- Department of Neurosurgery, Ohkawara Neurosurgical Hospital, Muroran, Japan
- Department of Neurosurgery, Saitama Medical University International Medical Center, Hidaka, Japan.
Correspondence Address:
Takuma Maeda, Department of Neurosurgery, Ohkawara Neurosurgical Hospital, Muroran, Japan.
DOI:10.25259/SNI_351_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takuma Maeda1,2, Shiho Sakai1,2, Manabu Osakabe1, Mai Okawara1, Tatsufumi Nomura1, Hiroyuki Yamaguchi1, Takahiro Maeda1, Hiroki Kurita2. Giant saccular aneurysm of the cervical internal carotid artery treated with aneurysmectomy and side-to-end anastomosis. 08-Jun-2023;14:202
How to cite this URL: Takuma Maeda1,2, Shiho Sakai1,2, Manabu Osakabe1, Mai Okawara1, Tatsufumi Nomura1, Hiroyuki Yamaguchi1, Takahiro Maeda1, Hiroki Kurita2. Giant saccular aneurysm of the cervical internal carotid artery treated with aneurysmectomy and side-to-end anastomosis. 08-Jun-2023;14:202. Available from: https://surgicalneurologyint.com/surgicalint-articles/12353/
Abstract
Background: Cervical aneurysms are rare, accounting for
Case Description: The patient had experienced cervical pulsation and shoulder stiffness for 3 months. The patient had no significant medical history. An otolaryngologist performed the vascular imaging and referred the patient to our hospital for definitive management. Neurological deficits were not observed. Digital subtraction angiography showed a giant cervical aneurysm with a diameter of 25 mm within the ICA, and there was no evidence of thrombosis within the aneurysm. Aneurysmectomy and side-to-end anastomosis of the cervical ICA were performed under general anesthesia. After the procedure, the patient experienced partial hypoglossal nerve palsy but fully recovered with speech therapy. Postoperative computed tomography angiography revealed the complete aneurysm removal and patency of the ICA. The patient was discharged on postoperative day 7.
