Paulo Henrique Pires de Aguiar, João Flavio Mattos Araújo. Giant mucopyocele associated with intracranial hypertension: Case report and literature review. 10-Oct-2017;8:242. Available from: http://surgicalneurologyint.com/surgicalint-articles/giant-mucopyocele-associated-with-intracranial-hypertension-case-report-and-literature-review/
Abstract
Background:Mucoceles are epithelial lined sacs that contain mucous. Eventually, they can be infected and so called mucopyoceles, which are usually slow growing lesions with common bone destruction located in the facial sinus. Mucoceles show multivariate etiology and occur between the fourth and seventh decade of life.
Case Description:Patient, 55-year-old, female, was referred unconscious with Cushing's triad to our department; she had fever since four days. The findings of skull computer tomography highlighted a large bifrontal lesion with an invasion of the rear wall of the frontal sinus, compression of the frontal lobes, and midline deviation. She was taken for an emergency surgery, which showed invasion of the dura and mucous infection. Postoperatively, there was a fast recovery of neurologic level and extubation on the second postoperative day. She took antibiotics for 14 days and was discharged from the hospital without neurologic deficits.
Conclusions:Mucopyoceles are usually slow growing lesions that rarely increases rapidly. Our patient presented signs of intracranial hypertension; therefore, it was necessary to have quick surgical intervention.
Keywords: Complication, Cushing signs, intracranial hypertension, mucocele, mucopyocele, paranasal infection
INTRODUCTION
Mucocele is a chronic collection of mucous mostly located in the paranasal sinus of the face because of an inflammatory procedure, trauma, tumor, or surgical manipulation that obstructs the ostium of the sinus.[
CASE DESCRIPTION
Patient was a 55-year-old female with smoking history; she checked in the Medical Center with low level of conscience, fever, and headache for four days. She was comatose, bradycardic, and hypertensive; under these circumstances, she was submitted to orotracheal intubation owing to Glasgow Coma Scale (GCS) 6.
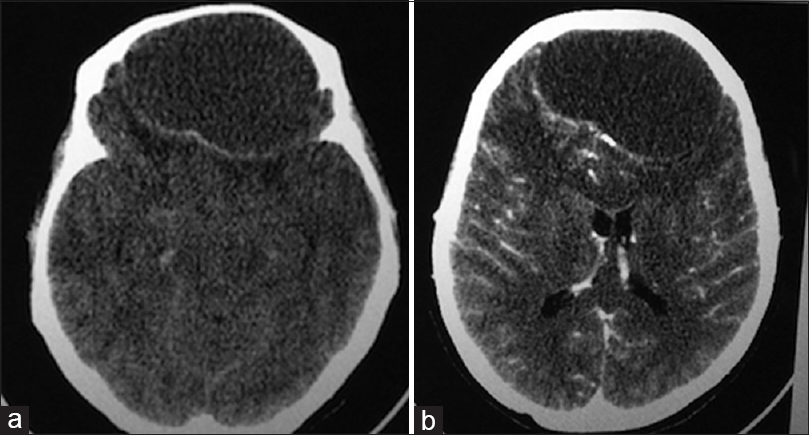
Urgent Computer Tomography (CT) scan highlighted extra-axial expansive lesion located in an anterior frontal region measuring 8.5 × 7 × 5 cm with homogenous and iso-hypodense content, compressing the bilateral frontal cerebral parenchyma, and thinning of the frontal bone with sclerotic margin [Figure
Treatment
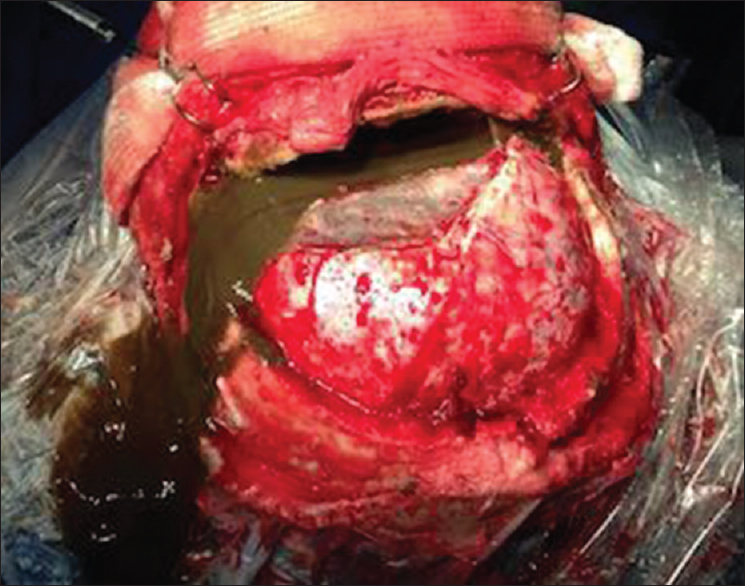
After CT scan, she was referred to the surgical center to emergency craniotomy for bifrontal expansive injury draining. Bicoronal incision was done followed by bifrontal craniotomy to access the extra-axial injury and frontal sinus [
During the surgical procedure, we observed greenish mucoid secretion associated with the presence of infection, dural laceration, and erosion of the frontal sinus (rear wall). The mucosa of the rear wall of the frontal sinus was scooped and covered by muscle.