Conclusion: Despite several limitations, surgical aneurysmectomy and reconstruction are recommended to eliminate the mass effect and to avoid postoperative ischemic complications, even in the endovascular era.
Keywords: Aneurysmectomy, Cervical aneurysm, Reconstruction, Side-to-end anastomosis
INTRODUCTION
Aneurysms of the cervical internal carotid artery (ICA) are rare, accounting for <0.2–5% of all carotid operations and <1% of all arterial aneurysms.[
CASE REPORT
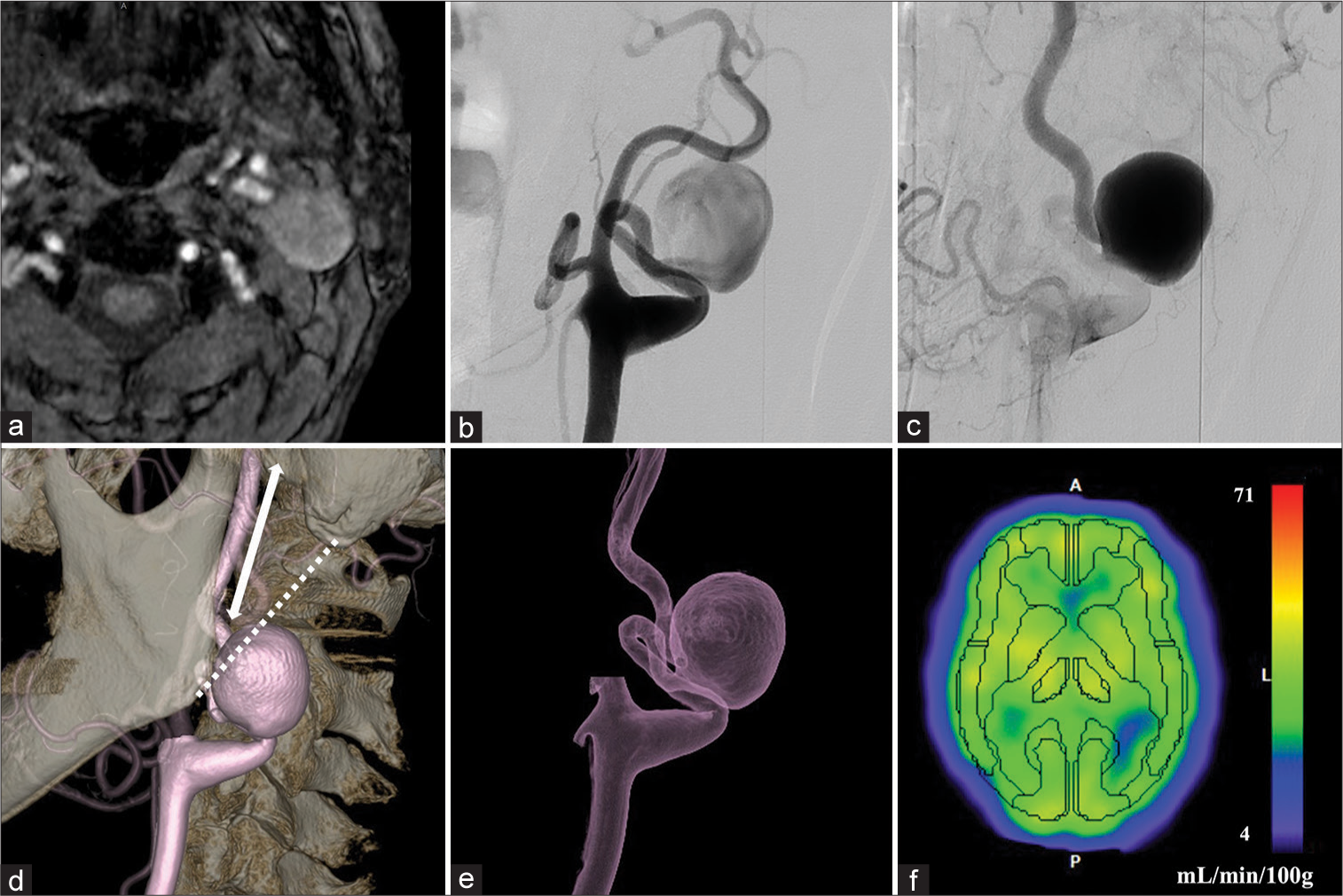
The patient was a 77-year-old man with no significant medical history. He had cervical pulsation and shoulder stiffness for 3 months, but neurological deficits were not observed. The patient was referred for a palpable swelling in the left cervical region. Magnetic resonance imaging performed on admission revealed a vascular lesion measuring 25 mm in diameter [
Figure 1:
Preoperative vessel imaging. Magnetic resonance image showing a vascular lesion in the left neck with a diameter of 25 mm (a). Digital subtraction angiograms in the early (b) and late (c) phases showing a giant saccular aneurysm of the cervical internal carotid artery (ICA) with the disturbance of blood flow. 3D-rotational angiogram showing the elongation and tortuosity of the vessel (d and e); the dotted line represents the Blaisdel line. The length of the distal ICA was 35 mm (double arrow). No hypoperfusion was observed on single-photon emission computed tomography images (f); the color bar represents the cerebral blood flow (mL/min/100g) of each individual voxel.
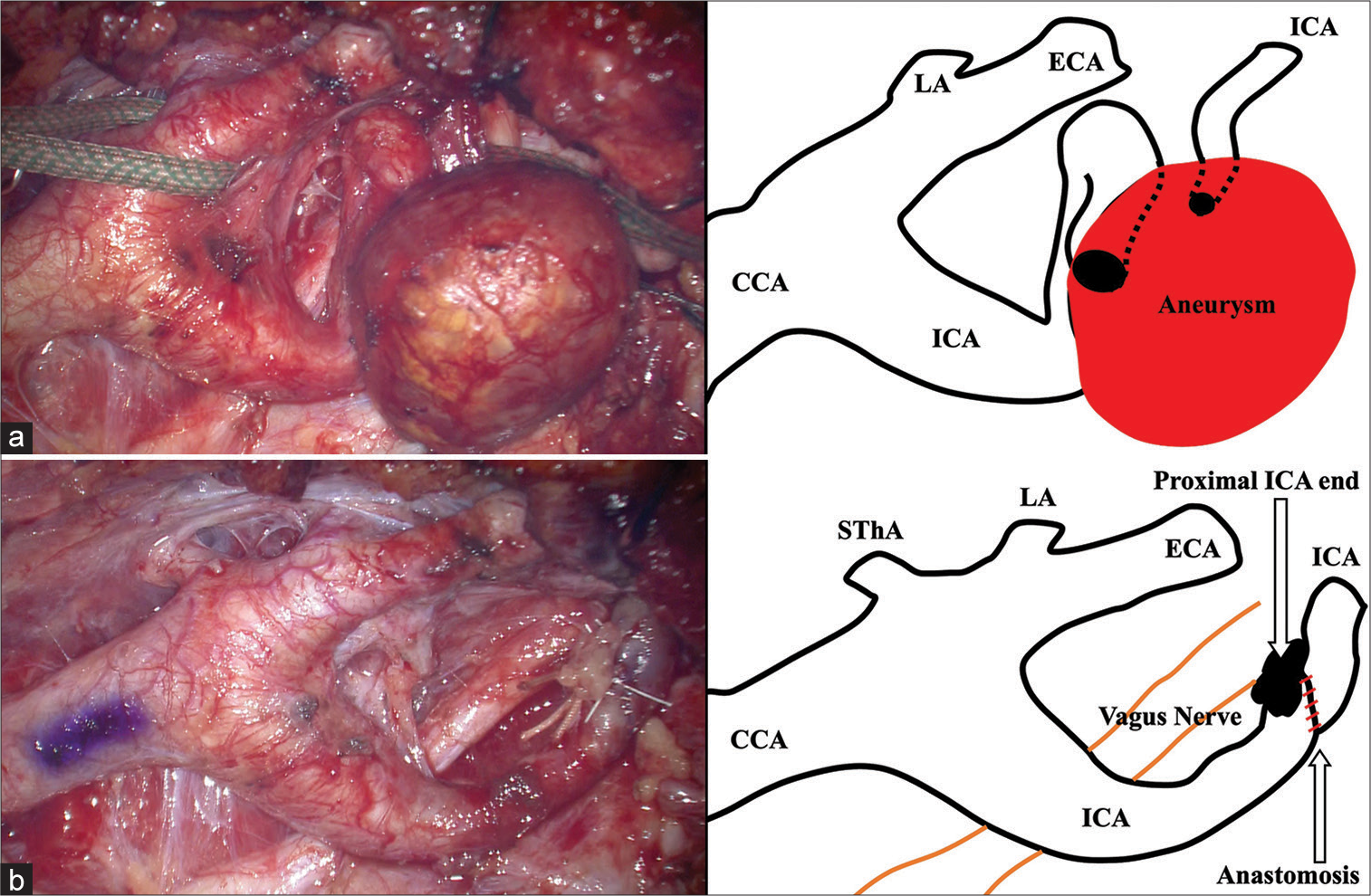
Under general anesthesia and motor-evoked potential (MEP), the aneurysm was excised, and side-to-end anastomosis of the cervical ICA was performed [
Figure 2:
Intraoperative images and schemes. Exposure of the aneurysm was performed through the standard approach along the anterior line of the sternocleidomastoid muscle (a), and aneurysmectomy and side-to-end anastomosis of the internal carotid artery were performed (b). CCA: Common carotid artery, ECA: External carotid artery, ICA: Internal carotid artery, LA: lingual artery, SThA: Superior thyroid artery.