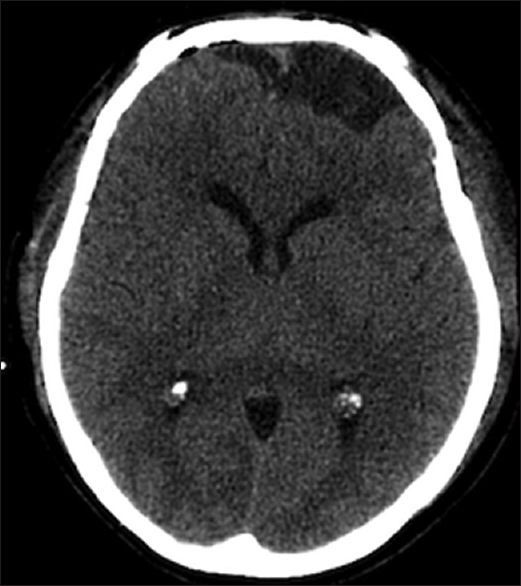
After the surgical procedure, the patient began the use of antibiotics, ceftriaxone, and metronidazole, which were taken for fourteen days. On the first postoperative day, the patient presented recovery of the level of conscience, being extubated on the second postoperative day and performed CT scan [
On the first postoperative day, a team of Ophthalmologists evaluated the eye and retina after surgery and did not find alterations. The patient was discharged from the hospital without neurologic deficits after the end of the antibiotics, with 6 months of follow up with no evidence of recurrence or new neurological deficits.
DISCUSSION
The destruction of the paranasal sinus is described in 10–20% of the mucopyoceles and it is contained by dura mater that is rarely penetrated by inflammation or tumor originated from the frontal sinus.[
We believe that the patient had mucocele for a long time as a result of erosion of the rear wall of the frontal sinus and invasion of dura mater, passing to present as headache and fever because of an infection that lasted for a short period. The infection caused increase of the lesion with compression of the frontal lobe and rear signs of intracranial hypertension.
Magnetic Resonance Imaging (MRI) of skull presented hypertension in T1 and T2, intra and extra cranial lesion, and intraorbital structures. The differential radiology diagnoses were dermoid cyst, histiocytosis, fungal infection, low-grade gliomas, and post-traumatic injury.[
The first treatment is the draining of accumulated secretion in the sinus and antibiotic therapy.[
An alternative surgical approach would be endoscopic surgery, which allows access to the frontal sinus and anterior cranial fossa. This access can be performed through transnasal approach, by orbit or even a combination of both access routes, adding versatility, a shorter surgical time, and an equal result.[
In the case presented, the patient had signs of intracranial hypertension, Cushing's triad; urgent CT scan was done to elucidate the diagnosis. We believe there was no time for MRI because of the signs of intracranial hypertension. The CT scan showed a significant lesion in a bilateral front region that justifies the clinical signs, which forced an emergency surgery. After the procedure, there was a clinical recovery that confirmed the diagnosis. The patient stayed under antibiotic for fourteen days due to an invasion of dura mater and purulent characteristic of the lesion in intra-operative, even though it showed negative cultures. Our infectology department made the decision for 2 weeks antibiotics due to the good resection of the mucopyocele with no intraoperative signs of osteomyelitis and negative bone cultures.
CONCLUSION
The mucopyeloceles have indolent growth and increased volume after infection, but rarely course with acute mass effect. Previous cases of mucopyocele associated to intracranial hypertension have not been mentioned in any literature. Thus, the case is relevant for literature due to the necessity of active intervention for better prognosis of the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Carmichael RA, Kang DR. Frontal Sinus Mucopyocele Presenting as a Subcutaneous Forehead Mass. J Oral Maxillofac Surg. 2015. 73: 2155-61
2. Chagla AS, Bhaganagare A, Kansal R, Tyagi D. Complete recovery of visual loss following surgical treatment of mucopyocele of the anterior clinoid process. J Clin Neurosci. 2010. 17: 670-2
3. El-Fiki ME, Abdel-Fattah HM, El-Deeb AK. Sphenoid Sinus Mucopyocele with Marked Intracranial Extension: A More Common Phenomenon in the Third World?. Surg Neurol. 1993. 39: 115-9
4. Joulali T, Derkaoui A, Shimi A, Khatouf M. Mucocèle frontale à extension orbito-cèrèbrale. Presse Med. 2014. 43: 1405-6
5. Kechagias E, Georgakoulias N, Ioakimidou C, Kyriazi S, Kontogeorgos G, Seretis A. Giant Intradural Mucocele in a Patient with Adult Onset Seizures. Case Rep Neurol. 2009. 1: 29-32
6. Koike Y, Tokoro K, Chiba Y, Suzuki SI, Murai M, Ito H. Intracranial extension of paranasal sinus mucocele: Two case reports. Surg Neurol. 1996. 45: 44-8
7. Kwon SH, Kim SH, Yoon JH. Anterior clinoid mucocele coexisting with sphenoid sinus mucocele. Auris Nasus Larynx. 2009. 36: 598-600
8. Lim JH, Sardesai MG, Ferreira M, Moe KS. Transorbital Neuroendoscopic Management of Sinogenic Complications Involving the Frontal Sinus, Orbit, and Anterior Cranial Fossa. J Neurol Surg Part B Skull Base. 2012. 73: 394-400
9. Lunardi P, Missori P, Di Lorenzo N, Fortuna A. Giant Intracranial Mucocele Secondary to Osteoma of the Frontal Sinuses: Report of Two Cases and Review of the Literature. Surg Neurol. 1993. 39: 46-8
10. Mundra RK, Gupta Y. Unusual Case of Frontoethmoid Mucopyocele with Intracranial and Orbital Extension. Indian J Otolaryngol Head Neck Surg. 2011. 63: 295-7
11. Van Manen SR, Bosch DA, Peeters FLM, Troost D. Giant intracranial mucocele. Clin Neurol Neurosurg. 1995. 97: 156-60
12. Weidmayer S. Frontal Mucocele with Intracranial Extension Causing Frontal Lobe Syndrome. Optomet Vis Sci. 2015. 92: 138-42