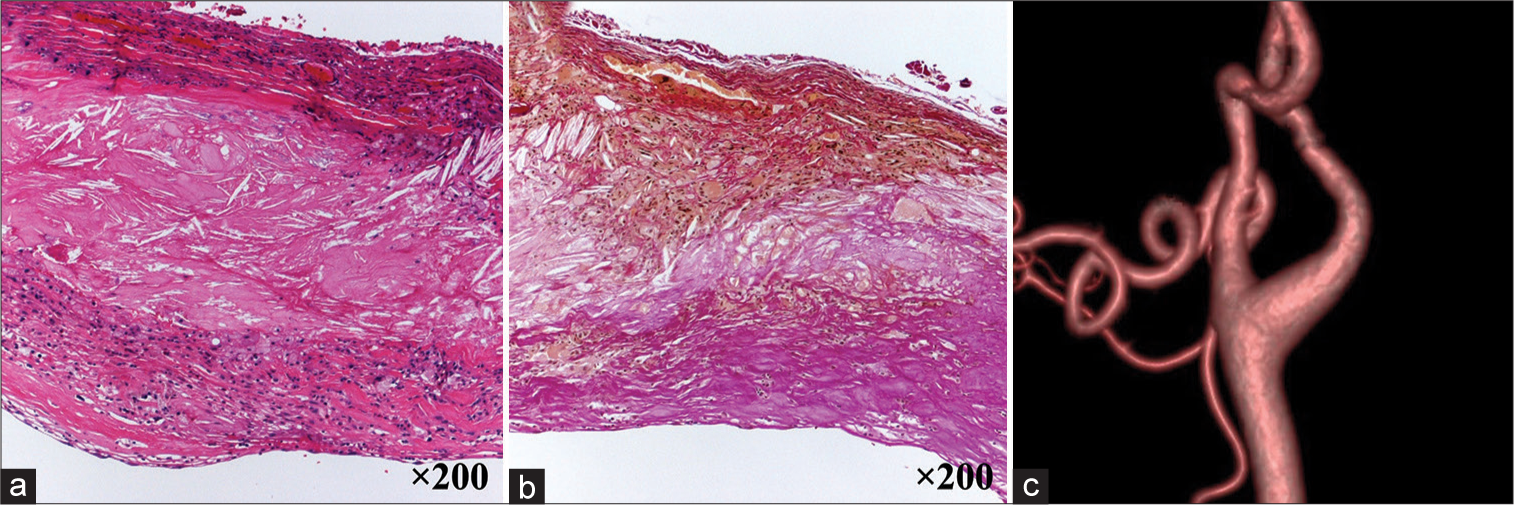
Figure 3:
Histopathological images showing the atherosclerotic aneurysm. The aneurysmal wall shows atheromatous changes with clusters of foamy cells and high cholesterol deposition (a). Elastica van Gieson staining showing the disappearance of elastic fibers in the internal elastic lamina and media (b). Postoperative computed tomography angiograph showing complete aneurysm removal and patency of the internal carotid artery (c).
DISCUSSION
Surgical treatment of cervical carotid artery aneurysms is rare, accounting for <0.2% of all cervical procedures.[
Although the exact rate of aneurysm rupture is unclear, surgical treatment should be considered to avoid rupture, thromboembolism, and mass effects, including lower cranial nerve palsy and discomfort. Several therapeutic options have been described for cervical aneurysms, including aneurysmectomy with or without reconstruction, proximal ligation, endovascular coiling, or stenting, and hybrid intervention.[
Previous reports have demonstrated that the endovascular procedure is an effective alternative for treating cervical aneurysms, with fewer procedure-related complications and shorter recovery times.[
There are two methods of ICA reconstruction: End-to-end and side-to-end anastomoses. No previous studies have compared these two methods in the human carotid artery. The two methods showed no significant differences in patency and complication rates in the rat carotid artery.[
CONCLUSION
Here, we presented a rare case of a giant saccular aneurysm of the cervical ICA. Despite the limitations, surgical aneurysmectomy and vessel anastomosis are recommended to prevent postoperative ischemic complications, even in the endovascular era.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmadi I, Herle P, Miller G, Hunter-Smith DJ, Leong J, Rozen WM. End-to-end versus end-to-side microvascular anastomosis: A meta-analysis of free flap outcomes. J Reconstr Microsurg. 2017. 33: 402-11
2. Attigah N, Külkens S, Zausig N, Hansmann J, Ringleb P, Hakimi M. Surgical therapy of extracranial carotid artery aneurysms: Long-term results over a 24-year period. Eur J Vasc Endovasc Surg. 2009. 37: 127-33
3. Blaisdell WF, Clauss RH, Galbraith JG, Imparato AM, Wylie EJ. Joint study of extracranial arterial occlusion. IV. A review of surgical considerations. JAMA. 1969. 209: 1889-95
4. Cunningham KS, Gotlieb AI. The role of shear stress in the pathogenesis of atherosclerosis. Lab Invest. 2005. 85: 9-23
5. Davidovic L, Koncar I, Dragas M, Ilic N, Banzic I, Pavlovic SU. Treatment strategies for carotid artery aneurysms. J Cardiovasc Surg (Torino). 2016. 57: 872-80
6. Dotson RJ, Bishop AT, Wood MB, Schroeder A. End-to-end versus end-to-side arterial anastomosis patency in microvascular surgery. Microsurgery. 1998. 18: 125-8
7. El-Sabrout R, Cooley DA. Extracranial carotid artery aneurysms: Texas Heart Institute experience. J Vasc Surg. 2000. 31: 702-12
8. Kankılıç N, Aydın MS, Göz M. Surgical repair of internal carotid artery aneurysm: Case report. Clin Med Insights Case Rep. 2021. 14: 1179547621991893
9. Khan NR, Shah A, Morcos JJ. Excision and end-to-end anastomosis of a giant partially thrombosed cervical internal carotid artery aneurysm mimicking a neck tumor: 2-dimensional operative video. Oper Neurosurg (Hagerstown). 2021. 20: E367-8
10. Liapis CD, Gugulakis A, Misiakos E, Verikokos C, Dousaitou B, Sechas M. Surgical treatment of extracranial carotid aneurysms. Int Angiol. 1994. 13: 290-5
11. Malikov S, Thomassin JM, Magnan PE, Keshelava G, Bartoli M, Branchereau A. Open surgical reconstruction of the internal carotid artery aneurysm at the base of the skull. J Vasc Surg. 2010. 51: 323-9
12. Ocal O, Yilmaz M, Peynircioglu B, Bilginer B, Peker A, Arat A. Hybrid vascular intervention for a giant cervical carotid artery aneurysm in a clopidogrel-hyporesponsive child. J Neurosurg Pediatr. 2018. 22: 265-9
13. Pulli R, Gatti M, Credi G, Narcetti S, Capaccioli L, Pratesi C. Extracranial carotid artery aneurysms. J Cardiovasc Surg (Torino). 1997. 38: 339-46
14. Rosset E, Albertini JN, Magnan PE, Ede B, Thomassin JM, Branchereau A. Surgical treatment of extracranial internal carotid artery aneurysms. J Vasc Surg. 2000. 31: 713-23
15. Shimizu T, Sakakura Y, Yamagiwa M, Hori M, Yuasa H, Murata M. Aneurysm of the extracranial carotid artery. Arch Otolaryngol Head Neck Surg. 1986. 112: 203-6
16. Welleweerd JC, den Ruijter HM, Nelissen BG, Bots ML, Kappelle LJ, Rinkel GJ. Management of extracranial carotid artery aneurysm. Eur J Vasc Endovasc Surg. 2015. 50: 141-7
17. Zhou W, Lin PH, Bush RL, Peden E, Guerrero MA, Terramani T. Carotid artery aneurysm: Evolution of management over two decades. J Vasc Surg. 2006. 43: 493-6